Full HTML
Epidemiology of cardiovascular diseases related admissions in a tertiary hospital in Hadramout Governorate, Yemen
Jamal M Basamed1, Abdul Raheem Bahishwan1, Musaab Fahmi Yousef2
Author Affiliation
1Consultant, Department of Medicine, Hadhramout Modern Hospital, Al Mukalla, Yemen,
2Medical Student, Department of Medicine, University of Jordan, School of Medicine, Amman, Jordan
Abstract
Background: Cardiovascular diseases (CVDs) are a major challenge confronting physicians in Hadramout Governorate. Little is known about the admission for CVD and outcome at Hadramout Modern Hospital. The aim of this study was to determine the frequency and pattern of CVD admissions in Hadramout Modern Hospital, Hadramout, Yemen. Materials and Methods: This retrospective cross-sectional study included all adult patients admitted for CVDs in the medical ward of Hadramout Modern Hospital from January 01 to December 31, 2023. Results: During the study period, a total of 1020 patients were admitted to the medical word, of which 158 (15.5%) cases were admitted with CVDs. There were 87 (55.1%) males, and the mean age was 58.09±15.08 years. There was a significant age difference between men and women (61.4 years vs. 54.04 years, p=0.002). The most commonly affected age group was those aged 55–64 (32.4%). Uncontrolled hypertension (81.6%), stroke (52.5%), heart failure (37.3%), and acute myocardial infarction (AMI) (36.1%) were the most common CVDs. The mean hospital stay was 7.93±2.83 (2–15 days). There were 220 total deaths in Hadramout Modern Hospital during the study period. Among them, 12 (5.5%) were due to CVDs with no significant sex difference (4 [5.6%] vs. 8 [9.2%]; p=0.549). Conclusion: Given the increasing burden of CVDs in our hospital, it is crucial to understand the epidemiological features of CVDs and their etiological factors to prioritize further research, prevention, and treatment strategies. Additionally, further research is needed in other governorates across the country to identify regions with the highest regional burden of CVDs so that policymakers can reallocate limited resources accordingly.
DOI: 10.32677/yjm.v3i1.4579
Keywords: Arrhythmias, Cardiovascular diseases, Hadramout, Heart failure, Hypertension, StrokeCorrespondence to: Dr. Jamal M Basamed, Department of Medicine, Hadhramout Modern Hospital, Al Mukalla, Yemen, E-mail: jamal.basamed20@gmail.com© 2024 Creative Commons Attribution-NonCommercial 4.0 International License (CC BY-NC-ND 4.0).Original ArticleAccess this article onlineReceived - 04 April 2024 Initial Review - 08 April 2024 Accepted - 19 April 2024Quick Response codeDOI: 10.32677/yjm.v3i1.4579
Pages: 25-29
View: 9
Download: 13
DOI URL: https://doi.org/10.32677/yjm.v3i1.4579
Publish Date: 11-05-2024
Full Text
INTRODUCTION
Cardiovascular diseases (CVDs) are a group of disorders of the heart and blood vessels, including coronary artery disease, cerebrovascular disease, rheumatic heart disease, and other conditions. CVDs are the leading cause of death worldwide, with above 70% in low- and middle-income nations [1]. To reduce the burden of CVDs on the health system and minimize the resources spent to combat CVDs and their social and economic consequences worldwide, it is crucial to understand the epidemiological characteristics of CVDs and their etiological factors in order to prioritize research, prevention, and treatment strategies. Although some risk factors, such as age, ethnicity, and sex, obviously cannot be modified, most of the risk factors are attributable to lifestyle and behavioral patterns, which can be changed. In developed countries, CVDs are well studied and there are well-defined policies in this regard [2-4]. Over 80% of the global burden of CVD is borne by low- and middle-income countries (LMICs), and it is believed that by 2030, CVDs and non-communicable diseases will be the dominant conditions in these countries [5-7]. However, CVDs still represent a challenge for health policymakers in LMICs due to the lack of data on the burden of CVDs in these countries (including Yemen) [8,9]. The lack of data on the burden of CVDs in Yemen results from a lack of research caused by the civil war, a lack of local expertise, and poor funding [10]. This study aimed to determine the frequency and pattern of CVDs in patients admitted to Hadramout Modern Hospital, Hadramout Governorate, Yemen.
MATERIALS AND METHODS
Study Design, Setting, and Population
A retrospective cross-sectional study was conducted from January 01, 2023 to December 31, 2023 in Hadramout Modern Hospital, Mukalla, Hadramout, Republic of Yemen. All patients admitted to the study with CVDs during the study period were included in this study. Hadramout Modern Hospital is a private referral center in Mukalla city, where students of medical and health institutes receive their training. It is a tertiary hospital serving approximately 1,000,000 people. The hospital covers all specialties, including an intensive care unit.
Inclusion and Exclusion Criteria
All patients suffering from various CVDs aged 18 years or older were included in this study; however, patients aged <18 or those with an unclear diagnosis of CVD or incomplete data were excluded.
Sample Size and Sampling Technique
All consecutive patients diagnosed with CVDs during the study period were included (complete enumeration) by adopting a purposive sampling technique.
Data Collection
Cases of CVD were identified by the medical records department. We then retrospectively reviewed the patients’ medical records and retrieved detailed data, including age, age groups, sex, a final diagnosis of CVD, length of hospital stay, and outcome. In this study, the diagnoses of CVDs were derived from medical records and depended solely on the treating physician.
Data Analysis
Data were reported as means±standard deviation for quantitative variables, while qualitative variables were described as numbers and percentages. Astudent t-test was used for continuous variables and a Mann–Whitney U-test if quantitative variables were not normally distributed. Pearson’s Chi-square tests or Fisher’s test, when appropriate, were used to test the differences in the proportion of categorical variables. The level of significance was established as p<0.05. Data analysis was performed with SPSS software (version 23; IBM Corp., Armonk, NY, USA).
Ethical Approval
Currently, there is no research committee in our governorate; therefore, permission to conduct the study was obtained from the hospital’s administrative office.
RESULTS
Demographic characteristics of the participants
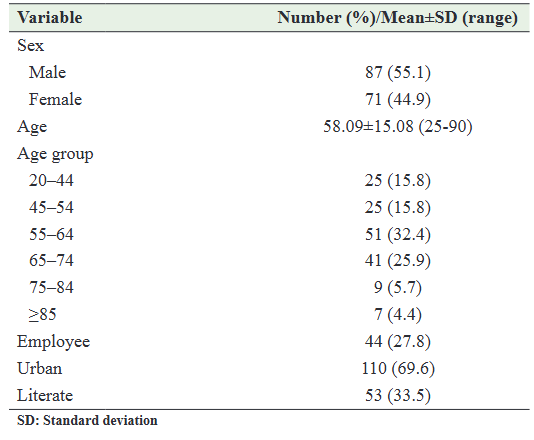
During the study period from January 01, 2023 to December 31, 2023, a total of 5624 patients were admitted to Hadramout Modern Hospital, of which 1020 were admitted to the medical ward. The number of patients admitted for CVDs during the same period was 158, representing 2.8% of all hospital admissions and 15.5% of patients admitted to the medical ward. Men were slightly more represented at 87 (55.1%), with no statistical significance (p=0.0718). The mean age was 58.09±15.08 years. There was a significant age difference between men and women (61.4 years vs. 54.04 years, p=0.002). The most commonly affected age group (32.4%) was those aged between 55 and 64 years. Table 1 describes the demographic characteristics of the participants.
Table 1: Demographic characteristics of the participants
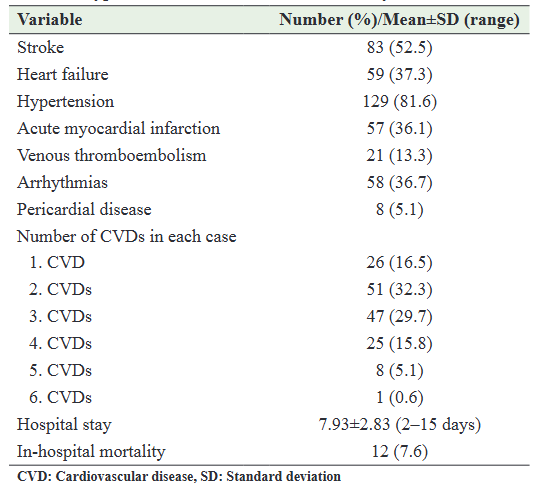
Types of CVDs, Hospitalization Duration, and In-Hospital Mortality
Table 2 summarizes the types of CVDs among the patients involved in this study. The most common CVDs were uncontrolled hypertension (81.6%), stroke (52.5%), heart failure (37.3%), and AMI (36.1%). Most patients 132 (83.5%) had more than one CVD, while 26 (16.5%) patients had only one CVD (Table 2). The mean length of hospitalization was 7.93±2.83 (range: 2–15 days). There were 220 total deaths in Hadramout Modern Hospital during the study period. Among them, 12 (5.5%) were due to CVDs with no significant sex difference (4 [5.6%] vs. 8 [9.2%]; p=0.549).
Table 2: Type and outcome of CVDs in our study
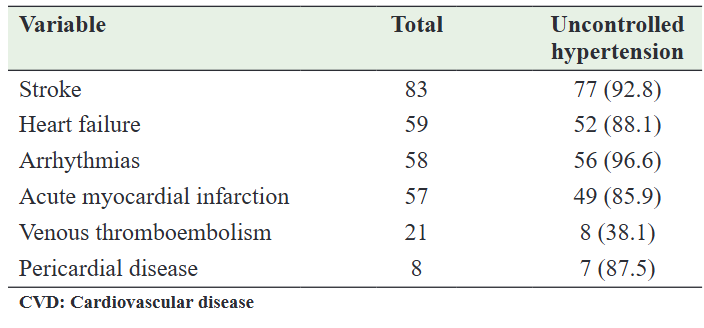
Types of CVDs Stratified by Age Group, Sex, and Uncontrolled Hypertension
When age groups were stratified by CVDs, including stroke, heart failure, hypertension, myocardial infarction, pericardial disease, and cardiac arrhythmias, the age group 55–64 years old was most commonly affected (Table 3). The stratification of CVDs by sex showed that patients with stroke had a significant male predominance, while no significant sex difference was found in other types of CVDs (Table 4). Stratification of hypertension according to types of CVD showed that it constitutes the common risk factor for almost all types of CVDs involved in this study (Table 5).
Table 3: The distribution of CVDs according to the age group
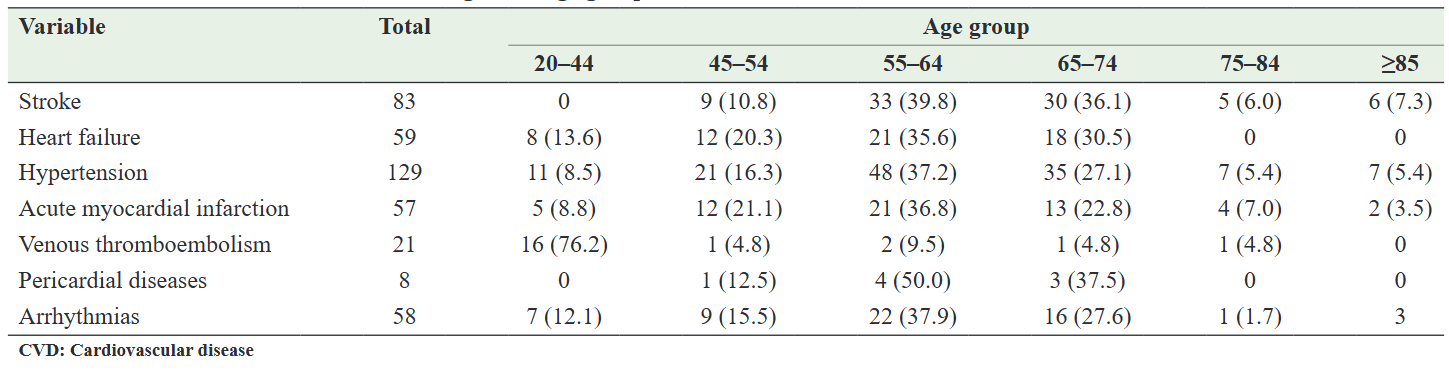
Table 4: The distribution of CVDs according to the sex
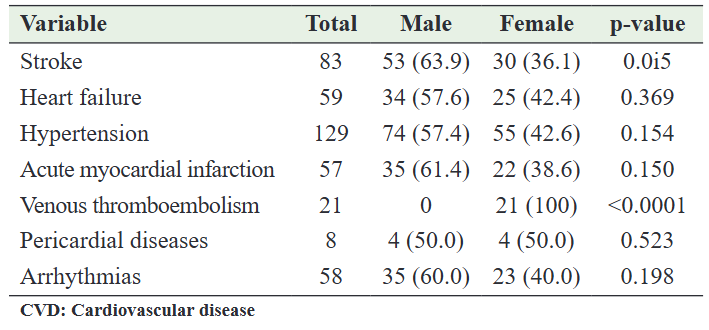
Table 5: Distribution of hypertension among various CVDs in this study
DISCUSSION
CVDs are a group of illnesses that mostly affect the heart and blood vessels accounting for the major causes of death and disability worldwide, particularly in low- and middle-income nations [1,5,6,11]. Therefore, CVDs remain a significant public health concern globally. An epidemiological transition from communicable to non-communicable diseases is observed worldwide, as evidenced by the evolution of publication topics over time. The theoretical framework underlying epidemiological transitions is that the health status and disease spectrum characteristics of different countries are related to their socioeconomic environment.
In Yemen, it is difficult to determine the period of epidemiological transition due to a lack of publications. Recently, few publications from Yemen have been found in the literature; however, to our knowledge, our study is the first that describes the CVDs’ epidemiology in a region in Yemen, where medical research is still in its infancy. This situation most likely resulted from civil war, poverty, a lack of resources, a lack of access to literature, and a lack of knowledge about the basics of medical research practice [10]. Therefore, efforts to advance research and create a cadre of CVD research leaders are essential. We found that CVDs accounted for 15.5% of medical ward admissions, which is comparable to a hospital‐based study conducted in Cameroon (15.9%) [12] but less than another study conducted in Nigeria (20.8%) [13] and higher than the 8.2% from the Ghanaian study [14]. This frequency variation in CVDs is not precise and does not reflect the real burden of the diseases in the regions under study because it is most likely influenced by the ease of access to health-care facilities in each country. The slight male preponderance observed in our study is similar to studies from Nigeria and Ghana [13,14].
The mean age in our study was 58.09 years, which is comparable to that reported in Cameroon [12], but higher than that reported by other authors in Rwanda and Nigeria [15,16]. The majority of the patients admitted for CVDs in our study were between 55 and 64 years old (Table 1), which is similar to that reported in Cameroon (50–69 years old) [12].
Interestingly, we found that most patients were admitted with more than one CVD (Table 2), with uncontrolled hypertension being the most frequently encountered CVD in this study. The stratification of hypertension according to types of CVDs showed that it constitutes the common risk factor for almost all types of CVDs involved in this study (Table 5), in agreement with numerous hospital-based studies worldwide [12-17]. Delay in treating hypertension leads to complications and, consequent, high mortality. Therefore, early detection and treatment of hypertension are crucial to reducing the burden of CVDs in any society. As mentioned earlier, the characteristics of each country’s health status and disease spectrum are linked to its socioeconomic environment. We therefore believe that the level of psychological stress caused by poverty and instability attributed to the civil war is likely closely related to the prevalence of hypertension in our study, while poor blood pressure management in our patients was most likely attributed to non-compliance with treatment due to the high cost of drugs or their unavailability [18]. Noticeably, uncontrolled hypertension was discovered incidentally in many patients who were admitted for other CVDs. If hypertension is not considered a cause for admission in most cases, stroke would be the most common CVD requiring admission to the medical ward in our study, accounting for 52, 5% of total admissions for CVDs, consistent with some studies from Nigeria [13,19]. In previous studies in Yemen, hypertension was the most common risk factor for stroke [18,20]. Heart failure was the second most common cause of admission accounting for 37.3% of CVD admissions in medical wards, consistent with the findings from Nigeria (36.2%) [13]. The majority of heart failure cases in our study were as a result of hypertension (88.1%). The large number of patients admitted for heart failure most likely experienced delays in treatment due to a lack of early access to health-care facilities or a lack of knowledge about risk factors and early symptoms of heart failure. Myocardial infarction ranked third in the list of causes of admission, which accounted for 36.1% of CVD admissions. Interestingly, most patients with venous thromboembolism (VTE) in our study 16 (76.2%) were aged 20–44 years and were all women (Table 4). To reduce the burden of CVD within this age group and to reduce morbidity such as post-thrombotic disease and chronic thromboembolic pulmonary hypertension [21], knowledge of VTE risk factors is crucial for prioritizing treatment strategies, research, prevention, and treatment.
The present study had certain limitations. First, the retrospective design, hospital-based setting, and study samples may reflect a potential methodological drawback considering generalizability to a particular population. Second, there were no clear diagnostic criteria for CVDs in the study, and the diagnosis was made based on the documents. Third, for technical reasons, we did not consider CVD risk factors. However, we are planning to include the risk factors in the coming studies. Despite these limitations, this is perhaps the first-ever study conducted in Yemen to explore the frequency and types of CVDs among patients in Hadramout Governorate. We believe that our findings will enrich the existing literature in the relevant field, particularly the baseline data on the frequency and types of CVDs in our population, which will consequently assist policymakers in developing preventive interventions in primary care practice aimed at reducing the burden of disease in the early stages and reducing pre-mature deaths due to CVDs.
CONCLUSION
Our study showed that CVDs accounted for 15.5% of medical ward admissions and that the 55–64-year age group was most commonly affected. Stroke was the most common cause of hospital admission, while hypertension was the most common risk factor. Deaths attributed to CVDs accounted for 5.5% of all deaths in our hospital. Given the increasing burden of CVDs in our hospital, it is crucial to understand the epidemiological features of CVDs and their etiological factors to prioritize further research, prevention, and treatment strategies. Additionally, further research is needed in other governorates across the country to identify regions with the highest regional burden of CVDs so that policymakers can reallocate limited resources accordingly.
References
1. Keates AK, Mocumbi AO, Ntsekhe M, et al. Cardiovascular disease in Africa: Epidemiological profile and challenges. Nat Rev Cardiol 2017;14:273-93.
2. Mensah GA, Wei GS, Sorlie PD, et al. Decline in cardiovascular mortality: Possible causes and implications. Circ Res 2017;120:366-80.
3. Tunstall-Pedoe H, Vanuzzo D, Hobbs M, et al. Estimation of contribution of changes in coronary care to improving survival, event rates, and coronary heart disease mortality across the WHO MONICA project populations. Lancet 2000;355:688-700.
4. Amadi CE, Lawal F, Ajiboye W, et al. Opportunistic screening of cardiovascular disease risk factors in community pharmacies in Nigeria: A cross-sectional study. Int J Clin Pharm 2020;42:1469-79.
5. Lopez AD, Mathers CD, Ezzati M, et al. Global and regional burden of disease and risk factors, 2001: Systematic analysis of population health data. Lancet 2006;367:1747-57.
6. Bygbjerg IC. Double burden of noncommunicable and infectious diseases in developing countries. Science 2012;337:1499-501.
7. Alwan A, Maclean DR. A review of non-communicable disease in low- and middle-income countries. Int Health 2009;1:3-9.
8. Zhao D. Epidemiological features of cardiovascular disease in Asia. JACC Asia 2021;1:1-13.
9. Pullar TJ, Allen J, Townsend N, et al. The impact of poverty reduction and development interventions on non-communicable diseases and their behavioural risk factors in low and lower-middle income countries: A systematic review. PLoS One 2018;13:e0193378.
10. Al-Shoaibi I, Abdo BA, Abdullah MA. Attitudes, knowledge, and obstacles regarding medical research among medical students at the faculty of medicine and health sciences, Ibb University, Ibb, Yemen. Yemen J Med 2022;1:89-92.
11. Roth GA, Mensah GA, Johnson CO, et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: Update from the GBD 2019 study. J Am Coll Cardiol 2020;76:2982-3021.
12. Nkoke C, Jingi AM, Makoge C, et al. Epidemiology of cardiovascular diseases related admissions in a referral hospital in the South West region of Cameroon: A cross-sectional study in sub-Saharan Africa. PLoS One 2019;14:e0226644.
13. Amadi CE, Mbakwem AC, Ajuluchukwu JN, et al. Trends and outcomes of cardiovascular disease admissions in Lagos, Nigeria: A 16-year review. Cardiovasc J Afr 2023;34:140-8.
14. Appiah LT, Sarfo FS, Agyemang C, et al. Current trends in admissions and outcomes of cardiac diseases in Ghana. Clin Cardiol 2017;40:783-8.
15. Amendezo E, Twagirumukiza M, Sebantunzi O, et al. Inhospital cardiovascular morbidity and mortality in the department of internal medicine at CHU Kigali (Rwanda). Ann Trop Med Public Health 2008;1:9-14.
16. Ansa VO, Ekott JU, Bassey EO. Profile and outcome of cardiovascular admissions at the University of Uyo Teaching Hospital, Uyo--a five year review. Niger J Clin Pract 2008;11:22-4.
17. Naliganti C, Valupadas C, Akkinepally RR. Prevalence of cardiovascular diseases in a tertiary care teaching hospital. Int J Pharm Pract 2016;9:214-8.
18. Basamed JM. Risk factors and outcomes of stroke in a tertiary hospital in Hadhramout Governorate, Yemen. Yemen J Med 2022;1:69-73.
19. Hadiza S. Cardiovascular disease admissions in medical wards of a tertiary hospital in North-western Nigeria. IOSR J Dent Med Sci 2018;17:47-50.
20. Hezam HS, Khan FY. Clinical presentation, risk factors, and outcomes of stroke in Shabwah Governorate, Yemen. Yemen J Med 2023;2:151-6.
21. Lacruz B, Tiberio G, Latorre A, et al. Venous thromboembolism in young adults: Findings from the RIETE registry. Eur J Intern Med 2019;63:27-33.
