Full HTML
Percutaneous cholecystostomy in acute cholecystitis – Narrative review article
Kumar Hari Rajah
Author Affiliation
Associate Professor of Surgery, Department of Surgery, Taylor’s University School of Medicine, and Health Science, Selangor, Malaysia
Abstract
Percutaneous cholecystostomy is often performed to treat high-risk patients with acute cholecystitis who are not suitable for cholecystectomy. It is performed by the interventional radiologist and can be performed through the transhepatic or transperitoneal route (direct gallbladder puncture, without passing through the liver). Percutaneous cholecystostomy is used as a bridging procedure to stabilize high-risk patients with acute cholecystitis. We prepared this narrative review article to describe the indications for performing this procedure and the consequences of its performance and to compare it with emergency cholecystectomy
DOI: 10.32677/yjm.v3i1.4406
Keywords: Acute cholecystitis, Cholecystectomy, Conservative treatment of acute cholecystitis, Non-operative treatment of acutecholecystitis, Percutaneous cholecystostomy
Pages: 21-24
View: 7
Download: 10
DOI URL: https://doi.org/10.32677/yjm.v3i1.4406
Publish Date: 11-05-2024
Full Text
Acute cholecystitis is a clinical condition most commonly caused by gallstones and is associated with symptoms of upper abdominal pain, nausea, and vomiting. Cholecystectomy is the treatment of choice for acute cholecystitis but for patients with high-risk factors such as increasing age, medical conditions such as heart disease, hypertension, and diabetes mellitus who are not candidates for surgery, percutaneous cholecystostomy can be used as a bridge to manage this condition [1-4]. Fig. 1, describes the flow chart of the management of acute cholecystitis. The World Society of Emergency Surgery guidelines for the diagnosis and management of acute calculous cholecystitis have recommended percutaneous drainage of the gallbladder in patients who are not fit for surgery. It is a safe and effective treatment option for elderly and high-risk patients. Delayed cholecystectomy should be offered for patients who have recovered and to reduce their perioperative risk factors [5,6]. The Tokyo Guidelines for the Diagnostic Criteria and Severity Grading of Acute Cholecystitis state that grade 3 acute cholecystitis of TG13 severity is associated with multiorgan failure and should be treated in the intensive care unit. Percutaneous cholecystostomy is often used in these patients because they are not suitable for cholecystectomy [7]. Percutaneous cholecystostomy involves the introduction of a catheter into the gallbladder which can be done through ultrasound or computerized tomography. This procedure can be done by a transhepatic or transperitoneal route. The procedure is associated with minimal risk and complication rates. It is a safe procedure to perform in elderly patients with acute biliary sepsis [8,9].
We have conducted this review article to describe the indications for percutaneous cholecystostomy, the time for removal of the tube, the complications of the procedure, and the comparison of this procedure with emergency cholecystitis. We conducted a literature search using PubMed, the Cochrane database of clinical reviews, Google Scholar, and Semantic Scholar, searching for randomized control trials, systemic reviews, meta-analyses, and observational and cohort studies from 1990 to 2023. All selected articles were available in full text. The following keywords were used “Percutaneous cholecystostomy,” “acute cholecystitis,” “conservative treatment of acute cholecystitis,” “cholecystectomy,” and “non-operative treatment of acute cholecystitis.” All articles were written in English and pediatric and pregnant patients were excluded from this review. Case reports and comments were excluded.
INDICATIONS FOR PERCUTANEOUS CHOLECYSTOSTOMY
Percutaneous cholecystostomy is performed in elderly patients with co-morbidities who present with acute cholecystitis. It was initially performed in patients who were not fit for surgery and who were hemodynamically unstable. These patients were often above the age of 70 and had an American Society of Anesthesia score of more than 2 and those that were septic. It is used as a bridging procedure to stabilize the patient and perform a cholecystectomy later [10-15]. Percutaneous cholecystostomy can be performed by the transhepatic route of the transabdominal route. The procedure is performed by the radiologist with an ultrasound approach. The transhepatic route is more common and easier to perform. The incidence of catheter dislodgement is also much less when compared to the trans-abdominal route. It was also associated with a reduced risk of biliary peritonitis [16-19]. When early percutaneous cholecystostomy is performed within 24 h of presentation of symptoms of acute cholecystitis is associated with reduced morbidity and duration of hospital stay. This highlights the importance of early diagnosis and treatment of this condition [20,21]. The incidence of recurrence of acute cholecystitis after percutaneous cholecystostomy has been reported to be 20% and only one-third of patients undergo a cholecystectomy due to their underlying medical problems and risk factors for anesthesia. It is often associated with repeated admissions to the hospital [22]. Percutaneous cholecystostomy can be performed as a definitive procedure in up to one-third of elderly patients who are present with acute cholecystitis. It is a convenient and effective procedure that is associated with low complication rates. Once the procedure is performed the catheter is kept for at least 3 weeks. Due to the high anesthetic risk to older patients, this procedure often becomes the definitive treatment option [23-26]. The use of percutaneous cholecystostomy in the management of mild-to-moderate acute cholecystitis was performed by selected retrospective studies but the recurrence rates and readmission rates were high, and it failed to demonstrate any long-term clinical benefit [27-29]. A cholecystogram should be performed in all patients who have a percutaneous cholecystostomy to look for obstruction at the cystic duct or the presence of incidental common bile duct stones. This will help in deciding whether these patients may require an endoscopic retrograde cholangiopancreatography or imaging like a magnetic resonance cholangiopancreatography [30]. Percutaneous cholecystostomy is often associated with longer stays in the hospital and increased pain over the tube site. It is also associated with recurrent admissions for cholecystitis. The management of the cholecystostomy tube is a problem with a risk of tube dislodgement and subsequent bile peritonitis [31,32]. Some factors that affect recurrence after placement of a percutaneous cholecystostomy tube include patients who present with severe cholecystitis, leukocytosis, and prolonged duration of tube placement [28,33]. A nationwide study comparing the long-term outcomes of percutaneous cholecystostomy to cholecystectomy by Anderson et al. included patients who were followed up over 12 years. This study concluded that percutaneous cholecystostomy was associated with reduced complications when compared with patients who underwent cholecystectomy, but it was associated with prolonged hospital stays and increased cost [34].
CONSEQUENCES OF PERCUTANEOUS CHOLECYSTOSTOMY
The duration of placement of the percutaneous cholecystostomy tube with depend on the co-morbidities of the patient as a retrospective study by Boules et al. showed that 32.9% of patients who underwent percutaneous cholecystostomy subsequently underwent cholecystectomy. Tube placement may be longer in old and frail patients. A retrospective study by Bundy et al. looking at the long-term outcomes of percutaneous cholecystostomy showed that only 29.6% of patients underwent cholecystectomy but percutaneous cholecystostomy was successful in all the patients who underwent the procedure [35,36]. Prolonged placement of the percutaneous cholecystostomy catheter is associated with increased morbidity and hospital stay. The average duration of keeping the tube includes 4–6 weeks when the acute cholecystitis is controlled. Removal of the catheter should be performed after 21 days. Factors that favor successful percutaneous drainage and subsequent cholecystectomy include younger patients and reduced anesthetic risk [37-40]. In patients with severe acute cholecystitis with co-morbidities and are not fit for cholecystectomy, the percutaneous cholecystostomy tube often becomes a definitive treatment as it is associated with low risk [41].
PERCUTANEOUS CHOLECYSTOSTOMY VERSUS CHOLECYSTECTOMY IN HIGH-RISK PATIENTS
A systemic review and meta-analysis by Huang et al. on percutaneous cholecystostomy versus emergency cholecystectomy in the treatment of acute cholecystitis in high-risk patients found that percutaneous cholecystostomy was associated with increased morbidity, mortality, length of hospital stay, and cost when compared with cholecystectomy. They concluded that emergency cholecystectomy is superior to percutaneous cholecystostomy. These findings were also confirmed by systemic reviews and meta-analyses that were conducted by Cirocchi et al. and Markopoulos et al. who compared emergency cholecystectomy against percutaneous cholecystostomy in the management of acute cholecystitis in high-risk patients [42-44]. The laparoscopic cholecystectomy versus percutaneous catheter drainage for acute cholecystitis (CHOCOLATE) multicenter randomized clinical trial where 142 high-risk acute cholecystitis patients were randomized to 66 who underwent emergency cholecystectomy and 68 who underwent percutaneous cholecystectomy. The results of this trial showed that the percutaneous cholecystostomy group was associated with increased morbidity, recurrence rate, and prolonged hospitalization when compared with the emergency cholecystectomy group. This trial concluded that emergency laparoscopic cholecystectomy is preferred to percutaneous cholecystostomy in the management of high-risk patients with acute cholecystitis [45]. Table 1 showing the comparison between percutaneous cholecystostomy and emergency cholecystectomy.
Table 1: The comparison of the mortality, complication, and recurrence rates of PC and EC
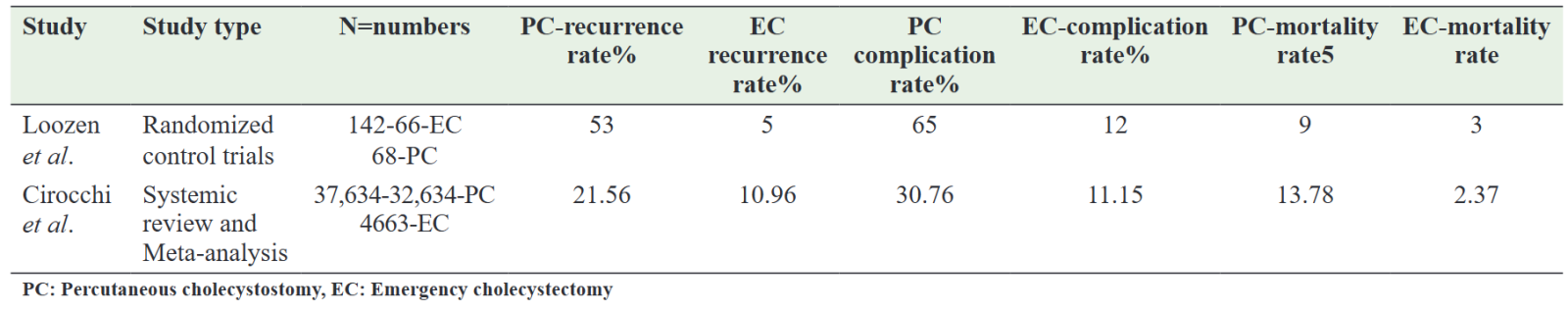
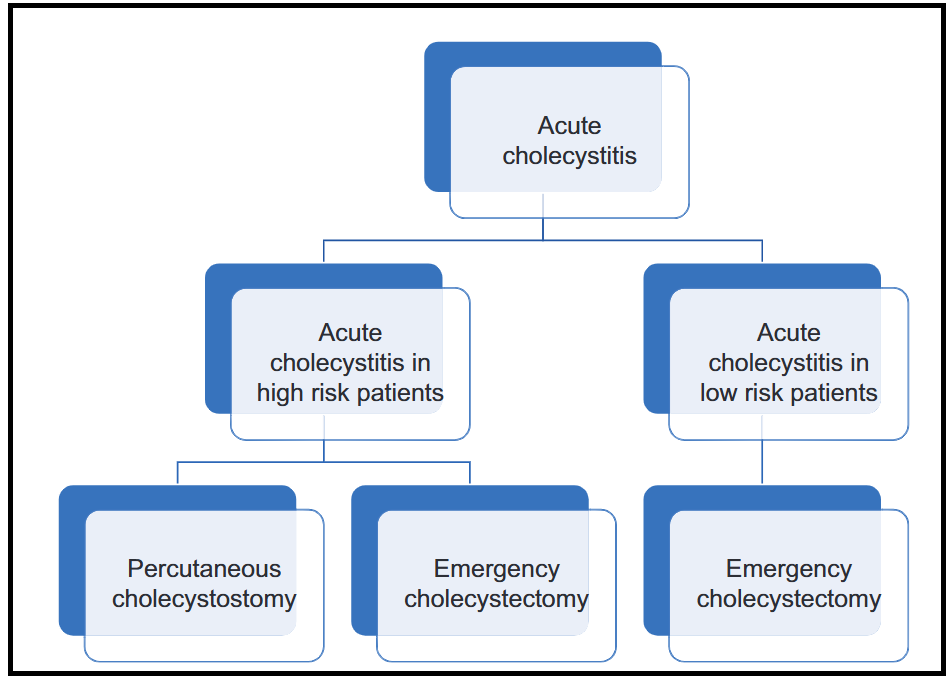
Figure 1: Describes the flow chart of the management of acute cholecystitis
CONCLUSION
Percutaneous cholecystostomy is an ideal bridging tool that can be used in the management of acute cholecystitis in high-risk patients. It is a safe minimally invasive treatment option to stabilize highrisk patients and perform cholecystectomy later. Percutaneous cholecystostomy is associated with reduced morbidity but it is associated with a higher mortality rate and prolonged hospital stay. Several systemic reviews and the multi-center randomized control trials (CHOCOLATE) however have demonstrated that emergency laparoscopic cholecystectomy is associated with better outcomes than percutaneous cholecystostomy in the management of acute cholecystitis in high-risk patients. Percutaneous cholecystostomy still has a role to play in the management of high-risk patients with acute cholecystitis in countries where intensive care management is not available and expertise in surgical management is not available. Future randomized control trials will need to be done by looking at the duration of the cholecystostomy tube, the method of percutaneous cholecystostomy tube insertion, and the recurrence rate. The major drawback of this review was that most of the studies were retrospective and that there were very few prospective studies and randomized control trials. Further research should also be conducted to see if percutaneous cholecystostomy can be performed in mild cases of acute cholecystitis and used to convert patients who would have needed an emergency cholecystectomy to a delayed elective cholecystectomy.
References
1. Halpin V. Acute cholecystitis. BMJ Clin Evid 2014;2014:0411.
2. Gandhi K, Du Plessis R, Klopper J, et al. Percutaneous cholecystostomy placement in cases of non-operative cholecystitis: A retrospective cohort analysis. World J Surg 2020;44:4077-85.
3. Bagla P, Sarria JC, Riall TS. Management of acute cholecystitis. Curr Opin Infect Dis 2016;29:508-13.
4. Cherng N, Witkowski ET, Sneider EB, et al. Use of cholecystostomy tubes in the management of patients with primary diagnosis of acute cholecystitis. J Am Coll Surg 2012;214:196-201.
5. Pisano M, Allievi N, Gurusamy K, et al. 2020 world society of emergency surgery updated guidelines for the diagnosis and treatment of acute calculus cholecystitis. World J Emerg Surg 2020;15:61.
6. Ansaloni L, Pisano M, Coccolini F, et al. 2016 WSES guidelines on acute calculous cholecystitis. World J Emerg Surg 2016;11:25.
7. Yokoe M, Hata J, Takada T, et al. Tokyo guidelines 2018: Diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci 2018;25:41-54.
8. Karakas HM, Yildirim G, Fersahoglu MM, et al. Percutaneous cholecystostomy: An update for the 2020s. North Clin Istanb 2021;8:537-42.
9. Howard JM, Hanly AM, Keogan M, et al. Percutaneous cholecystostomy--a safe option in the management of acute biliary sepsis in the elderly. Int J Surg 2009;7:94-9.
10. Winbladh A, Gullstrand P, Svanvik J, et al. Systematic review of cholecystostomy as a treatment option in acute cholecystitis. HPB (Oxford) 2009;11:183-93.
11. Malik A, Seretis C. Use of percutaneous cholecystostomy for complicated acute lithiasic cholecystitis: Solving or deferring the problem? Pol Przegl Chir 2021;93:7-12.
12. Masrani A, Young D, Karageorgiou JP, et al. Management algorithm of acute cholecystitis after percutaneous cholecystostomy catheter placement based on outcomes from 377 patients. Abdom Radiol (NY) 2020;45:1193-7.
13. Hung YL, Sung CM, Fu CY, et al. Management of patients with acute cholecystitis after percutaneous cholecystostomy: From the acute stage to definitive surgical treatment. Front Surg 2021;8:616320.
14. Popowicz A, Lundell L, Gerber P, et al. Cholecystostomy as bridge to surgery and as definitive treatment or acute cholecystectomy in patients with acute cholecystitis. Gastroenterol Res Pract 2016;2016:3672416.
15. Kortram K, de Vries Reilingh TS, Wiezer MJ, et al. Percutaneous drainage for acute calculous cholecystitis. Surg Endosc 2011;25:3642-6.
16. Horn T, Christensen SD, Kirkegård J, et al. Percutaneous cholecystostomy is an effective treatment option for acute calculous cholecystitis: A 10-year experience. HPB (Oxford) 2015;17:326-31.
17. Higa JT, Sahar N, Kozarek RA, et al. EUS-guided gallbladder drainage with a lumen-apposing metal stent versus endoscopic transpapillary gallbladder drainage for the treatment of acute cholecystitis (with videos). Gastrointest Endosc 2019;90:483-92.
18. Gulaya K, Desai SS, Sato K. Percutaneous cholecystostomy: Evidencebased current clinical practice. Semin Intervent Radiol 2016;33:291-6.
19. Akhan O, Durmaz H, Balcı S, et al. Percutaneous drainage of retroperitoneal abscesses: Variables for success, failure, and recurrence. Diagn Interv Radiol 2020;26:124-30.
20. Chou CK, Lee KC, Chan CC, et al. Early percutaneous cholecystostomy in severe acute cholecystitis reduces the complication rate and duration of hospital stay. Medicine (Baltimore) 2015;94:e1096.
21. Yirgin H, Topal Ü, Tatlıdil Y, et al. What is the effect of percutaneous cholesistostomy in patients with acute cholecystitis? when is the right time for the procedure? [Akut kolesistitli hastalarda perkütan kolesistostominin etkisi nedir? İşlem için doğru zaman ne zaman?] Ulus Travma Acil Cerrahi Derg 2023;29:1269-79.
22. Sanjay P, Mittapalli D, Marioud A, et al. Clinical outcomes of a percutaneous cholecystostomy for acute cholecystitis: A multicentre analysis. HPB (Oxford) 2013;15:511-6.
23. Nasim S, Khan S, Alvi R, et al. Emerging indications for percutaneous cholecystostomy for the management of acute cholecystitis--a retrospective review. Int J Surg 2011;9:456-9.
24. Kesim Ç, Özen Ö. Ultrasound-guided percutaneous cholecystostomy as bridging or definitive treatment in patients with acute cholecystitis grade II or III. Heliyon 2023;9:e15601.
25. Rodríguez-Sanjuán JC, Arruabarrena A, Sánchez-Moreno L, et al. Acute cholecystitis in high surgical risk patients: Percutaneous cholecystostomy or emergency cholecystectomy? Am J Surg 2012;204:54-9.
26. Colonna AL, Griffiths TM, Robison DC, et al. Cholecystostomy: Are we using it correctly? Am J Surg 2019;217:1010-5.
27. Turiño SY, Shabanzadeh DM, Eichen NM, et al. Percutaneous cholecystostomy versus conservative treatment for acute cholecystitis: A cohort study. J Gastrointest Surg 2019;23:297-303.
28. Wang CH, Wu CY, Yang JC, et al. Long-term outcomes of patients with acute cholecystitis after successful percutaneous cholecystostomy treatment and the risk factors for recurrence: A Decade Experience at a single center. PLoS One 2016;11:e0148017.
29. Corbetta Machado MJ, Gray A, Cerdeira MP, et al. Short-and long-term outcomes of percutaneous cholecystostomy in an Australian population. ANZ J Surg 2020;90:1660-5.
30. Kuan LL, Oyebola T, Mavilakandy A, et al. Retrospective analysis of outcomes following percutaneous cholecystostomy for acute cholecystitis. World J Surg 2020;44:2557-61.
31. Garcés-Albir M, Martín-Gorgojo V, Perdomo R, et al. Acute cholecystitis in elderly and high-risk surgical patients: Is percutaneous cholecystostomy preferable to emergency cholecystectomy? J Gastrointest Surg 2020;24:2579-86.
32. Andrén-Sandberg A, Haugsvedt T, Larssen TB, et al. Complications and late outcome following percutaneous drainage of the gallbladder in acute calculous cholecystitis. Dig Surg 2001;18:393-8.
33. Loftus TJ, Collins EM, Dessaigne CG, et al. Percutaneous cholecystostomy: Prognostic factors and comparison to cholecystectomy. Surg Endosc 2017;31:4568-75.
34. Anderson JE, Chang DC, Talamini MA. A nationwide examination of outcomes of percutaneous cholecystostomy compared with cholecystectomy for acute cholecystitis, 1998-2010. Surg Endosc 2013;27:3406-11.
35. Boules M, Haskins IN, Farias-Kovac M, et al. What is the fate of the cholecystostomy tube following percutaneous cholecystostomy? Surg Endosc 2017;31:1707-12.
36. Bundy J, Srinivasa RN, Gemmete JJ, et al. Percutaneous cholecystostomy: Long-term outcomes in 324 patients. Cardiovasc Intervent Radiol 2018;41:928-34.
37. Charrier T, Kepenekian V, Muller A, et al. Management after percutaneous cholecystostomy: What should we do with the catheter? Surg Laparosc Endosc Percutan Tech 2018;28:256-60.
38. Cooper S, Donovan M, Grieve DA. Outcomes of percutaneous cholecystostomy and predictors of subsequent cholecystectomy. ANZ J Surg 2018;88:E598-601.
39. Kayaoglu SA, Tilki M. When to remove the drainage catheter in patients with percutaneous cholecystostomy? Rev Assoc Med Bras (1992) 2022;68:77-81.
40. Park JK, Yang JI, Wi JW, et al. Long-term outcome and recurrence factors after percutaneous cholecystostomy as a definitive treatment for acute cholecystitis. J Gastroenterol Hepatol 2019;34:784-90.
41. Abdelsaid K, Hassan M, Jayasankar B, et al. Percutaneous cholecystostomy in severe acute cholecystitis: An observational study from a single institute. Cureus 2023;15:e34539.
42. Huang H, Zhang H, Yang D, et al. Percutaneous cholecystostomy versus emergency cholecystectomy for the treatment of acute calculous cholecystitis in high-risk surgical patients: A meta-analysis and systematic review. Updates Surg 2022;74:55-64.
43. Cirocchi R, Cozza V, Sapienza P, et al. Percutaneous cholecystostomy as bridge to surgery vs surgery in unfit patients with acute calculous cholecystitis: A systematic review and meta-analysis. Surgeon 2023;21:e201-23.
44. Markopoulos G, Mulita F, Kehagias D, et al. Outcomes of percutaneous cholecystostomy in elderly patients: A systematic review and meta-analysis. Prz Gastroenterol 2021;16:188-95.
45. Loozen CS, van Santvoort HC, van Duijvendijk P, et al. Laparoscopic cholecystectomy versus percutaneous catheter drainage for acute cholecystitis in high risk patients (CHOCOLATE): Multicentre randomised clinical trial. BMJ 2018;363:k3965.
