Full HTML
Pneumomediastinum in association with COVID-19
K Aravind Raj1, Sharad Sable1, A K Saby1, Ketaki Utpat2, Unnati Desai3
Author Affiliation
1Junior Resident, Department of Pulmonary Medicine, T. N. Medical College, B. Y. L. Nair Hospital, Mumbai, Maharashtra, India
2Associate Professor, Department of Pulmonary Medicine, T. N. Medical College, B. Y. L. Nair Hospital, Mumbai, Maharashtra, India
3Associate Professor and Incharge, Department of Pulmonary Medicine, T. N. Medical College, B. Y. L. Nair Hospital, Mumbai, Maharashtra, India
Abstract
Coronavirus disease 2019 (Covid-19) pneumonia is a progressive disease. Respiratory droplets carrying the SARS-COV2 virus enter the upper respiratory tract and multiply in the lungs, causing pneumonia. Many scientific papers have described the most common radiological features of COVID-19 pneumonia, such as multifocal bilateral peripheral areas, subsegmental patchy consolidation, subpleural location, and predominant involvement of the lower lobe and posterior segments. However, the presence of pneumomediastinum has only been reported in a few cases.
DOI: 10.32677/yjm.v2i3.3813
Pages: 180-181
View: 2
Download: 5
DOI URL: https://doi.org/10.32677/yjm.v2i3.3813
Publish Date: 19-12-2023
Full Text
Coronavirus disease 2019 (Covid-19) pneumonia is a progressive disease. Respiratory droplets carrying the SARS-COV2 virus enter the upper respiratory tract and multiply in the lungs, causing pneumonia [1]. Many scientific papers have described the most common radiological features of COVID-19 pneumonia, such as multifocal bilateral peripheral areas, subsegmental patchy consolidation, subpleural location, and predominant involvement of the lower lobe and posterior segments. However, the presence of pneumomediastinum has only been reported in a few cases [2].
A 78-year-old man with a history of hypertension and cerebrovascular accident on regular medication presented with complaints of a four-day high-grade fever associated with chills and dry cough during the first wave of the COVID-19 pandemic. The nasal swab real-time polymerase chain reaction (RT-PCR) test for Covid-19 was positive. On examination, he had no respiratory distress and vital signs were stable. Routine blood work was within normal limits. High-resolution computed tomography (HRCT) of the chest showed bilateral ground-glass opacities (GGO), typical of Covid-19 pneumonia. The patient was initially treated with antivirals and antibiotics. On day 7, the patient showed disease progression with post-exercise desaturation. He had an oxygen saturation (SpO2) of 92% on room air and a SpO2 of 88% after exercise. The patient was transferred to the respiratory intensive care unit. Chest HRCT was repeated; Compared to the previous ones, there was an increase in GGO (25–50% lung involvement). He was treated with non-invasive ventilation (NIV), low molecular weight heparin, steroids, antibiotics, antivirals, and other supportive therapies according to current local guidelines. The patient's symptoms improved upon initial medical treatment. On the 22nd day of hospitalization, the patient complained of chest pain and shortness of breath with nasal twang and increased the fraction of inspired oxygen (FiO2) requirement on NIV. On palpation, crepitus was felt in the neck. Other vital signs were normal. A chest x-ray and repeat chest HRCT examination confirmed pneumomediastinum with subcutaneous emphysema. [Fig. 1a,b]. The patient was treated conservatively. On discharge, his symptoms improved and his vital signs were stable.
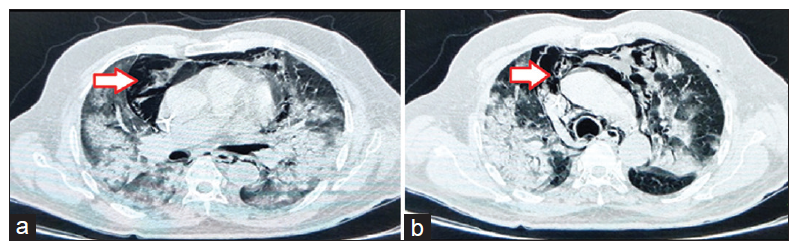
Figure 1: (a) Chest high-resolution computed tomography showing bilateral ground-glass opacities with pneumomediastinum (White arrow). (b) Chest high-resolution computed tomography showing bilateral ground-glass opacities with pneumomediastinum (White arrow)
Pneumomediastinum is a condition in which there is air in the mediastinum. This condition can result from physical trauma or other situations that cause air to escape from the lungs, respiratory tract, or intestines into the mediastinum. Spontaneous pneumomediastinum is uncommon in viral pneumonia. Increased alveolar pressures and diffuse alveolar injury in severe COVID-19 disease with the presence of cough predispose to alveolar rupture along the path of least resistance area i.e. mediastinum causing the pneumomediastinum [3]. The diagnosis can be confirmed by chest x-ray or chest HRCT. The main symptom is usually severe central chest pain. Other symptoms include shortness of breath, voice distortion (like with helium), and subcutaneous emphysema, which particularly affects the face, neck and chest. Pneumomediastinum can also be characterized by shortness of breath typical of a respiratory system problem. It is often recognized on auscultation by a “crunching” sound synchronized with the cardiac cycle (the Hamman crackle). Pneumomediastinum may also present with symptoms mimicking cardiac tamponade due to increased intrapulmonary pressure on venous flow to the heart. The tissues in the mediastinum usually resorb the air slowly in the cavity so most pneumomediastinum cases are treated conservatively [4].
Learning point
- Pneumomediastinum should be considered in the differential diagnosis list of worsening respiratory symptoms and sudden increases in oxygen requirement in COVID-19 patients.
- For COVID-19 patients with worsening respiratory symptoms and a sudden increase in oxygen requirements, physicians should have a low threshold for performing radiological imaging such as chest HRCT.
- Spontaneous pneumomediastinum is a disease with a favorable prognosis if recognized early and in the correct clinical setting of bilateral severe pneumonia.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient for the publication of this report and all associated images.
AUTHORS’ CONTRIBUTIONS
All authors contributed to the completion of this work. The final manuscript was read and approved by all authors
References
- An Introduction to COVID-19. In: Artificial Intelligence for Coronavirus Outbreak. SpringerBriefs in Applied Sciences and Technology. Springer, Singapore 2021. Available at https://doi.org/10.1007/978-981-15-5936-5_1 [accessed on 28th December 2022].
- Romano N, Fischetti A, Melani EF. Pneumomediastinum Related to Covid-19 Pneumonia. Am J Med Sci. 2020 Dec;360(6):e19-e20.
- Kolani S, Houari N, Haloua M, et al. Spontaneous pneumomediastinum occurring in the SARS-COV-2 infection. IDCases. 2020 May 11;21:e00806.
- Kouritas VK, Papagiannopoulos K, Lazaridis G, et al. Pneumomediastinum. Journal of thoracic disease 2015; 7: S44-S49.
