Full HTML
The accuracy of gross medical thoracoscopy findings in the diagnosis of pleural tuberculosis: A hospital-based study from Qatar
Aisha Aladab, Anam Elarabi, Mousa Hussein, Gokhan Demir, Adel Issam Albozom, Hassan Ibrahim, Khaled Mohamed Al-arb, Osaid Yousef Al-Qahoush, Ali Ibrahim, Hussain Ibrahim, Mohammad Jamal Abushanab, Mohammed Salah Makawi, Musaab Fahmi Yousef
Author Affiliation
1Senior Consultant Pulmonary and Sleep Medicine,
2Consultant Pulmonary and Sleep Medicine,
4Registered Nurse, Bronchoscopy Unit, Department of Pulmonology,
3Resident, Department of Medicine, Hamad General Hospital,
5Medical Student, Department of Medicine, Qatar University, Medical College, Doha, Qatar,
6Medical Student, Department of Medicine, Jordan University of Science and Technology,
7Medical Student, Department of Medicine, University of Jordan, School of Medicine, Amman, Jordan
Abstract
Background: Pleural tuberculosis (TB) diagnosis is a challenging clinical entity. Medical thoracoscopy (MT) is quickly replacing other diagnostic methods as the preferred diagnostic method for exudative pleural effusions. This study aimed to describe the gross MT findings in pleural TB and to evaluate the accuracy of these findings in the diagnosis of pleural TB in terms of sensitivity and specificity. Methods: This is a retrospective descriptive study involving all patients who underwent MT in the pulmonary department of Hamad General Hospital, from January 2014 to December 2019 to determine the etiology of undiagnosed pleural effusions. Results: We studied 400 cases, 353 (88.3%) were male and 47 (11.7%) were female. Their mean age was 37.49±12.46 years. Gross MT findings included free fluid 400 (100%), nodules 307 (76.8%), adhesions 226 (56.5%), pleural thickening 382 (95.5%), and pleural hyperemia 366 (91.5%). Confirmed cases of pleural TB based on histomicrobiologic studies were 320 (80.0%). The specificities of pleural nodules, adhesions, thickening, and hyperemia were 52.50%, 11.25%, 50.00%, and 25.00%, respectively. While the sensitivities for pleural nodules, adhesions, thickening, and hyperemia were 58.75%, 97.19%, 83.44%, and 95.62%, respectively. Conclusion: Gross MT findings without pleural nodules, hyperemia, and thickening can be used to rule out pleural TB, thereby allowing the treating physician to postpone antitubercular therapy until the final diagnosis is confirmed. However, the presence of these gross findings has no significant association with pleural TB. On the other hand, pleural adhesions showed low sensitivity and specificity for pleural TB.
DOI: 10.32677/yjm.v2i3.4346
Keywords: Malignant tuberculosis, Medical thoracoscopy, Pleural effusion, Pleural tuberculosis
Pages: 157-160
View: 3
Download: 6
DOI URL: https://doi.org/10.32677/yjm.v2i3.4346
Publish Date: 19-12-2023
Full Text
Pleural tuberculosis (TB) is one of the most common sites of extrapulmonary TB, although the incidence varies by region [1]. Pleural TB, which accounts for 10–48% of all cases worldwide [2-7], remains a diagnostic challenge and cannot be diagnosed based on clinical findings that are quite complex, nonspecific, and similar to other diseases, including pneumonia and cancer. Blood biochemistry, complete blood cell count, and radiographic studies are of limited diagnostic value. Acid-fast smear of pleural fluid has a low yield and cultures require weeks to give results and are positive in 30–70% of diagnosed cases [8]. Polymerase chain reaction (PCR) analysis for rapid detection of bacillus tubercles in pleural fluid has low yield, and the role of other biomarkers such as adenosine deaminase and gamma interferon is less well described and currently being evaluated as diagnostic tools [8,9]. Medical thoracoscopy (MT) with targeted biopsy provides a quick and correct diagnosis in 63–100% of cases and should be carried out early in suspected cases [8-11]. The characteristic gross findings documented by thoracoscopy in pleural TB include adherence, thickening, nodules, pleural hyperemia, and plaques [12]. The accuracy of these macroscopic findings in suspecting pleural TB is not widely studied worldwide. This study aimed to describe the gross MT findings in pleural TB and to evaluate the accuracy of these findings in the diagnosis of pleural TB in terms of sensitivity and specificity.
MATERIALS AND METHODS
Study Design, Population, and Setting
This was a retrospective descriptive study of all patients who underwent MT to determine the cause of undiagnosed exudative pleural effusions after initial hematological, microbiological, and cytological analyses were inconclusive. In the present study, exudative pleural effusion was diagnosed using Light’s criteria. The study was carried out in the pulmonary department of Hamad General Hospital (the only tertiary referral center in Qatar that performs MT) from January 1, 2014, to December 31, 2019.
Procedure
All patients underwent diagnostic MT under local anesthesia. The pleural space was systematically examined, and a biopsy of the visible nodules, adhesions, pleural thickening, and hyperemic areas was taken and sent for histopathology, Ziehl–Neelsen stains, TB culture, and TB-PCR. Pleural fluid was sent for Ziehl– Neelsen staining, TB-PCR, and TB culture. An intercostal drain was inserted for up to 48 h.
Case Definitions
Sample Size All cases with undiagnosed exudative pleural effusion that was identified during the study period were involved in this study (complete enumeration).
Data Collection
We obtained the list of patients who underwent MT during the period of study from the records of the pulmonology unit at Hamad General Hospital. The electronic medical records of the patients were reviewed retrospectively and the following variables were retrieved: age, gender, origin (distribution according to 5 regions of the national territory), occupation, symptoms (cough, dyspnea, fever, weight loss, and pleuritic pain), and results of pleural fluid study. The gross MT findings were classified into four patterns: pleural hyperemia, nodules, pleural thickening, and pleural adhesions.
Statistical Analysis
This study used simple descriptive statistics. Data were presented as the mean±SD for quantitative variables, whereas qualitative variables were described as numbers and percentages. To assess the accuracy of the findings in the diagnosis of pleural TB, we used the medical calculator (MedCalc) [13], to calculate the accuracy of tests in terms of sensitivity and specificity.
Ethical Aspects
This study obtained ethical approval from the research committee at Hamad Medical Corporation (Protocol # MRC-01-20-175).
RESULTS
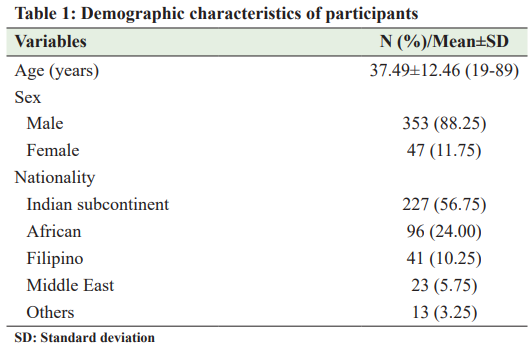
From January 1, 2014, to December 31, 2019, we studied 400 cases of exudative pleural effusion who underwent MT in the Department of Pulmonology, Hamad General Hospital, Doha, Qatar. The mean age of the patients was 37.49±12.46 years (range: 19–89 years). Out of 400, there were 353 (88.3%) male and 47 (11.7%) female patients. Most of our patients were nonQataris, particularly from the Indian subcontinent (Table 1). The gross MT findings included free fluid 400 (100%), nodules 307 (76.8%), adhesions 226 (56.5%), pleural thickening 382 (95.5%), and pleural hyperemia 366 (91.5%). Confirmed cases of pleural TB based on histomicrobiologic studies were 320 (80.0%). Non-TB cases included acute/chronic inflammation 37 (9.25%), malignancy 27 (6.75%), fibrinous exudate 10 (2.5%), and others 11(2.75%) (Table 2). We compared the gross MT findings with the final diagnosis to assess the accuracy of these findings in diagnosing pleural TB in terms of sensitivity and specificity. The specificities of pleural nodules, adhesions, thickening, and hyperemia were 52.50%, 11.25%, 50.00%, and 25.00%, respectively, while the sensitivities for pleural nodules, adhesions, thickening, and hyperemia were 58.75%, 97.19%, 83.44%, and 95.62%, respectively. Table 3 summarizes the diagnostic acccuracy of the gross MT findings in the diagnosis of pleural TB.
DISCUSSION
Pleural biopsy gives a better diagnostic value than pleural fluid alone. It can be obtained by different procedures including closed pleural biopsies, thoracoscopy, or open surgical biopsies [14]. MT
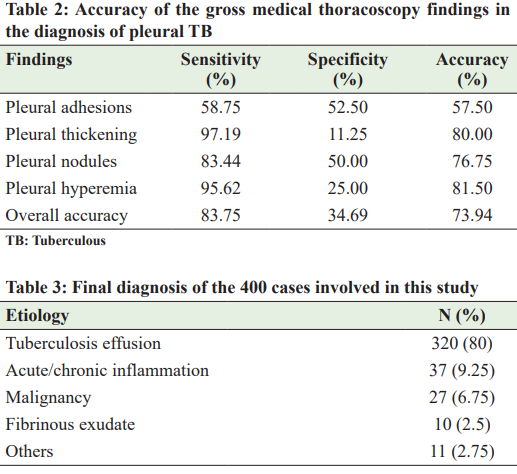
is the thoracoscopic examination of the pleural space in a nonintubated patient under local anesthesia. It is well-documented that this procedure is safe and highly sensitive for the diagnosis of exudative pleural effusions as it allows the collection of pleural biopsies under direct visualization [15]. The gross MT findings are the first and most direct insights into MT. Therefore, the selection of areas for biopsy sampling depends on the operator’s familiarity with various macroscopic findings and the accuracy of these findings in diagnosing pleural TB to increase the diagnostic yield of the selected biopsy. In addition, since histological examination usually takes 5–7 days in many hospitals [16], macroscopic MT findings can give physicians an early impression of the diagnosis and help them initiate antituberculous treatment, thereby avoiding undesirable complications due to delayed initiation of therapy. In one study, the characteristic macroscopic (gross) findings of video-assisted thoracoscopy in pleural TB included free pleural fluid, adherence, thickening, nodules, pleural hyperemia, and plaques [12]. In this study, we grouped the gross MT findings into four groups, namely, pleural nodules, pleural adhesions, pleural thickening, and pleural hyperemia. Of these, the presence of pleural thickening was the most commonly described finding (95.5%) followed by pleural hyperemia (91.5%). These two findings showed higher sensitivities for the diagnosis of pleural TB compared with other findings, 97.19% and 95.62%, respectively. However, these two findings showed low specificity for the diagnosis of pleural TB, namely, 11.23% and 25%, respectively. Therefore, pleural thickening and hyperemia can be used as good indicators to exclude pleural TB, thereby avoiding unnecessary initiation or continuation of antituberculous therapy even if the final histomicrobiological findings are inconclusive. Other gross findings in the present study included pleural nodules 76.8% and adhesions 56.5%. Our study showed that pleural nodules had a sensitivity of 83.44% for the diagnosis of pleural TB, which is consistent with a study by Kumar et al. [17], who found that pleural nodules had a sensitivity of 83%, but unlike another study by Thomas et al. [18], who found that pleural nodules had a sensitivity of 58%. On the other hand, pleural nodules in our study showed low specificity (50%) for pleural TB, unlike the other two studies by Kumar et al. and Thomas et al., who found that the specificities of pleural nodules to pleural TB were 100% and 89%, respectively. Therefore, our study demonstrated that the presence of pleural nodules has no significant association with pleural TB. However, the absence of nodules can be used to exclude pleural TB, justifying the delay in starting antituberculous therapy until the final diagnosis is confirmed. Interestingly, we found that the pleural adhesions had low sensitivity and specificity for the diagnosis of pleural TB. The retrospective design of our study is the main limitation of our study. Furthermore, due to the hospital-based nature, it is not possible to generalize our results. However, the strength of our study lies in the sample size, which was large enough to validate our results compared to other studies [17,18].
CONCLUSIONS Our study showed that the gross MT findings have high sensitivity, but lack specificity. Therefore, the absence of pleural nodules, hyperemia, and thickening on MT can be used to rule out pleural TB, thereby allowing the treating physician to delay antituberculous therapy until the final diagnosis is confirmed. However, the presence of these gross findings has no significant association with pleural TB. On the other hand, pleural adhesions showed low sensitivity and specificity for the diagnosis of pleural TB. AUTHORS’ CONTRIBUTIONS All authors have made a significant contribution to the work reported, whether in conception, study design, implementation, data collection, data analysis, and interpretation, or all of these areas, they also participated in drafting, revising, or critically reviewing the article and gave final approval to publish the version
References
1. Cohen LA, Light RW. Tuberculous pleural effusion. Turk Thorac J 2015;16:1-9.
2. Hezam HS, Humaidah SH. Prevalence of tuberculosis in Shabwah governorate, Yemen: A cross-sectional study. Yemen J Med 2022;1:36-9.
3. Khattab MA, Khan FY, Maslamani M, et al. Pulmonary and extra pulmonary tuberculosis in Qatar: A first retrospective population-based study. Adv Infect Dis 2015;5:148-53.
4. Basamed JM, Alamoudi KA, Khan FY. Prevalence of tuberculosis in Hadramout Al-Sahel, Yemen: A 1-year cross-sectional study. Yemen J Med 2023;2:33-6.
5. Sabu SK, Paul V, Mathew DJ, et al. Changing trends in incidence and clinical spectrum of extra-pulmonary tuberculosis: A 10-year retrospective study in a rural teaching hospital in South India. Int Surg J 2019;6:220-6.
6. Tahseen S, Khanzada FM, Baloch AQ, et al. Extrapulmonary tuberculosis in Pakistan-a nation-wide multicenter retrospective study. PLoS One 2020;15:e0232134.
7. Macías A, Sánchez-Montalvá A, Salvador F, et al. Epidemiology and diagnosis of pleural tuberculosis in a low incidence country with high rate of immigrant population: A retrospective study. Int J Infect Dis 2019;78:34-8.
8. Vorster MJ, Allwood BW, Diacon AH, et al. Tuberculous pleural effusions: Advances and controversies. J Thorac Dis 2015;7:981-91.
9. Khan FY, Hamza M, Omran AH, et al. Diagnostic value of pleural fluid interferon-gamma and adenosine deaminase in patients with pleural tuberculosis in Qatar. Int J Gen Med 2013;6:13-8.
10. Singh R, Shah NZ, Dar KA, et al. Medical thoracoscopy: Diagnostic role in the management of undiagnosed pleural effusions and its complications. Indian J Chest Dis Allied Sci 2022;64:258-62.
11. Casalini AG, Mori PA, Majori M, et al. Pleural tuberculosis: Medical thoracoscopy greatly increases the diagnostic accuracy. ERJ Open Res 2018;4:1-9.
12. Vásquez-Rodriguez JF, Bravo-Ojeda JS, Erazo LA, et al. Correlation between videothoracoscopy and biopsy in patients with pleural effusion and suspected tuberculosis in a high complexity military hospital. Infectio 2019;23:240-5.
13. MedCalc. Available from: https://www.medcalc.org/calc/diagnostic_test. php [Last accessed on 2023 May 01].
14. Koegelenberg CF, Bolliger CT, Theron J, et al. Direct comparison of the diagnostic yield of ultrasound-assisted Abrams and Tru-Cut needle biopsies for pleural tuberculosis. Thorax 2010;65:857-62.
15. Wang Z, Xu LL, Wu YB, et al. Diagnostic value and safety of medical thoracoscopy in tuberculous pleural effusion. Respir Med 2015;109:1188-92.
16. Kong XL, Zeng HH, Chen Y, et al. The visual diagnosis of tuberculous pleuritis under medical thoracoscopy: A retrospective series of 91 cases. Eur Rev Med Pharmacol Sci 2014;18:1487-95.
17. Kumar S, Agarwal R, Bal A, et al. Utility of adenosine deaminase (ADA), PCR and thoracoscopy in differentiating tuberculous and non-tuberculous pleural effusion complicating chronic kidney disease. Indian J Med Res 2015;141:308-14.
18. Thomas M, Ibrahim WH, Raza T, et al. Diagnostic utility of sago-like nodules on gross thoracoscopic appearance in tuberculous pleural effusion and their correlation with final histo-microbiologic findings. J Tuberc Res 2018;6:270-80.
