Full HTML
Primary duodenal tuberculosis in an 8-year-old child with gastric outlet obstruction
Rashmi Ranjana1 , Saurav Srivastava1 , Digamber Chaubey2 , Sandip Kumar Rahul3
Author Affiliation
1 Resident, Department of Paediatric Surgery, Indira Gandhi Institute of Medical Sciences, Patna, Bihar, India,
2 Assistant Professor, Department of Paediatric Surgery, Indira Gandhi Institute of Medical Sciences, Patna, Bihar, India,
3 Associate Professor, Department of Paediatric Surgery, Indira Gandhi Institute of Medical Sciences, Patna, Bihar, India
Abstract
Primary duodenal tuberculosis (TB) is a rare condition, particularly among children that is easily misdiagnosed even in endemic areas. We present a rare case report of primary duodenal TB in an 8-year-old child who presented with gastric outlet obstruction. Endoscopyguided biopsies were non-conclusive. The patient underwent exploratory laparotomy and during surgery, a 5 cm×5 cm mass was observed in the first part of the duodenum with thickening of the duodenal wall and mesenteric lymphadenopathy. Multiple biopsies were taken from the mass and lymph nodes, and a gastrojejunostomy was performed to relieve the obstruction. Histopathological examination of the duodenal mass and the lymph node samples showed caseating granuloma and giant cells, which are consistent with duodenal TB. The patient received a 6-month regimen of anti-tubercular treatment including 2 months of isoniazid, rifampicin, pyrazinamide, and ethambutol followed by 4 months of isoniazid and rifampicin; he has remained asymptomatic on 3 monthly follow-ups for the past 18 months
DOI: 10.32677/yjm.v2i3.3715
Keywords: Anti-tubercular therapy, Duodenal tuberculosis, Gastric outlet obstruction, Gastrojejunostomy
Pages: 168-170
View: 5
Download: 7
DOI URL: https://doi.org/10.32677/yjm.v2i3.3715
Publish Date: 19-12-2023
Full Text
Abdominal tuberculosis (TB) is one of the most common yet misdiagnosed forms of extrapulmonary TB. It accounts for approximately 13% of extrapulmonary TB cases [1] and 1–4% of total TB cases [1-3]. Abdominal TB may involve the gastrointestinal (GI) system, peritoneum, lymph nodes, and, less frequently, solid organs. Debi et al. found that the ileocecal region (65%), jejunum, and colon (10.8%) were the most commonly affected areas of the GI tract; however, the esophagus (0.2–1%), stomach (0.4–2%), and duodenum (2–2.5%) were also affected [4]. Abdominal TB is rare in children. A study of 5911 Indian children with TB found that 115 (1.9%) had abdominal TB, of which only 21 (0.3%) had GI TB [5]. Although duodenal TB is rare, it has been described in an increasing number of reports in recent years, particularly in adult patients. However, duodenal TB among children is extremely rare, with only a few cases have been reported in the literature [6-9]. We report a case of primary duodenal TB misdiagnosed as gastric outlet obstruction in an 8-year-old male child who had no evidence of pulmonary TB.
CASE REPORT
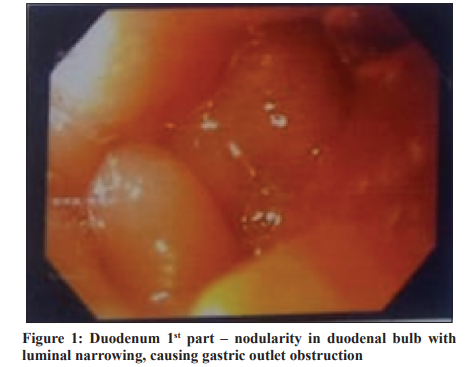
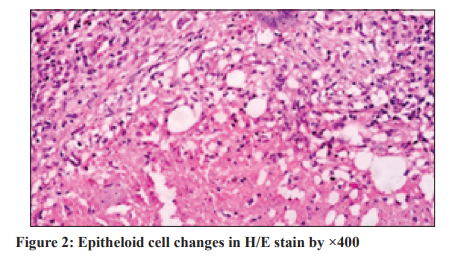
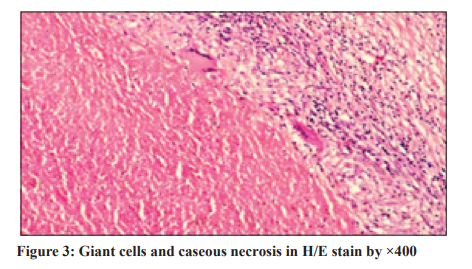
An 8-year-old male child suffered from recurrent non-biliary vomiting and epigastric fullness for 3 weeks, associated with recurrent fever and abdominal pain for the past 2 weeks. The parents noticed that the child had lost appetite and weight over the past 2 months and denied that the patient had a cough or shortness of breath. He had no history of TB and had no exposure to the disease nor any known comorbidities or history of hospitalization. Family history was negative for all relevant diseases, particularly TB. On examination, he weighed 19 kg and was dehydrated, febrile, and tachycardic. There was fullness in the upper abdomen with visible gastric peristalsis; no mass or organomegaly was found on palpation of the abdomen. Systemic examination was unremarkable. A routine blood examination revealed hemoglobin of 9.0 g/dL with normal serum electrolytes. Liver function tests with serum albumin levels were within normal limits. X-ray (chest and abdomen) showed a prominent gastric shadow with a paucity of distal gas. Both lung fields appeared normal. The abdominal ultrasound revealed a distended stomach and a narrowing of the first part of the duodenum. Upper GI endoscopy revealed nodularity in the first part of the duodenum with luminal narrowing through which the endoscope could not be passed further (Fig. 1). Multiple biopsies were taken for Mycobacterium tuberculosis (MTB) polymerase chain reaction test, Acid-fast bacilli smear and culture, and Helicobacter pylori. The patient was admitted to the ward while results were pending. Given these data, the diagnosis of gastric outlet obstruction was suspected and the surgical team was consulted who recommended surgical intervention. The patient underwent exploratory laparotomy and during surgery, a 5 cm×5 cm mass was observed in the first part of the duodenum with thickening of the duodenal wall and mesenteric lymphadenopathy. Peritoneal cavity lavage was performed, and gastrojejunostomy was performed to relieve obstruction. Biopsies were taken from the duodenal mass and mesenteric lymph nodes, and the post-operative recovery was uneventful, and the presenting symptoms resolved. The results of endoscopic biopsies were non-conclusive because the samples were inadequate; however, histopathological examination of the duodenal mass and the lymph node samples showed caseating granuloma and giant cells, which are consistent with duodenal TB (Figs. 2 and 3). The patient received a 6-month regimen of anti-tubercular treatment including 2 months of isoniazid, rifampicin, pyrazinamide, and ethambutol followed by 4 months of isoniazid and rifampicin; he has remained asymptomatic on 3 monthly follow-ups for the past 18 months.
DISCUSSION
Duodenal TB is rare even in endemic areas, with duodenal TB in children being an extremely rare disease. Probable causes for duodenal sparing include high acidity, a paucity of lymphoid tissue, and rapid transit of food in the stomach [9]. Duodenal TB can be primary or secondary. When duodenal TB occurs in the absence of other TB lesions in the body, it is called primary duodenal TB [9], which is caused by Mycobacterium bovis and is usually due to ingestion of contaminated milk from infected cows [10]. Primary duodenal TB is a rare condition, particularly among children. We consider our case as a primary duodenal TB
based on the absence of other TB lesions, especially pulmonary TB. Secondary duodenal TB originates in an extraintestinal primary focus, usually pulmonary, and extends to the intestinal tract either as a consequence of hematogenous dissemination in the form of disseminated TB or following ingestion of contaminated pulmonary secretions. It is usually caused by MTB. Duodenal TB poses a considerable diagnostic challenge due to the lack of specific symptoms and pathognomonic findings. In addition, no single diagnostic method alone is enough to establish the diagnosis. It is most likely misdiagnosed as peptic ulcer disease, inflammatory bowel disease, or malignancy. A high index of suspicion supported by radiological investigation, explorative laparotomy, and histopathological examination of the tissue can only lead to a definitive diagnosis of this rare condition. Endoscopy may not be diagnostic as described in our case, so exploratory laparotomy is necessary in most cases. In our case, despite the patient developed vomiting and epigastric fullness for 3 weeks, the diagnosis of duodenal TB was not immediately considered because the personal and family history was negative for tuberculosis, the patient had no detectable contact with potentially infected individuals, and extraintestinal localization of TB was not suspected at that time of the physical examination or chest X-ray. Our patient required an exploratory laparotomy to visualize the lesion and obtain an adequate biopsy to confirm the diagnosis. Treatment of duodenal TB has two aspects: first, initiation of anti-tubercular medications, and second, relief from obstruction. If the diagnosis is made before surgery, most lesions improve with appropriate anti-tubercular treatment, particularly, when there is partial obstruction. However, complete obstruction will
need surgical intervention (gastrojejunostomy) or endoscopic dilatation [11]. The diagnosis of primary duodenal TB is usually made after surgery and in such cases, gastrojejunostomy is performed to relieve the obstruction, while anti-tuberculosis treatment is initiated after the biopsy results confirm the diagnosis. In our patient, the diagnosis of the gastric outlet obstruction was made intraoperatively, which required a gastrojejunostomy; however, duodenal TB was confirmed histopathologically later, which required the implementation of anti-tubercular therapy
CONCLUSION
A high index of suspicion is required for the diagnosis of duodenal TB because there are no specific clinical, laboratory, imaging, or endoscopic findings. Our case highlights the importance of considering duodenal TB in the differential diagnosis of all pediatric patients in endemic areas who present with chronic abdominal signs and symptoms suggestive of gastric outlet obstruction. 6 months of anti-tubercular therapy is effective in treating duodenal TB, but if the diagnosis is in doubt, surgery may be a better option to confirm the diagnosis and relieve the obstruction.
CONSENT FOR PUBLICATION
Written informed consent was obtained from parents for the publication of this case report and all associated images.
AUTHORS’ CONTRIBUTIONS
All authors contributed to the completion of this work. The final manuscript was read and approved by all authors.
References
1. Chander V, Raina SK, Bhardwaj AK, et al. Clinico-epidemiological profile of extra pulmonary tuberculosis: A report from a high prevalence state of northern India. Public Health Res 2012;2:185-9.
2. Khattab MA, Khan FY, Al Maslamani M, et al. Pulmonary and extra pulmonary tuberculosis in Qatar: A first retrospective population-based study. Adv Infect Dis 2015;5:148-53.
3. Dhali A, Das K, Dhali GK, et al. Abdominal tuberculosis: Clinical profile and outcome. Int J Mycobacteriol 2021;10:414-20.
4. Debi U, Ravisankar V, Prasad KK, et al. Abdominal tuberculosis of the gastrointestinal tract: Revisited. World J Gastroenterol 2014;20:14831-40.
5. Basu S, Ganguly S, Chandra PK, et al. Clinical profile and outcome of abdominal tuberculosis in Indian children. Singapore Med J 2007;48:900-5.
6. Israr S. Duodenal tuberculous stricture with multiple Jejunal and Ileal strictures: A rare cause of intestinal obstruction in a child. J Surg Pak 2022;27:139-42.
7. Karmakar BC, Paria PP, Halder RC, et al. Gastric outlet obstruction: A rare presentation of abdominal tuberculosis. J Evol Med Dent Sci 2015;4:2833-6.
8. Misra S, Kumar P, Mehta S, et al. Tubercular stricture of the duodenum in a child. J Paediatr Child Health 1992;28:338.
9. Upadhyaya VD, Kumar B, Lal R, et al. Primary duodenal tuberculosis presenting as gastric-outlet obstruction: Its diagnosis. Afr J Paediatr Surg 2013;10:83-6.
10. Moirangthem GS, Singh NS, Bhattacharya KN, et al. Gastric outlet obstruction due to duodenal tuberculosis: A case report. Int Surg 2001;86:132-4. 11. Bansal RK, Ranjan P, Kumar M, et al. A case series of gastric outlet obstruction secondary to tuberculosis: New diagnostic and treatment paradigm. J Dig Endosc 2014;5:121-5.
