Full HTML
Lacrimal sac dacryolith treated with endoscopic dacryocystorhinostomy: A case report and literature review
Pankaj Goyal1, Chandrani Chatterjee2
Author Affiliation
1Consultant Surgeon, Department of ENT, Apollo ENT Hospital, Jodhpur, Rajasthan,
2Specialist, Department of ENT, All India Institute of Medical Sciences, AIIMS, Patna, Bihar, India.
Abstract
Dacryolith is a concretion within the nasolacrimal systemthat may calcify and cause further obstruction of the nasolacrimal pathway. It may cause intermittent epiphora without inflammation or recurrent dacryocystitis and is often diagnosed during dacryocystorhinostomy (DCR). We report the case of a lacrimal sac dacryolith in a 37-year-old man who was referred to our hospital from the eye clinic with complaints of epiphora that were not relieved by medication. He had no history of epiphora. During endoscopic DCR, the presence of dacryolith in the lacrimal sac was detected and completely removed while the pus was drained. The patient was discharged on the second postoperative day with systemic and topical antibiotics. During routine follow-up, the patient was in good condition and had no complaints. We aim to raise awareness among clinicians of this unusual cause of nasolacrimal duct obstruction, which can be successfully managed with endoscopic DCR rather than an open external approach.
DOI: 10.32677/yjm.v3i1.4402
Keywords: Dacryolith, Endoscopic dacryocystorhinostomy, Epiphora, Lacrimal sac, Nasolacrimal duct obstruction
Pages: 51-53
View: 6
Download: 10
DOI URL: https://doi.org/10.32677/yjm.v3i1.4402
Publish Date: 11-05-2024
Full Text
INTRODUCTION
Throughout the nasolacrimal system, dacryoliths are concretions that frequently consist of lipids, epithelial cells, and other detritus. Lacrimal calculus, also called ophthalmolith or dacryolith can form spontaneously or as a result of precipitation of calcium and phosphate salts on foreign material [1]. Intermittent epiphora without inflammation or recurrent dacryocystitis are signs and symptoms of dacryoliths (1). Dacryoliths may result in sporadic or continuous discomfort, as well as acute or chronic dacryocystitis (2). Patients with dacryolithiasis in the lacrimal sac often suffer from a history of lacrimal sac distention, long-term intermittent epiphora, and/or partial blockage of the nasolacrimal duct (NLD).
The frequency of dacryoliths in the lacrimal sac in patients undergoing DCR ranges from 6.0% to 18.0% [3-5]. The prevalence of dacryoliths in the population has not been studied. Most published studies of dacryolites have included a very modest number of samples [6–8]. Actinomycotic infection-related canalicular concretions have long been linked to canaliculitis.
The pathogenesis of lacrimal sac dacryoliths remains unclear despite substantial recent progress [1-3]. The process leading to dacryolith production has been proposed to be influenced by numerous predisposing variables. Age (less than 50 years), gender (females more frequently), smoking, history of chronic dacryocystitis and primary acquired nasolacrimal duct obstruction (PANDO) are some of these variables [3-5, 7, 9]. Some studies have shown that dacryolith formation may be associated with the expression of two peptide members of the trefoil factor (TFF) family, particularly TFF1 and TFF3, as well as the lacrimal sac epithelium and NLD synthesis of a variety of mucins [3, 10, 11].
Any abnormality anywhere throughout the drainage pathway, such as punctal diseases, canalicular deficits, aberrations in the lacrimal sac or duct, or intranasal pathology, can additionally have a role in the production of dacryoliths. Dehydration and denaturation of proteins in the lacrimal ducts are mostly caused by lacrimal sac diverticula, changes in the channel wall, flow, or fluid, chronic blockage and inflammation of the sac, and anomalies in the Hasner valve [2]. In patients with primary NLDO requiring dacryocystorhinostomy (DCR), dacryoliths are more commonly associated with male gender, presence of sac distension, partial NLDO, and smoking history [11]. In this report, we present a case of lacrimal sac dacryolith in a 37-year-old man who presented with complaints of epiphora which was not subsided with medications and treated successfully with endoscopic DCR.
CASE REPORT
A 37-year-old man came to our hospital complaining of sporadic, watery discharge from his left eye for over three months. The patient had no history of infection. No history of trauma, nasal congestion, cheek enlargement, diplopia, or visual impairment. Prior to his presentation, he was examined by an ophthalmologist who assured him that his eye was normal and prescribed oral and topical antibiotics and decongestants, after which his symptoms did not improve. The ophthalmologist proceeded to the sac syringing and concluded that there was regurgitation coming from the opposite punctum, so he referred the patient to us.
In our hospital, nasal endoscopy results were normal and we advised the patient to undergo endoscopic dacryocystorhinostomy (DCR). After receiving formal consent, the patient was scheduled for surgery Under general anesthesia. A curvilinear incision (6-8 mm anterior to the uncinate process) was made on the left side of the lateral wall of the nose after the operative site had been painted and draped. The anterior flap was raised. The maxillary frontonasal process was displayed. The bony protrusion was removed with a Kerrison Rongeur bone punch, exposing the lacrimal sac. A cut had been done over the sac area, and the pus was evacuated. The presence of dacryolith was discovered in the lacrimal sac (Figures 1 and 2). It was removed in its entirety (figure3 and 4).
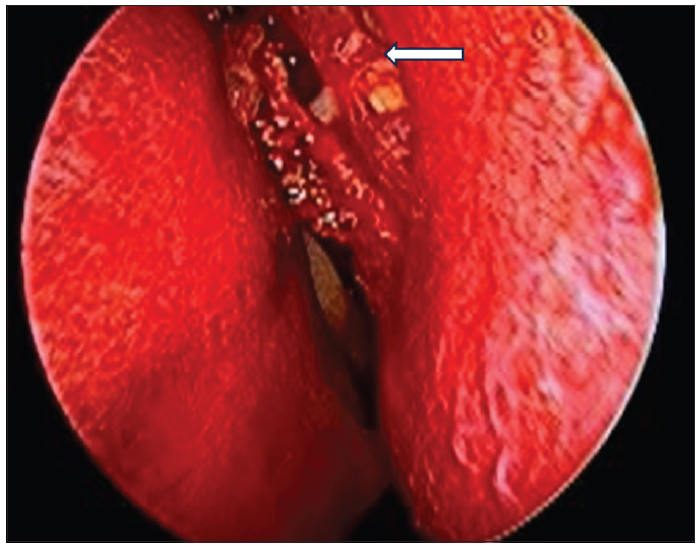 | 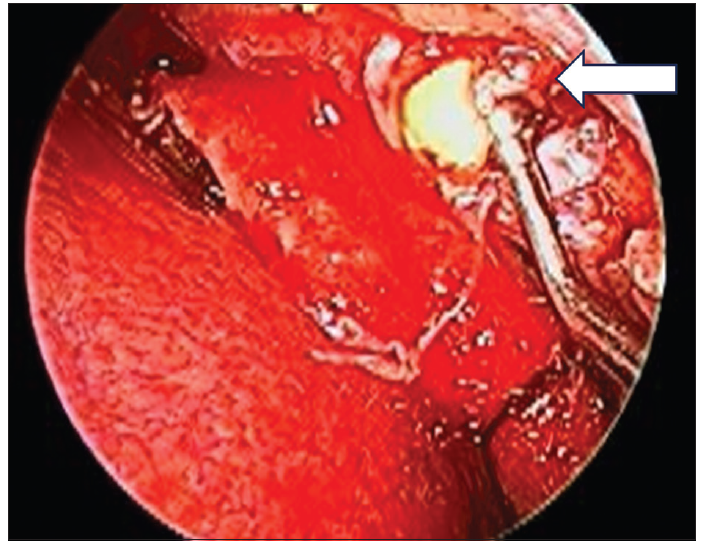 | 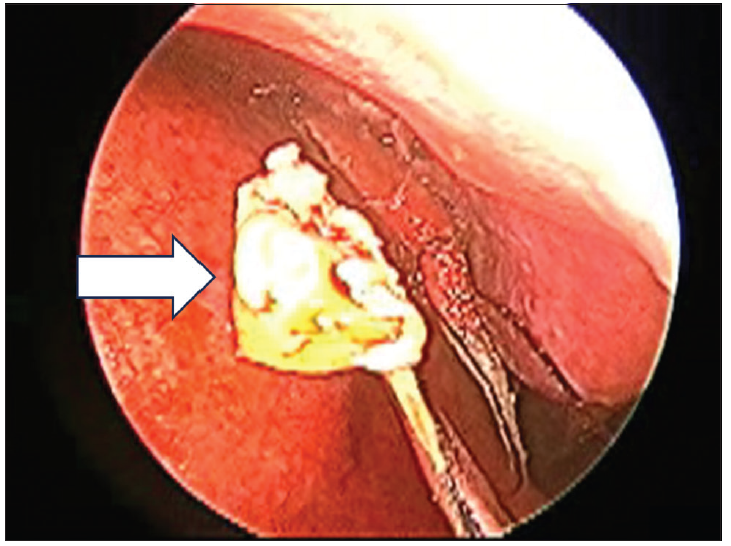 | 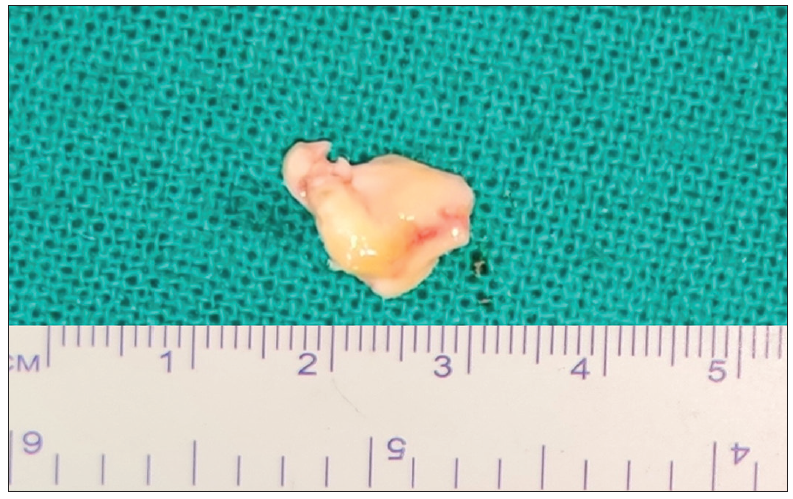 | ||
| Figure 1: Endoscopic view of left nasal cavity after exposing lacrimal sac | Figure 2: Endoscopic view of dacryolith after incising the lacrimal sac | Figure 3: Intraoperative picture showing dacryolith | Figure 4: Surgical specimen of dacryolith |
Following the excision of the dacryolith, sac syringing revealed an unrestricted flow of normal saline. Hemostasis was successfully completed, and the patient was extubated and sent to the recovery room. The patient was released on systemic and topical antibiotics on the second postoperative day. During routine follow-up, the patient was in good condition and had no complaints.
DISCUSSION
Cesoni reported dacryoliths or "calculi" of the lacrimal drainage system in 1670 [12], and they are routinely encountered by every lacrimal surgeon. Although dacryoliths have a lengthy history, our understanding of their pathogenesis is still in its infancy. The prevalence of dacryoliths in the general population is unknown. Relatively few dacryoliths were included in the majority of published investigations [4-6]. Of patients receiving EDCR, dacryoliths are seen in between 6.0 and 18.0% of instances [1, 2]. The most common cause of dacryolith development is primary acquired nasolacrimal duct obstruction (PANDO) [3-5, 10].
Despite the exact cause of the stones is unknown, there appeared to be an association between them and chronic dacryocystitis with stagnation caused by nasolacrimal stenosis. It is additionally difficult to identify which condition was more of a development driver—dacryolithiasis or chronic dacryocystitis [7, 13]. Morphological traits resembling fungi or structures resembling hyphae have been reported in some investigations [7, 14]. More study is required even though it appears that fungus could enhance the dacryolith creation process. Regretfully, there isn't much pertinent information about the culture of lacrimal sac stones in the literature. On the other hand, other writers think that in certain cases, dacryolith development requires explanations other than simple blockage.
The observation that the nasolacrimal duct is not necessarily narrow on dacryocystogram in patients with dacryoliths lends credence to this claim [15].
A higher prevalence of acute dacryocystitis with dacryoliths has been shown by some earlier studies (12,9); however, probably, these investigations did not distinguish between acute dacryocystitis and lacrimal sac distention (retention). In fact, while acknowledging the distinction in clinical presentation between acute dacryocystic retention and the more traditional infectious dacryocystitis, some publications have referred to this condition as "non-infectious dacryocystitis." [16]
All patients who have a suspected foreign body, or lacrimal sac dacryolith, should be managed as a nonoperative case, according to Jones and Wobig [17]. This means that massage, lacrimal irrigation, and probing should be used until the patient's symptoms have subsided. For acute dacryocystic retention, Smith et al.'s nonsurgical treatment was shown to be successful [18] .They recommended percutaneous aspiration of the lacrimal sac contents prior to irrigation and probing. Angiographic approaches have been reported for percutaneous nasolacrimal duct probing as a therapeutic modality. (15)
In our experience, conservative treatment is recommended for patients who experience occasional episodes or whose symptoms resolve on their own, particularly if testing reveals just partial nasolacrimal duct occlusion. We recommend an endoscopic DCR, which will typically give symptomatic relief of epiphora and pain, if the situation worsens to total blockage or if the symptomatic episodes increase in frequency. (14,19,21)
The limitation of dacryocystogram and computed tomography is that while these imaging modalities can identify a "mass" inside the lacrimal sac, conclusive characterization might not be achievable. Surgical planning could be impacted in patients with clinical characteristics that point to a dacryolith, who have not improved with conservative care, and who need a DCR. While some writers feel that endoscopic DCR is not affected by the presence of a dacryolith, others argue that it may make the procedure more challenging or even potentially contraindicated. (21) If a dacryolith is detected preoperatively, surgical planning can be changed accordingly, depending on the particular lacrimal surgeon's competence and experience. If DCR is performed endoscopically or via an external method, a wider hole for lacrimal sac exploration is usually required. The absence of a facial scar, the intact lacrimal pump system, and the ability to simultaneously treat co-occurring nasal disorders are some of the reasons why endoscopic DCR is preferable to the external approach.
CONCLUSION
This is an illness that is diagnosable and treatable in an acute condition. Our instances demonstrate that putty-like casts, called dacryoliths, that originate in the nasolacrimal system can lead to sporadic epiphora. Using the sac syringing test, dacryoliths in the lacrimal sac must be clinically evaluated and considered as a possible cause of intermittent epiphora. Even when used in an acute setting, endoscopic DCR is a safe technique with good outcomes.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient for publication of this case report and all accompanying images.
AUTHORS’ CONTRIBUTIONS
All authors contributed to the completion of this work. The final manuscript was read and approved by all authors
References
- Aydin U, Hastar E, Yildirim D. Dacryolith: two case reports. Dentomaxillofac Radiol. 2007; 36(4):237-9.
- Rosen WJ, Rose GE. Intranasal passage of dacryoliths Br J Ophthalmol. 2000;84(7):799-800.
- Paulsen F. Pathophysiological aspects of PANDO, dacryolithiasis, dry eye, and punctum plugs. In: Weber RK, Keerl R, Schaefer SD et al Atlas of lacrimal surgery. Springer, Berlin, 2007, p 15–27
- Repp DJ, Burkat CN, LucarelliMJ. Lacrimal excretory system concretions: canalicular and lacrimal sac. Ophthalmology. 2009;116:2230– 2235
- Hurwitz JJ. Diseases of the Sac and Duct. In: Hurwitz JJ (ed) The lacrimal system, 1st edn. Lippincott Raven, Philadelphia, 1996, p 117–138
- Iliadelis ED, Karabatakis VE, Sofoniou MK. Dacryoliths in a series of dacryocystorhinostomies: histologic and chemical analysis. Eur J Ophthalmol. 2006; 16(5):657–662
- Orhan M, Onerci M, Dayanir V et al. Lacrimal sac dacryolith: a study with atomic absorption spectrophotometry and scanning electron microscopy. Eur J Ophthalmol. 1996;6(4):478–480
- Iliadelis E, Karabatakis V, SofoniouM. Dacryoliths in chronic dacryocystitis and their composition (spectrophotometric analysis). Eur J Ophthalmol. 1999;9(4):266–268
- Herzig S, Hurwitz JJ. Lacrimal sac calculi. Can J Ophthalmol.1979; 14(1):17–20
- Paulsen FP, Schaudig U, Fabian A, et al. TFF peptides and mucins are major components of dacryoliths. Graefes Arch Clin Exp Ophthalmol 2006;244(9):1160–1170
- Yazici B, Hammad AM, Meyer DR. Lacrimal sac dacryoliths: predictive factors and clinical characteristics. Ophthalmology. 2001 Jul;108(7):1308-12.
- Duke-Elder S, ed. Textbook of Ophthalmology. Vol. 5: The Ocular Adnexa. London: Kimpton, 1952;5364.
- Viers ER. Lacrimal disorders. CV Mosby, St. Louis, 1976, p 150–180
- Berlin AJ, Rath T, Rich L. Lacrimal system dacryoliths. Ophthalmic Surg 1980;11(7):435–6
- Gonnering RS, Bosniak SL. Recognition and management of acute noninfectious dacryocystic retention. Ophthal Plast Reconstr Surg 1989;5:27–33.
- Hurwitz JJ, ed. The Lacrimal System. Philadelphia: Lippincott- Raven, 1996:117–38.
- Jones LT, Wobig JL, eds. Surgery of the Eyelids and Lacrimal System. Birmingham, AL: Aesculapius Publishing Co, 1976: 185–93.
- Smith B, Tenzel RR, Buffam FV et al. Acute dacryocystic retention [case report]. Arch Ophthalmol 1976; 94:1903– 4.
- Jones LT. Tear-sac foreign bodies. Am J Ophthalmol 1965; 60:111–3.
- Wilkins RB, Pressly JP. Diagnosis and incidence of lacrimal calculi. Ophthalmic Surg 1980; 11:787–9.
- Berlin AJ. Success rate of endoscopic laser-assisted dacryocystorhinostomy [letter]. Ophthalmology 2000; 107:4 –5.
