Full HTML
The relationship between healthy lifestyle behaviors and pregnancy distress situations in pregnant women during the COVID-19 epidemic
Reyhan Aydin Dogan1, Esra Yılmaz2, Mehtap Çelik3
Author Affiliation
1Assistant Professor, Department of Midwifery, Faculty of Health Sciences, Karabuk University,
2Karabük Provincial Health Directorate, Eflani District Integrated Hospital,
3Specialist Midwife, Delivery Room, Karabuk Training and Research Hospital, Karabuk, Turkey
Abstract
Background: The COVID-19 pandemic is causing significant changes in pregnant women's healthy lifestyles such as nutrition, physical activity, sleep, and weight gain. This study was conducted to determine the relationship between pregnant women's healthy lifestyle behaviors and distress during the COVID-19 pandemic. Methods: The data were collected between April and October 2021 through face-to-face interviews with pregnant women over 18. The sample of the study consisted of 209 pregnant women. The Tilburg Pregnancy Distress Scale and the Healthy Living Behaviors Scale were used to collect data. Descriptive statistics, parametric tests, and regression analysis methods were used to analyze the data in the study. Results: As a result of the study, the mean Tilburg Distress Scale score of pregnant women was 19.91 ± 9.15. The total psychological distress score of 26.8% of the pregnant women was observed to be higher than the cut-off point. The mean score of the Healthy Living Behaviors Scale of Pregnant Women was 120.71 ± 17.04. It was observed that the Tilburg Distress Scale total score and the spousal Participation sub-dimension score affected pregnant women's Healthy Living Behaviors Scale total score (values p<0.001 and p<0.005, respectively). It was determined that the total score of the Tilburg Distress Scale was 0.34 times effective on the quality of life during pregnancy, and the spousal participation sub-dimension was -2.16 times effective. Conclusion: This study concluded that pregnant women experienced psychological distress during the COVID-19 period and that this situation affected the quality of life of pregnant women.
DOI: 10.32677/yjm.v2i3.4307
Keywords: COVID-19, Healthy lifestyle, Pregnancy, Psychological distress
Pages: 161-167
View: 4
Download: 4
DOI URL: https://doi.org/10.32677/yjm.v2i3.4307
Publish Date: 19-12-2023
Full Text
INTRODUCTION
Pregnancy is a natural process in a woman's life. However, it is a difficult period in which many physical and mental changes are experienced. During this period, a woman's lifestyle and attitude toward pregnancy can change the course of pregnancy [1]. A healthy pregnancy can directly or indirectly affect the health of the fetus. Pregnant women who maintain a healthy lifestyle in the preconception period and throughout pregnancy can protect themselves and their babies from many risks in the prenatal, natal, and postnatal periods [2,3]. For this reason, a healthy lifestyle during pregnancy is essential for adequate fetal development and maternal health [2].
While pregnancy generally refers to emotional relief, it can be perceived as a troublesome process that negatively affects the quality of life for most women. Psychological distress is a negative situation that many women experience throughout their lives. There may be problems in social relations with physical and emotional changes during pregnancy. Changes in body image during pregnancy, inability to adapt, the threat of preterm birth, pregnancy complaints, the feeling of inadequacy, social support inadequacies, anxiety about being a parent, and financial inadequacy can facilitate distress during pregnancy [4,5]. Since distress during pregnancy threatens maternal and fetal health, diagnosing and treating it early is essential [6].
The COVID-19 pandemic, a global problem, causes significant changes in the healthy lifestyle of pregnant women, such as nutrition, physical activity, sleep, and weight gain. In addition, uncertainty brings psychological problems in pregnant women, as in all societies [7–9]. This situation may cause predictable problems during pregnancy, childbirth, and postpartum.
It is thought that pregnant women with healthy lifestyle behaviors may experience the pregnant woman may manage less distress or the distress experienced. This study aimed to determine the relationship between pregnant women's healthy lifestyle behaviors and psychological distress during the COVID-19 pandemic.
MATERIALS AND METHODS
Study Design, Population, and Setting
This prospective, hospital-based, cross-sectional study was conducted between April 4, 2021, and October 4, 2021, at Karabük Training and Research Hospital. Pregnant women who visited the hospital between the specified dates were included in this study. Aarabük Training and Research Hospital is the main referral hospital for maternal and child care in the center of Karabük.
Definition of Cases
Pregnant women who met the inclusion criteria and applied to the hospital between 04 April 2021 and 04 October 2021 were included in this study.
Inclusion Criteria
- Having no problems speaking and writing Turkish
- Being pregnant,
- Not having a chronic disease,
- Agreeing to participate in the study.
Exclusion Criteria
- Not being able to read or write Turkish,
- Having a chronic disease,
- Not agreeing to participate in the study
Sample Size
In this correlational study, the universe consisted of pregnant women living in Karabuk in 2021. The sample of the study consisted of 209 pregnant women according to the results of bivariate normal model power analysis when 95% confidence (1-α), 95% test power (1-β), ρH1 =0.29 and ρH0 = 0.50. When no study examined the relationship between the two scales in the literature, the ρH1 hypothesis was calculated over the low-level correlation value, and the ρH0 hypothesis was calculated over the high-level correlation.
Data Collection
The data were collected by face-to-face interview method between 04.04.2021 and 04.10.2021 with pregnant women who agreed to participate in the study and were over 18. The data were collected using the "Personal Information Form," the Healthy Living Behaviors in Pregnancy Scale (HLBS), and the Tilburg Pregnancy Distress Scale (TPDS). The personal information form consists of 14 questions the researchers prepared, including the pregnant women's socio-demographic characteristics.
Measures
Healthy Living Behaviors in Pregnancy Scale
Developed by Yılmaz and Karahan in 2018, it has 29 items and a "multi-component discrete structure." It consists of 6 (six) subscales as "Pregnancy Responsibility, Nutrition, Hygiene, Physical Activity, Travel and Acceptance of Pregnancy." It is a 5-point Likert type, never (1), rarely (2), occasionally (3), often (4), and always (5). The lowest score that can be obtained on the full scale is 29, and the highest score is 145. The Cronbach Alpha coefficient is 0.83 for the full scale, and the values of the subscales are Pregnancy Responsibility 0.71, Hygiene 0.64, Nutrition 0.73, Physical Activity 0.69, Travel 0.81, and Pregnancy Acceptance 0.63, respectively.
Tilburg Pregnancy Distress Scale
Çapık and Pasinlioğlu performed the Turkish validity and reliability of the TPDS in 2013. The scale consists of 16 items and two sub-dimensions, "Negative Affect" and "Spouse Participation." It is a 4-point Likert type, very often (0), quite often (1), occasionally (2), rarely or never (4). The Negative Affect sub-dimension consists of 11 items, 5,6,7,9,10,11,12,13,14, and 16. These items are reverse-coded. The spouse Participation sub-dimension consists of 5 items 1,2,4,8, and 15. The total Cronbach Alpha coefficient of the scale was found to be 0.83, and the value of the sub-dimensions, respectively, was found to be 0.72 for Spouse Participation and 0.83 for Negative effect. It was determined that the cut-off point of the scale was 28 for the total score. According to the cut-off point, a total score of 28 and above indicates that the pregnant woman is at risk for distress.
Statistical Analysis
The data obtained from the study were evaluated with SPSS for Windows (version 20.0, Statistical Package for Cronbach's Alpha reliability coefficient. It was observed that the data showed a normal distribution since the total score of HLBS, the total score of TPDS, and its sub-dimensions remained within the +2.0/-2.0 limit range of Skewness and Kurtosis values [10]. The sub-dimensions of HLBS did not show a normal distribution. The statistical mean, standard deviation, and minimum and maximum values of the continuous variables in the study are shown. Descriptive statistics of categorical variables were examined with frequency and percentage. The effect of the total score of HLBS, occupation on TPDS, and the number of living children was examined with two-way MANOVA. The factors affecting the total score of HLBS were explained by linear regression. The factors affecting pregnant women with distress according to the cut-off point of TPDS were explained by binary logistic regression. The study examined the relationship between the two scales and their sub-dimensions by Spearman correlation. Multiple comparisons were evaluated with Bonferroni correction. The results of the analysis are presented as mean ± s. deviation. The significance level was taken as p <0.05.
Ethical Consideration
This study was approved by the administration of Karabük Training and Research Hospital. The goals and significance of the current study were explained in detail to the patients in a straightforward manner. Therefore, all participants gave their written, informed consent.
RESULTS
The study found that Cronbach's Alpha value of the total HLBS score was 0.91. The Cronbach's Alpha values of the sub-dimensions of the scale were found to be 0.85 for Pregnancy Responsibility, 0.70 for Hygiene, 0.78 for nutrition, 0.71 for Physical Activity, 0.83 for Travel, and 0.65 for Pregnancy Acceptance. The Cronbach's Alpha value of the TPDS total score was found to be 0.82. When the Cronbach's Alpha values of the sub-dimensions of the scale were examined, the Negative effect was found to be 0.91, and Spouse Participation was found to be 0.74.
In the study, the mean age of the pregnant women was 27.96 ± 5.47, the mean number of pregnancies was 2.09 ± 1.13, the mean gestational week was 34.36 ± 7.00, and the mean weight gained during pregnancy was 11.55 ± 7.75. It was observed that 30.1% of the pregnant women were high school graduates, 74.6%were homemakers, 36.8% of their spouses were secondary school graduates, 39.7% of their spouses worked as workers, 81.3% had a moderate income, 88% had a nuclear family, and 97.6% became pregnant willingly (Table 1).
Table 1: Multiple comparison results of factors affecting healthy living behaviors in pregnant
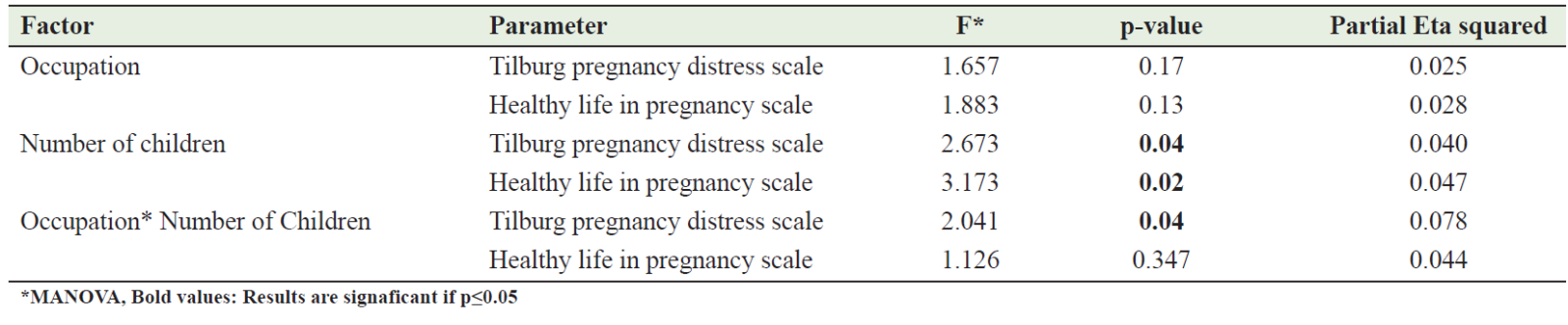
The mean TPDS score was 19.91 ± 9.15. It was observed that 26.8% of the pregnant women had a higher TPSS total score than the cut-off point. The mean score of HLBS was found to be 120.71 ± 17.04. In the study, the main effect of the number of living children of pregnant women was found to be significant in both scales (p values of 0.04 and 0.02, respectively). In both scales, it was observed that the number of children between 2 and 3 and above was higher than the mean scores of the scale. At the same time, the interaction between the number of children living with the profession was observed to have a significant relationship with TPDS (p=0.04). It was determined that the mean scale score of pregnant women with three or more children was higher than the total score average.
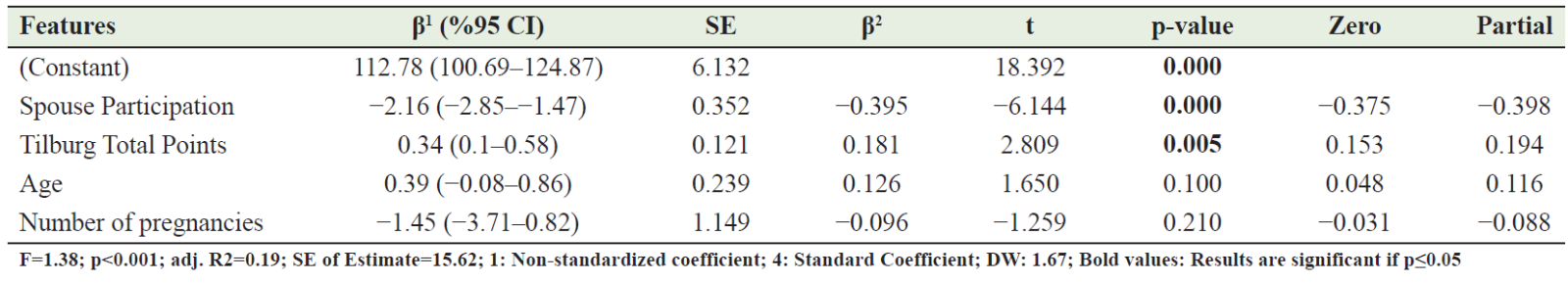
Age, number of pregnancies, total TPDS score, Spousal Participation, and Negative Affect sub-dimension scores affecting the total score of HLBS were explained with a linear regression model. With the model, 19% of the factors affecting healthy lifestyle behaviors in pregnant women were explained. Since the Negative Affect sub-dimension was incompatible, it was excluded from the model. It was observed that the TPDS total score and Spousal Participation sub-dimension score affected the total score of HLBS (p values <0.001 and 0.005, respectively). The TPDS total score was 0.34 times effective on the quality of life during pregnancy, and the spousal participation sub-dimension was -2.16 times effective (Table 2).
Table 2: Linear regression analysis of factors affecting healthy lifestyle behaviors in pregnant women
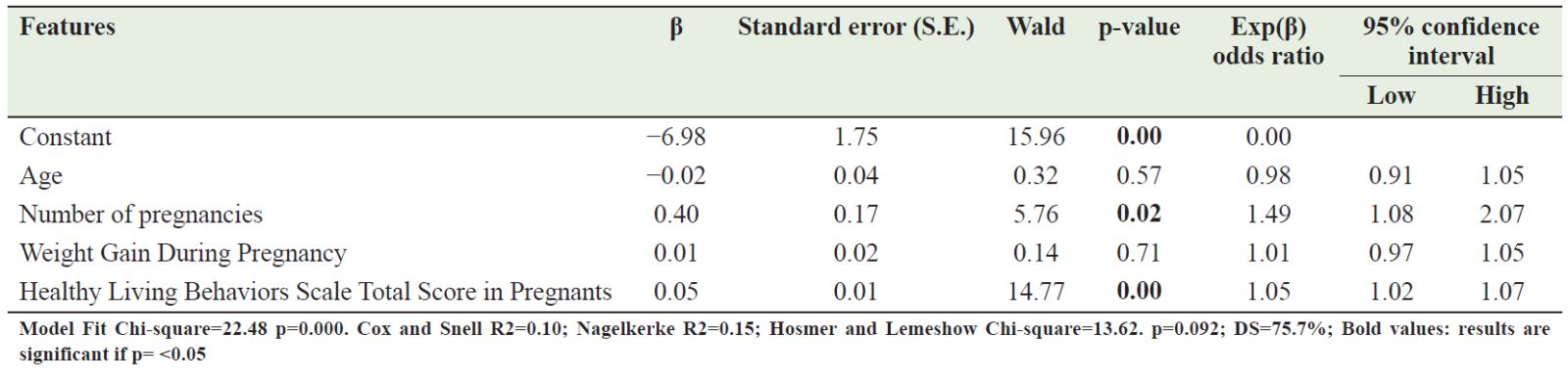
Pregnant women with a total TPDS score higher than 28, according to the cut-off point, were found to be in distress. The factors affecting this, such as age, number of pregnancies, weight gained during pregnancy, and total score of HLBS, were explained by binary logistic regression. The model was observed to be compatible, and the correct classification rate was 75.7%. In the model, it was observed that distress, number of pregnancies, and total score of HLBS had an effect. As the number of pregnancies increased, it was observed that the distress rate of pregnant women increased by 0.40 times. It was determined that pregnant women's distress increased 0.005 times as the total score of HLBS increased (Table 3).
Table 3: Examination of the factors affecting stress in pregnancy by binary logistic regression
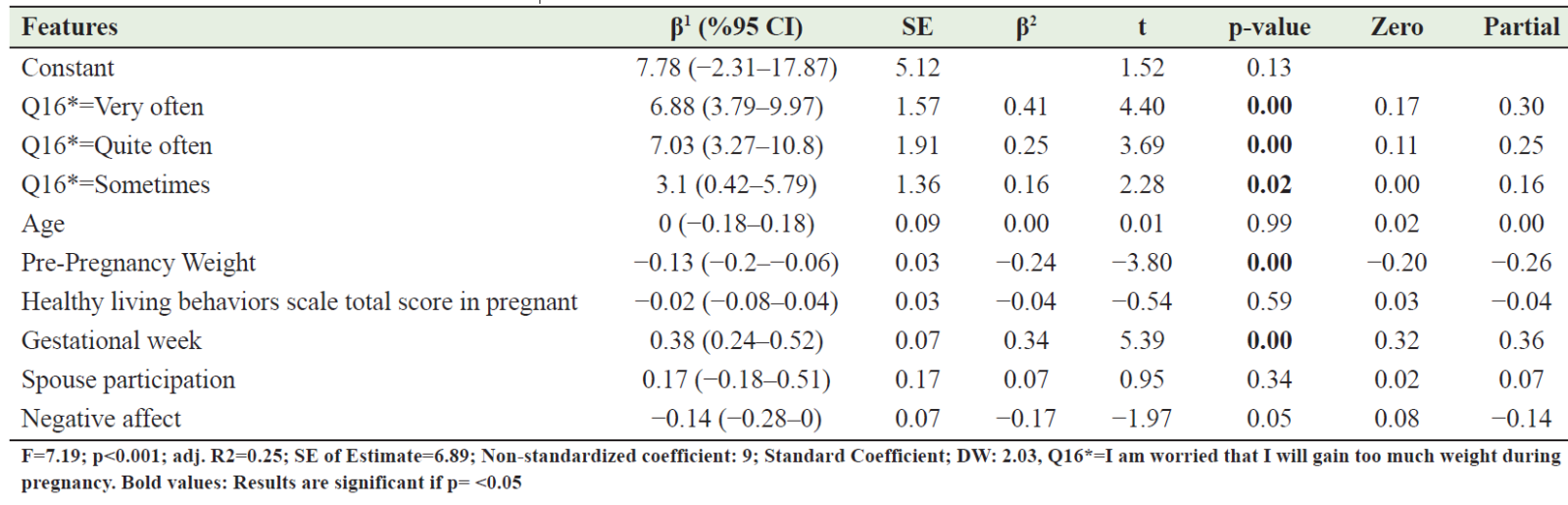
The factors affecting the weight gain of pregnant women were explained by linear regression analysis. Factors affecting weight gain during pregnancy are worrying that I will gain too much weight, age, pre-pregnancy weight, HLBS score, gestational week, total TPDS score, spouse participation, and negative affect sub-dimension scores. Since the total score of TPDS, one of these factors was insignificant, it was automatically excluded from the model by regression. With the model created, 25% of the factors affecting the weight gained until the current gestational week are explained. It was observed that those who rarely worried about gaining weight during pregnancy gained 6.88 times more weight than those who worried very often, 7.03 times more than those who worried quite often, and 3.1 times more than those who worried occasionally. It was observed that the other factor that was significant with the model was the weight gained before pregnancy. It was observed that women who were overweight before pregnancy gained 0.13 times less weight during pregnancy. It was observed that the weight gained during pregnancy and the gestational week was also significant. It was concluded that as the gestational week increased, the weight gained increased 0.38 times (Table 4).
Table 4: Analysis of the factors affecting weight gain during pregnancy by linear regression
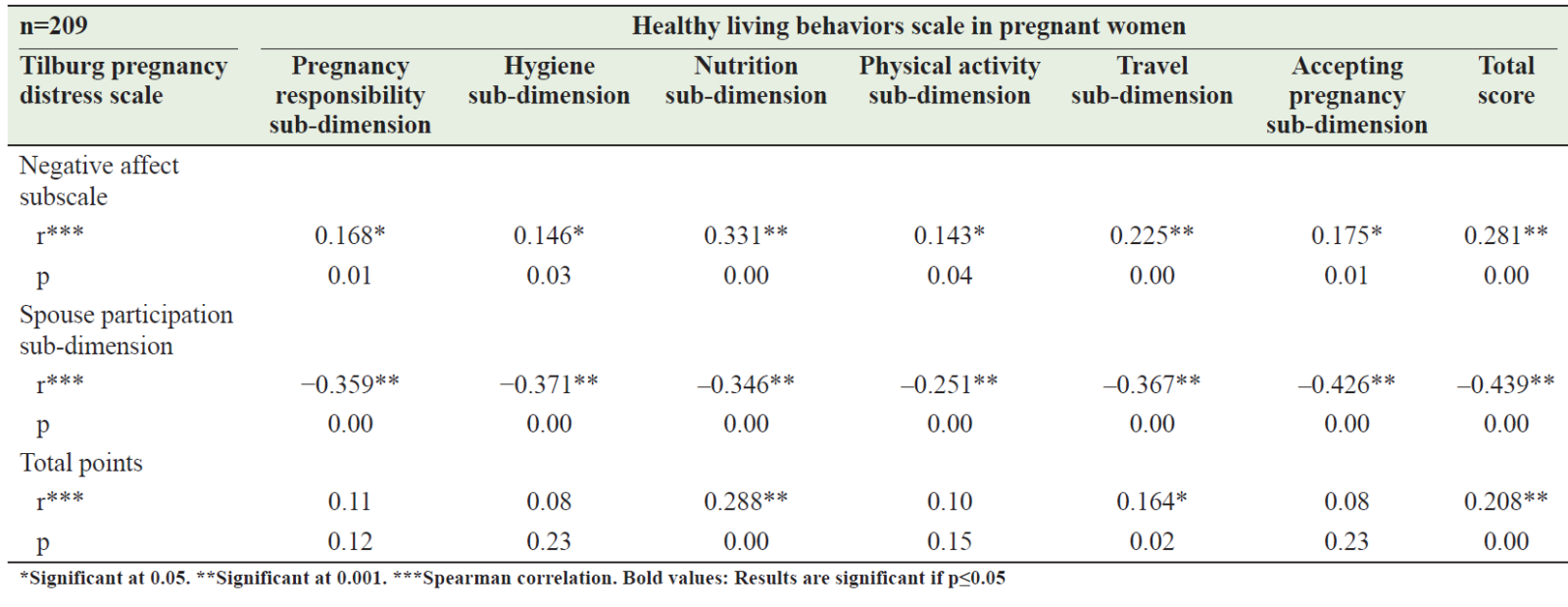
The relationship between TPDS and its sub-dimensions and HLBS and its sub-dimensions was examined by Spearman correlation. A positive low-level significant relationship was found between the total score of the TPDS and the total score of the HLBS (r = 0.28 p = 0.00), a positive low-level significant relationship was found between the Nutrition sub-dimension and the Travel sub-dimension (r = 0.29 p = 0.00), and a positive low-level significant relationship was found between the TGSS and the Travel sub-dimension and the Travel sub-dimension (r = 0.16 p = 0.00). A moderately significant negative correlation (r = -0.44 p = 0.00) was found between the Spousal Participation sub-dimension of HLBS and the total score of HLBS. A moderately negative correlation was found with all its sub-dimensions. A low positive correlation was observed between the Negative Affect sub-dimension of TPDS and the total score of HLBS (r = 0.28 p = 0.00) and all its sub-dimensions (Table 5).
Table 5: The relationship between Tilburg pregnancy distress scale and healthy life behaviors scale in pregnant women
DISCUSSION
A healthy lifestyle and distress level during pregnancy are essential for pregnant women to have a healthy process. The study concluded that there was a positive relationship between the healthy lifestyle behaviors of pregnant women and the level of distress during pregnancy during the pandemic. In addition, it was observed that the healthy lifestyle of pregnant women was at a reasonable level (120.71) during the pandemic, and a significant part (27%) had high distress.
To determine the psychological distress of pregnant women, the mean scores of the current studies using the TPDS scale were found to be 14.23 ± 7.8 points by Kızoğlu and Beydağ (2022), 13.48 ± 8.60 points by Dündar et al. (2019), 20.02 ± 6.28 points by Bacacı and Apay (2018) and 23.66 ± 7.48 points by Yıldız Çiltaş and Köse Tuncer (2019). In the study, the mean TPDS score of pregnant women was found to be 19.91 ± 9.15 [6,11–13]. Since the scores obtained from a scale of 28 and above indicate that pregnant women are in psychological distress, it was concluded that pregnant women participating in this study experienced low levels of distress.
The high level of education of the pregnant woman, her desire for pregnancy, having a nuclear-type family, the presence of social security, having information about pregnancy, planning pregnancy, being pregnant with the first child, spousal support, and having a small number of children can affect pregnancy adaptation and readiness [14,15]. Davoud et al. (2020) found that the quality of life of pregnant women with 1 or 2 children was higher. That psychological health and the number of children were negatively related [16]. Similarly, Hu et al. (2017) found that multiparous women had a higher risk of depression than nulliparous women [17]. The study determined that the number of living children was adequate for pregnant women's perceived distress and healthy living behaviors. As the number of living children increases, the increase in the healthy living behaviors score of pregnant women suggests that they apply the healthy living behaviors they have acquired from the pregnancy they have experienced to their current pregnancy.
There are many studies on the healthy lifestyle behaviors of pregnant women. These studies focused more on socio-demographic factors affecting health behavior. Davoud et al. (2020) concluded that there is a significant relationship between quality of life and educational background, number of children, and profession in pregnant women and that the quality of life of pregnant women with 1 or 2 children and primary school graduates and homemakers is higher [16]. In their study, Çelik and Derya (2019) concluded that the number of pregnancies, living children, parity, the desire for pregnancy, and the number of antenatal care were effective in pregnant women's health practices [18]. Beyaz et al. (2020) found that the mean scores of health practices of pregnant women who worked in any job and had a high level of education were higher [19]. In the study of Özcan et al. (2020), it was determined that there was an increase in the level of health behaviors of pregnant women who were housewives, exercised regularly, had entire sexual life, had a planned pregnancy, and gave their last birth vaginally [20]. The study found that age, number of pregnancies, level of distress during pregnancy, and spousal support were influential in the healthy lifestyle behaviors of pregnant women. This situation requires service planners and servers to evaluate the factors affecting the healthy lifestyle behaviors of pregnant women more broadly and to provide services for their needs. In addition, the services to be provided can be individualized for each pregnant woman and facilitate the acquisition and development of positive health behaviors.
Lack of social support may threaten maternal health during pregnancy and adversely affect pregnancy outcomes [21]. Kanığ and Eroğlu (2020) concluded in their study that there is a positive relationship between the level of perceived social support in pregnancy and healthy lifestyle behaviors. It was determined that as the support of a particular person, family, and friends increased, the level of healthy lifestyle behaviors increased [22]. Similarly, Fathnezhad-Kazemi et al. (2021) found that as the perceived social support score increased in pregnant women, the total score of health promotion behaviors increased[23]. In their study examining the relationship between pregnant women's distress and social support during the COVID-19 pandemic, Goldstein et al. (2022) concluded that pregnant women experience high levels of psychological distress and this situation is mainly due to the lack or lack of social support [24]. In the study, it was concluded that spousal support reduced distress during pregnancy by two times. Unlike the literature, pregnant women with high levels of spousal support had less healthy lifestyle behaviors. This situation has led to an increase in the time spent at home with the spouse during the pandemic period, and this can be explained by the increased spouse support and the fact that pregnant women have less need to seek information for their healthy lifestyle behaviors.
Distress during pregnancy may adversely affect maternal and fetal well-being and seriously threaten pregnancy outcomes. In a cross-sectional study in which Firouzbakht et al. (2022) wanted to determine the coping strategies and depression rate in pregnant women during the COVID-19 pandemic, they concluded that age, education, and residence, which are socio-demographic variables, predict psychological stress and are statistically significant[25]. Similarly, in the study where the level of psychological distress in pregnant women was wanted to be determined during the COVID-19 pandemic, the fear of going to the hospital for occupation, prenatal care, and other health problems, and the fear of being alone and unaided at birth were found to be associated with an increase in the perceived distress score [26]. Crowe et al. (2022) concluded that primiparity, multiparity, trimester, ethnicity, relationship, and working status, which are among the socio-demographic characteristics they questioned, were not effective on perceived stress in their study in which they wanted to determine the stress level of Irish pregnant women during the COVID-19 pandemic [27]. The study found that the number of pregnancies and healthy lifestyle behaviors of the factors affecting pregnant women's distress were adequate. Accordingly, it was observed that as the number of pregnancies and healthy lifestyle behaviors increased, the distress rate of pregnant women increased. These factors may explain 76% of the perceived distress in pregnancy during the COVID-19 pandemic. Factors affecting the distress level in pregnant women have not yet been explained (24%). For this situation, well-designed qualitative research with explicit statements from pregnant women is needed.
Weight gain during pregnancy can cause maternal distress. Nagl et al. (2015), in their systematic review examining the relationship between obesity and anxiety in pregnancy and the postpartum period, concluded that the anxiety level of obese pregnant women was higher[28]. The study concluded that the weight gained during pregnancy was influential in the distress perceived by pregnant women. It was determined that the pregnant woman's age, prenatal weight, gestational week, the thought of gaining more weight during pregnancy, spousal support, and negative emotions affected the weight gained during pregnancy. As the level of anxiety decreased, it was observed that the tendency to gain weight was higher. The motivation-enhancing effect of anxiety can explain this finding.
Mental well-being in pregnant women is associated with health promotion behaviors [29]. But in humans, perfectionist thinking can lead to distress, anxiety, and depression (Flett and Hewitt 2002; Sancar, Kartal, and Gübeş 2021). A woman's desire to manage her pregnancy and perfectionist mindset can create distress. When the literature is examined, no study examines the relationship between healthy lifestyle behaviors and distress levels of pregnant women with COVID-19. The study observed that the distress scores of pregnant women with highly healthy lifestyles increased. This situation can be explained by the fact that pregnant women with high awareness can experience more individual control, dominance over their bodies, high expectations, negative emotions, and distress toward possible consequences.
This study has some limitations that must be considered with caution when discussing the results. The first limitation of this study was that it was descriptive. Study results showed associations, but should not be interpreted as causation. In addition, the fact that the data were collected in the first year of the pandemic period and it was conducted in a single province is an important limitation.
CONCLUSION
The pandemic and extraordinary situations negatively affect maternal and newborn health. Maternal well-being during pregnancy is potentially a marker of antenatal, natal, and postnatal processes. More time should be devoted to training and counseling services to improve the health of pregnant women and optimize pregnancy outcomes. Determination and evaluation of the health behaviors of pregnant women should be made objectively. The needs of pregnant women should be met in line with their individual needs. In addition, well-designed qualitative research should identify obstacles and facilitators pregnant women face; new strategies should be developed, and the care provided should be individualized.
AUTHORS’ CONTRIBUTION
All authors have made a significant contribution to the work reported, whether in conception, study design, implementation, data collection, data analysis, and interpretation, or all of these areas; they also participated in drafting, revising, or critically reviewing the article; and gave final approval to publish the version.
References
1. Rathfisch G, Mecdi̇ M. Evidence-based practices in disorders occurring during pregnancy. Florence Nightingale Journal of Nursing 2014;21:129–38.
2. Cyphers NA, Clements AD, Lindseth G. The relationship between religiosity and health-promoting behaviors in pregnant women. West J Nurs Res 2017;39:1429–46.
3. Yılmaz E, Karahan N. Development and validity and reliability of the Healthy Living Behaviors Scale during Pregnancy. Cukurova Medical Journal 2019;44:498–512.
4. Çapik A. Validity and Reliability Study of the Tılburg Pregnancy Distress Scale. Thesis. Ataturk University, 2013.
5. Yüksel F, Akin S, Durna Z. Prenatal distress in Turkish pregnant women and factors associated with maternal prenatal distress. Journal of Clinical Nursing 2014;23:54–64.
6. Kizoğlu F, Beydağ KD. Prenatal tanı testi için başvuran gebelerin distres düzeyleri ile bebek sağlık denetim odağının belirlenmesi. Abant Sağlık Bilimleri ve Teknolojileri Dergisi 2022;2:18–25.
7. Hori N, Shiraishi M, Harada R, et al. Association of lifestyle changes due to the COVID-19 pandemic with nutrient ıntake and physical activity levels during pregnancy in Japan. Nutrients 2021;13:3799.
8. Luong TC, Pham TTM, Nguyen MH, et al. Fear, anxiety and depression among pregnant women during COVID-19 pandemic: impacts of healthy eating behaviour and health literacy,. Ann Med 2021;53:2120–31.
9. Stampini V, Monzani A, Caristia S, et al. The perception of Italian pregnant women and new mothers about their psychological wellbeing, lifestyle, delivery, and neonatal management experience during the COVID-19 pandemic lockdown: a web-based survey. BMC Pregnancy Childbirth 2021;21:473.
10. George D. SPSS for windows step by step: A simple study guide and reference, 17.0 update, 10/e. Pearson Education India. 2011.
11. Bacaci H, Apay SE. The relationship between body image perception and distress in pregnant women 2018.Journal of Düzce University Health Sciences Institute;8:76–82.
12. Çiltaş, Yıldız N, Tunce, Köse S. Defining distress in pregnancy: Erzincan example. Mehmet Akif Ersoy University Health Sciences Institute Journal 2019;7:15–24.
13. Dündar T, Özsoy S, Aksu H, et al. Effect of obstetric characteristics on distress during pregnancy 2019;22:17–24.
14. Demirbas H, Kadıoğlu H. Adaptation of women in the prenatal period to pregnancy and related factors. MUSBED 2014;4:200–6.
15. Yekenkunrul D, Mete S. Examination of the relationship between nausea and vomiting during pregnancy, marital adjustment and spousal relationship. Journal of Dokuz Eylül University School of Nursing 2020;5:89-95.
16. Davoud A, Abazari M. The Relationship between quality of life and physical activity, worry, depression, and ınsomnia in pregnant women. Iran J Psychiatry 2020;15:159–68.
17. Hu HQ, Zhang J, Zhao W, et al. The occurrence and determinants of anxiety and depression symptoms in women of six counties/ districts in China during pregnancy. Zhonghua yu fang yi xue za zhi [Chinese journal of preventive medicine] 2017;51:47–52.
18. Celik AS, Derya YA. Determination of pregnant women's self-care power and health practices levels and affecting factors. GÜSBD 2019;8:111–9.
19. Beyaz E, Gökçeoğlu S, Özdemi̇r N. Determination of health practice levels of pregnant women in Muş city center. Van Sag Bil Derg. 2020;13:9–16.
20. Özcan H, Polat T, Öztürk A, et al. Determination of healthy lifestyle behaviors and affecting factors in pregnant women. Online Turkish Journal of Health Sciences 2020;5:482–92.
21. Fleuriet KJ, Sunil TS. Perceived social stress, pregnancyrelated anxiety, depression and subjective social status among pregnant Mexican and Mexican American women in south Texas. Journal of Health Care for the Poor and Underserved 2014;25:546–61.
22. Kanığ M, Eroglu K. Investigation of the relationship between the level of perceived social support and healthy lifestyle behaviors of pregnant women. Journal of Psychiatric Nursing 2020;11:333–40.
23. Fathnezhad-Kazemi A, Aslani A, Hajian S. Association between perceived social support and health-promoting lifestyle in pregnant women: A Cross-sectional study. J Caring Sci 2021;10:96–102.
24. Goldstein E, Brown RL, Lennon RP, et al. Latent class analysis of health, social, and behavioral profiles associated with psychological distress among pregnant and postpartum women during the COVID‐19 pandemic in the United States. Birth 2022:10.1111/birt.12664.
25. Firouzbakht M, Rahmani N, Sharif Nia H, et al. Coping strategies and depression during the COVID-19 pandemic in pregnant women: a cross sectional study. BMC Psychiatry 2022;22:1–8.
26. Rimal SP, Thapa K, Shrestha R. Psychological distress and coping among pregnant women during the COVID 19 pandemic. J Nepal Health Res Counc 2022;20:234–40.
27. Crowe S, Sarma K. Coping with Covid-19: stress, control and coping among pregnant women in Ireland during the Covid-19 pandemic. BMC Pregnancy Childbirth 2022;22:274.
28. Nagl M, Linde K, Stepan H, et al. Obesity and anxiety during pregnancy and postpartum: A systematic review. Journal of Affective Disorders 2015;186:293–305.
29. Pasha H, Faramarzi M, Chehrazi M, et al. Health-promotion and health-harming behaviours in pregnant women: role of coping strategies, anxiety, and depression. Journal of Obstetrics and Gynaecology 2022;42:410–5.
30. Flett GL, Hewitt PL. Perfectionism and maladjustment: An overview of theoretical, definitional, and treatment issues. Perfectionism: Theory, research, and treatment, Washington, DC, US: American Psychological Association; 2002, p. 5–31.
31. Sancar Y, Kartal S, Gübeş NÖ. Examining the relationship between teachers' burnout and perfectionism levels. Uşak University Journal of Social Sciences 2021:156–73.
