Full HTML
A case of pneumomediastinum after dental root canal treatment
Özkan Kömürcü, Hatice Güldal, Yasin Haydar Yartaşı, Doğukan Güler, Mustafa Boğan
Author Affiliation
1Specialist, Department of Emergency, Şehitkamil State Hospital, Gaziantep,
2Resident, Department of Emergency, School of Medicine, Düzce University, Düzce, Turkey,
3Consultant, Department of Emergency, School of Medicine, Düzce University, Düzce, Turkey
Abstract
We presented a rare case in which a 27-year-old female patient developed cervicofacial emphysema and pneumomediastinum following dental root canal treatment on her lower right second molar. She presented to the emergency department with facial and neck pain, difficulty in swallowing, and a feeling of tightness and pressure in the chest. Computed tomography revealed free air foci extending from the right mandibular region to the mediastinum. Pneumomediastinum related to dental root canal treatment was considered and the patient was admitted to the thoracic surgery department and oxygen therapy and prophylactic antibiotics were initiated. After 3 days of observation, the emphysema resolved, the symptoms disappeared, and the inflammatory markers remained within normal limits. The patient was discharged in stable condition.
DOI: 10.32677/yjm.v2i3.4195
Keywords: Cervicofacial emphysema, Dental root therapy, Pneumomediastinum
Pages: 174-176
View: 2
Download: 3
DOI URL: https://doi.org/10.32677/yjm.v2i3.4195
Publish Date: 19-12-2023
Full Text
Pneumomediastinum is a condition characterized by the accumulation of extra-alveolar air in the mediastinum [1-3]. Spontaneous pneumomediastinum refers to the presence of air in the mediastinum of a healthy person without an obvious trigger such as surgery, visceral perforation, infection, or trauma. Once the causative factor is identified, the presence of air in the mediastinum is considered secondary pneumomediastinum [4]. Spontaneous pneumomediastinum has been linked to various respiratory techniques that cause the development of high intrathoracic pressures such as Valsalva maneuvers, coughing, vigorous crying, and forceful retching or vomiting [5]. Secondary pneumomediastinum can develop as a result of chest trauma or a severe asthma attack, as well as during mechanical ventilation, surgery, or diagnostic procedures. Tracheal, bronchial, or esophageal ruptures as well as dental procedures can less frequently lead to pneumomediastinum [4-6]. Pneumomediastinum as a result of emphysema in the cervicofacial area after dental root canal treatment (endodontics) is rare. We presented such a case to alert physicians about this important condition, which is usually misdiagnosed as an allergic reaction in emergency rooms and leads to treatment errors.
CASE REPORT
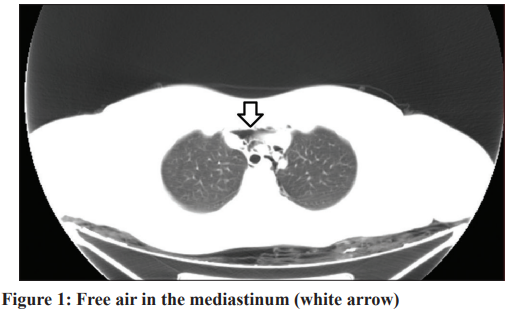
A 27-year-old female patient presented to the emergency department with facial and neck pain, difficulty in swallowing, and a feeling of tightness and pressure in the chest. The patient mentioned that these symptoms started a day before her presentation, following dental root canal treatment (endodontics) on her lower right second molar. On examination, the patient was conscious and alert with normal blood pressure. Her body temperature was 37.0°C, she was breathing at a rate of 18 breaths per minute, and her oxygen saturation level was 96% on room air. Examination of the oropharynx and oral mucosa revealed no abnormalities, but crepitus without local tenderness or erythematous change was noted in an area between the right parotid gland and the neck, indicating the presence of cervicofacial emphysema. Examination of other systems was unremarkable. Chest X-ray was unremarkable and the electrocardiogram showed a normal sinus rhythm. Flexible laryngoscopy results were normal. Complete blood count, serum electrolytes, liver, and kidney function tests were within normal limits. C-reactive protein levels also were within the normal ranges. Chest computed tomography revealed free air foci extending from the right mandibular region to the mediastinum (Fig. 1). Pneumomediastinum related to dental root canal treatment was considered and the patient was admitted to the thoracic surgery department. Oxygen therapy and prophylactic antibiotics were initiated. After 3 days of observation, the emphysema resolved, the symptoms disappeared, and the inflammatory markers remained within normal limits. The patient was discharged in stable condition.
DISCUSSION
Pneumomediastinum secondary to cervicofacial emphysema is extremely rare and has been reported in the literature following head-and-neck surgery, trauma to the face and oral cavity, and dental procedures [7]. Dental procedures as a secondary cause of pneumomediastinum were first reported in 1870 when a musician in a band experienced swelling on the side of tooth extraction after immediately playing the trumpet. Military doctor Alexander Turnbull was fascinated by this clinical presentation and called it traumatic emphysema [8]. Dental procedures reported to cause pneumomediastinum include tooth extraction, preparation, restorative treatment, endodontic treatment, and subgingival curettage, which involve the use of handpieces and high-pressure air/water syringes [9,10]. Our patient developed pneumomediastinum secondary to cervicofacial emphysema after endodontic treatment. The development of cervicofacial emphysema and pneumomediastinum after dental procedures, especially procedures on the posterior mandibular teeth, may be due to the anatomical structure of the region. The roots of the first, second, and third mandibular molars are known to communicate directly with the sublingual and submandibular spaces. These communicate with the pterygomandibular, parapharyngeal, and retropharyngeal spaces, the latter communicating with the mediastinum [11,12]. This allows air to enter the pericardium, pleural cavity, retroperitoneum, and mediastinum. In addition, the spread of microorganisms of the oral flora along the emphysematous tracts may be responsible for soft-tissue infections such as deep neck infections and mediastinitis [12]. The clinical presentation of cervicofacial emphysema and pneumomediastinum after dental procedures includes acute swelling of the cervicofacial region, chest pain, shortness of breath, chest pressure, difficulty swallowing, and a sore throat. Our patient presented with facial and neck pain, difficulty in swallowing, and a feeling of tightness and pressure in the chest. These symptoms are non-specific and can occur in many clinical conditions following dental procedures. In addition to cervicofacial emphysema, the differential diagnosis of acute swelling of the cervicofacial region after dental procedures may include angioedema secondary to the use of some medications such as non-steroidal anti-inflammatory drugs or local anesthetics. Other differential diagnoses include soft-tissue infections, which are characterized by systemic and local manifestations such as fever, local redness, and hotness [12]. Palpable crepitus without local signs of inflammation is a pathognomonic sign of cervicofacial emphysema [13], which in our case could have helped emergency physicians make the correct diagnosis and avoid unnecessary investigations and treatments. Serious complications may develop as a result of pneumomediastinum. These include pneumothorax, cardiac tamponade, airway obstruction, air embolism, necrotizing soft-tissue infections, and mediastinitis [12]. Identifying and treating the underlying cause is an essential part of managing cervicofacial emphysema and pneumomediastinum. Air is naturally absorbed by soft tissue; therefore, it is recommended to admit the patient, administer antibiotics, observe the patient, and ensure the emphysema and pneumomediastinum which do not worsen, and the respiratory status remains uncompromised. Our patient was admitted to the thoracic surgery department for observation and oxygen therapy and prophylactic antibiotics were initiated for 3 days. He was subsequently discharged with resolved emphysema and symptoms disappeared.
CONCLUSION
The emergency physician should be aware that the presentation of a patient with shortness of breath and acute swelling of the cervicofacial region after dental root canal treatment may indicate the diagnosis of cervicofacial emphysema and pneumomediastinum, which must be recognized and treated as early as possible to avoid possible complications.
Consent for Publication
Written informed consent was obtained from the patient for publication of this case report and all accompanying images.
AUTHORS’ CONTRIBUTIONS
All authors contributed to the completion of this work. The final manuscript was read and approved by all authors
References
1. Molla YD, Abegaz SH, Desita ZT. Spontaneous pneumomediastinum with subcutaneous emphysema in a young healthy female, a case report. Heliyon 2023;9:e18326.
2. Deskins SJ, Brunner NE, Brunner M. A case report on subcutaneous emphysema and pneumomediastinum following a routine dental procedure. Cureus 2023;15:e41177.
3. Grooteman KV, van den Bergh JE, Tukkie R, et al. Een onschuldige vorm van pneumomediastinum [A harmless form of pneumomediastinum: Avoid unnecessary diagnostics and treatment]. Ned Tijdschr Geneeskd 2023;167:D7309.
4. Kouritas VK, Papagiannopoulos K, Lazaridis G, et al. Pneumomediastinum. J Thorac Dis 2015;7:S44-9.
5. Afzali N, Malek A, Attar AH. Cervicofacial emphysema and pneumomediastinum following dental extraction: Case report. Iran J Pediatr 2011;21:253-5.
6. Yoshimoto A, Mitamura Y, Nakamura H, et al. Acute dyspnea during dental extraction. Respiration 2002;69:369-71.
7. Rad MV, Chan EK, Ahmed IH. Cervicofacial subcutaneous emphysema and pneumomediastinum secondary to dental treatment in a young man. Respir Med Case Rep 2019;28:100918.
8. Turnbull A. A remarkable coincidence in dental surgery. Br Med J 1900;1:1131.
9. Jones A, Stagnell S, Renton T, et al. Causes of subcutaneous emphysema following dental procedures: A systematic review of cases 1993-2020. Br Dent J 2021;231:493-500.
10. Feinstone T. Infected subcutaneous emphysema: Report of case. J Am Dent Assoc 1971;83:1309-11.
11. Josephson GD, Wambach BA, Noordzji JP. Subcutaneous cervicofacial and mediastinal emphysema after dental instrumentation. Otolaryngol Head Neck Surg 2001;124:170-1.
12. Frühauf J, Weinke R, Pilger U, et al. Soft tissue cervicofacial emphysema after dental treatment: Report of 2 cases with emphasis on the differential diagnosis of angioedema. Arch Dermatol 2005;141:1437-40.
13. Sarfi D, Haitami S, Farouk M, et al. Subcutaneous emphysema during mandibular wisdom tooth extraction: Cases series. Ann Med Surg (Lond) 2021;72:103039.
