Full HTML
A rare case of bilateral lung metastasis from renal cell carcinoma 26 years after nephrectomy
Waleed Khaled Kaleem1, Samira Awad Ba Nser2, Rasheed Mohammed Bamekhlah3, Wadeea Saaeed Bin Gouth4, Mohammed Ahmad Bakrmom5
Author Affiliation
1Assitant Profosser of Internal Medicine and Oncology, Oncology Consultant,
2Medical Specialist, Department of Medicine, Ibn-Seena Teaching Hospital, Mukalla, Hadramout, Yemen
3Profosser of Internal Medicine, Senior Medical Consultant, Department of Medicine,
4Profosser, Department of Radiology,
5Medical Student Last Year, Department of Medicine, College of Medicine and Health Sciences, Hadramout University,
Abstract
Renal cell carcinoma (RCC) is a malignant tumor that often metastasizes early. About 33% of RCC patients present with metastatic masses, mostly in the lungs. Our patient was a 66-year-old woman who had a left-sided nephrectomy for RCC 26 years ago. Prior to the current presentation, she sought medical advice for about a year because of her easy fatigability, which was attributed to her normocytic normochromic anemia. Incidentally, a mass was discovered in each lung, which was found histopathologically and immunohistochemically to be a metastasis of RCC. The patient received sunitinib, which is the standard treatment for patients with advanced RCC and metastases without benefit at initial doses and cycles. Consequently, the dose was increased up to four times the initial dose, and by the third cycle, side effects appeared in the form of impaired consciousness up to deep coma, hypertension, hypercarotenemia, pancytopenia, hyponatremia, hypokalemia, and subclinical hypothyroidism. She was taken to the hospital and then sadly passed away.
DOI: 10.32677/yjm.v2i2.4035
Keywords: Lung metastasis, Renal cell carcinoma, Side effects, Sunitinib
Pages: 108-111
View: 3
Download: 7
DOI URL: https://doi.org/10.32677/yjm.v2i2.4035
Publish Date: 28-09-2023
Full Text
Introduction
Renal cell carcinoma (RCC) is a malignant tumor that often metastasizes early to multiple sites, and approximately 33% of RCC patients have metastatic masses at presentation. It commonly metastasizes to the lung parenchyma (45.2%), the skeleton (29.5%), the lymph nodes (20.8%), the liver (20.3%), the adrenal glands (8.9%) and the Brain (8.1%) [1].
Patients with advanced RCC typically receive sunitinib, a multi-targeted tyrosine kinase inhibitor (TKI), which inhibits the vascular endothelial growth factor (VEGF) receptor, platelet-derived growth factor (PDGF), and other tyrosine kinases. It can cause serious adverse events, some of which are thought to be associated with its anti-tumor effects [2].
In this report, we describe a case of RCC in the left kidney which was removed 26 years ago, and metastases were discovered in both lungs a year ago. The patient received sunitinib and experienced serious adverse events and consequently died. Our aim in presenting this case was to demonstrate how RCC metastases can develop even after curative nephrectomy and show how sunitinib can cause serious side effects that require ongoing monitoring.
Case report
A 66-year-old female from a rural area came to our hospital in December 2021 complaining of easy fatigability for many weeks, she was not known to be hypertensive or diabetic, and with no significant medical history rather than a left nephrectomy 26 years ago due to renal cancer, and was not followed by any adjuvant treatment. Clinical examination was unremarkable, however, a chest X-ray revealed an opaque lesion in both lung fields. Computed tomography (CT) of the chest revealed a large heterogeneous speculative mass (5.2 x 5.2 cm) at the level of the left pulmonary lingula and another nodule of similar size (2.2 x 2.2 cm) at the level of the right upper lobe (Figure 1). Pleural effusion and/or mediastinal lymphadenopathy were not found. The radiologist concluded that it was either a primary malignant tumor of the left lung which had metastasized to the right lung or metastasis of an extrapulmonary malignancy. A CT-guided biopsy was consistent with primary clear cell adenocarcinoma with a differential diagnosis of metastatic clear cell carcinoma.
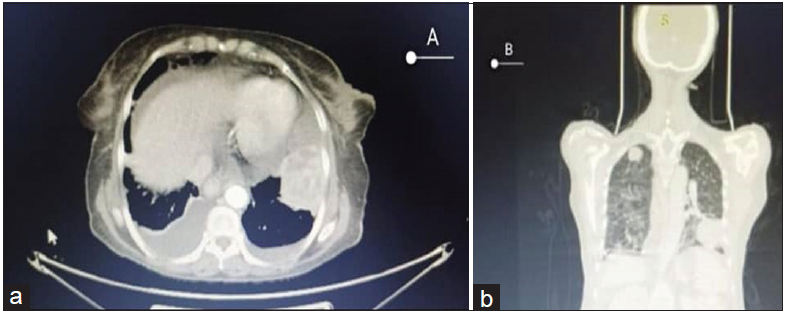
Figure 1: CT images in July 2022 (a) axial section soft-tissue window of lower chest shows solid metastatic mass at the distal left lung, with bilateral mild pleural effusion and ascites. (b) coronal section lung
window shows the basal metastatic left lung mass, and metastatic nodule in the right upper lung

Figure 2: Pallor and yellowish discoloration of the soles of both feet

Figure 3: Pallor and yellowish discoloration of the palms of both hands
The patient was advised to travel abroad for additional management because the country lacked the necessary diagnostic facilities. When the patient was reevaluated abroad in February 2022, the results for -fetoprotein, carcinoembryonic antigen (CEA), CA 19.9, and CA 125 were all within normal ranges. A positron emission tomography (PET) scan revealed an increase in the size of both left and right lung masses (7.2 x 5.8 and 3 x 2 cm, respectively). CT-guided biopsy was repeated and revealed metastatic carcinoma consistent with metastatic clear cell RCC. The immunohistochemical studies reported that the malignant cells were positive for PAX8, CK7, CD10, and Carbonic Anhydrase, proving that the masses were clear cell RCC metastases.
In March 2022, the patient received sunitinib in 6-week cycles. Sunitinib tablet 12.5 mg was administered daily for 4 weeks, followed by 2 weeks off the drug. After three 6-week cycles in July 2022, CT scans of the abdomen and chest showed that the metastatic lesions in both lungs had shrunk slightly. The right kidney and liver were normal, while the patient developed pleural effusion and ascites. She remained treatment-free for three months. In October 2022, CT was repeated and showed the same metastatic masses in both lungs, but the pleural effusion and ascites disappeared (Figure 3). Brain CT was normal.
Sunitinib was re-introduced in a higher dose; 50 mg daily for 4 weeks then one week off and repeated for 3 cycles. Omega 3 capsules and vitamin A rich diet were recommended. In January 2023, while receiving the third cycle of sunitinib 50 mg, the patient presented to our hospital with impaired consciousness, affected memory and mood, and unawareness for the previous 3 weeks, in addition to yellowish discoloration of her skin.
On examination, She was afebrile, not in distress, but was found to be unconscious and had a Glasgow Coma Score (GCS) of 6. She was very pale and had yellowish skin all over her body, more evident on her palms and soles, but the sclera and buccal cavities were clear (Figures 2 and 3)and there were scattered purpura and ecchymosis. Her blood pressure was 150/90 mmHg, the temperature was 36.5°C, and her pulse rate was 96 beats/min regular with average volume. There was scattered coarse crepitation in both lungs, more on the left side. The rest of her examination was unremarkable. Investigations showed pancytopenia, severe hyponatremia, mild hypokalemia, mild hypocalcemia, and high TSH (Table 1).
Table 1: Laboratory test results
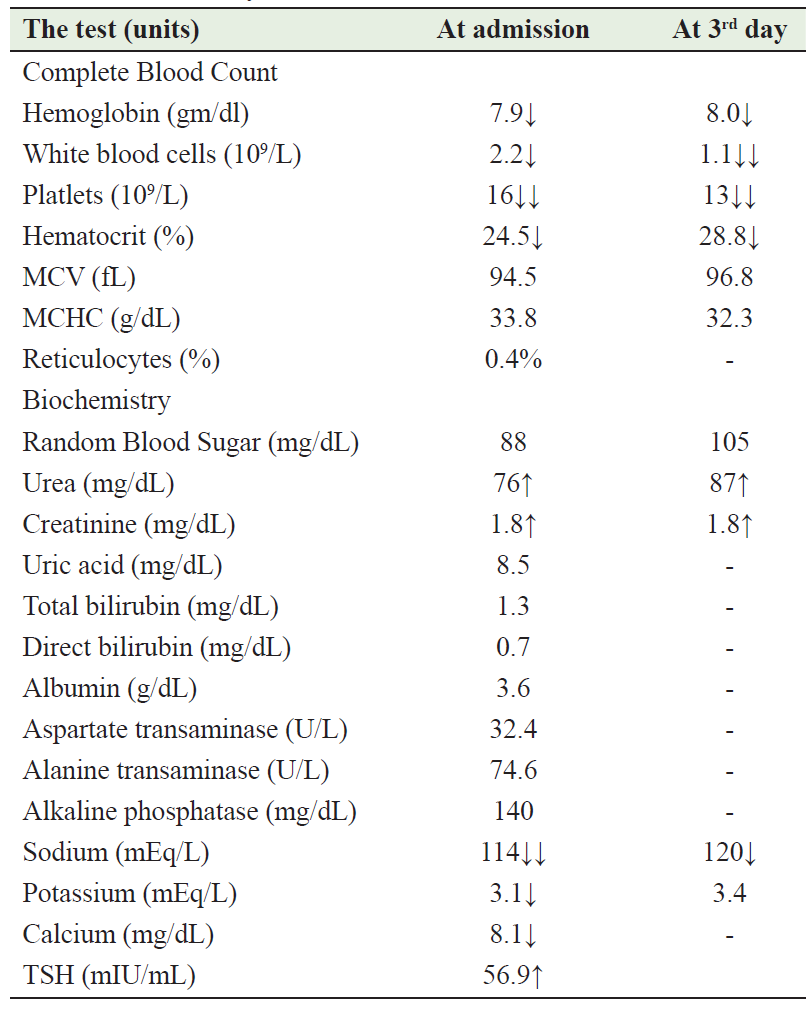
The patient received supportive care as follows: oxygen therapy, 4 units of platelets, normal saline 0.9%, Ringer's lactate, potassium chloride, and calcium gluconate while sunitinib was discontinued. Two days later, the GCS was 4 and the white blood cell count decreased to 1.1 x 109/L, granulocyte stimulating factor (GSF) was introduced, and the high vitamin A diet was discontinued. After 3 days her condition deteriorated and the GCS dropped to 3, then unfortunately the patient passed away.
Discussion
Renal cell carcinoma is a relatively common condition with about 25% of patients having metastatic disease at the time of diagnosis, and an additional 25% developing metachronous metastases, usually within the first five years after nephrectomy. Some authors argue that imaging follow-up may not be cost-effective for low-risk diseases, however, late metastasis from RCC has been reported [3]. The incidence of late recurrence is 11% in patients surviving for 10 years and the longest interval to recurrence reported was 45 years.[4,5] Long-term survival rates of 21-44% have been documented following curative resection for RCC metastases at various sites [6]. Metastases from RCC can be diagnosed in virtually any location, but they commonly spread to the lung [7]. Our case was disease-free 26 years after nephrectomy, but in the last year, bilateral lung metastases were accidentally discovered, which turned out to be clear cell RCC. There are 16 tumor subtypes in the current World Health Organization classification system for RCC. The major histologic variants include clear cell, papillary, chromophobe, and collecting duct tumors, and clear cell carcinoma accounts for 70% to 80% of RCC [8].
The recommended starting dose of sunitinib is 50 mg orally once daily for 28 days followed by a 2-week drug-free period [9]. Regression of RCC after TKI treatment is frequently observed within a few months. Albiges et al reported 36 cases of patients with metastatic RCC who experienced a complete response (CR) following treatment with sorafenib or sunitinib. CR was achieved in a median time of 12.6 months (range 2–28 months) after the start of TKI therapy [10]. In a similar case report, sunitinib administration was started at a dose of 37.5 mg daily for 2 weeks followed by 1 week off. One day after the two-week treatment, the patient was emergently hospitalized for impaired consciousness. Laboratory tests revealed hypoglycemia, hyponatremia, liver dysfunction and thrombocytopenia with disseminated intravascular coagulation (DIC), and the blood concentration of sunitinib was much higher than usual [11]. In the current case report, no serious side effects were identified when sunitinib was started at a low dose (12.5 mg daily), except for mild bilateral pleural effusion and ascites, which resolved three months later when the patient stopped taking the drug. However, since the patient was not improving, he was started on a high dose of sunitinib (50 mg daily), whereupon the patient developed impaired consciousness by the third day of admission, hypertension, hypercarotenemia, pancytopenia, hyponatremia, and subclinical hypothyroidism that have been reported as side effects of sunitinib [12-14]. Sunitinib inhibits the VEGF receptor and other tyrosine kinases, including PDGF and KIT receptors at nanomolar concentrations. TKIs have a unique mechanism of action and exhibit a distinct pattern of toxicities [15,16]. The severe adverse events and dramatic effects of treatment may be attributable to genetic susceptibility to TKI and overexposure to sunitinib [11].
Hypertension is one of the most common side effects of sunitinib that may occur in a range of 10.3-67% of cases [17-19], while the precise mechanism is not clear, hypotheses include pressor stimulation, increased extracellular volume, decreased vascular compliance, increased vascular resistance, endothelial dysfunction and altered nitrous oxide metabolism [20]. All grades of leukopenia, neutropenia, anemia, and/or thrombocytopenia were reported in 60% to 70% of all patients treated with sunitinib [21]. Blood counts usually recover during the 2-week off period or with drug interruptions. Complete blood counts (CBC) should be obtained immediately prior to each cycle in patients with documented cytopenias in prior cycles or at the end of the 4-week dosing period when cytopenias are likely. If neutropenia or thrombocytopenia are present at the time of initiation of a new cycle, dose delay is recommended. If the same toxicity occurs in subsequent cycles, dose reduction in sunitinib should be considered [13]. Hyponatremia occurs in about 10.1% [16,17], The mechanism of hyponatremia with sunitinib is not clearly established, TKIs are mostly associated with a syndrome of appropriate antidiuretic hormone secretion (SIADH)-related mechanism [22]. About 85% of euthyroid patients who received sunitinib for RCC, developed one or more abnormal thyroid function tests [14]. Although hypercarotenemia which affects about 32% of patients receiving sunitinib [16,17]; is a direct side effect of the drug, hypothyroidism was a risk factor as well as the vitamin A intake through foods (eggs, papaya, and tomatoes) and omega 3 capsules.
It is recommended that CT imaging be performed within 1 week after the nephrectomy to rule out any residues, as well as other blood tests such as liver function tests and echocardiography at baseline before starting sunitinib. Thereafter, monitoring is planned every three months to rule out recurrence and/or distant metastasis, for the first year and then every 6 months for 2 years, and finally annually until the completion of 5 years.
Therapeutic drug monitoring of total sunitinib (sunitinib and N-desethyl sunitinib) is used to improve therapeutic efficacy [23] while preventing adverse effects. However, monitoring sunitinib concentration in the blood to prevent late diagnosis of sunitinib toxicity is not performed in our hospital due to a lack of facilities. Instead, we ordered laboratory investigations such as liver function tests, CBC, and thyroid function tests as a baseline and during each cycle.
Conclusion
Metastasis of RCC may appear after a prolonged interval following primary cancer removal by nephrectomy. Therefore, even decades after curative nephrectomy, when clinicians encounter lung masses in patients with a history of RCC, they should still take the possibility of metastasis from RCC into account. Moreover, sunitinib must be used with regular follow-up to recognize any adverse reaction early.
CONSENT FOR PUBLICATION
Verbal informed consent was obtained from the patient’s son for the publication of this case report and all accompanying images
AUTHORS’ CONTRIBUTIONS
All authors contributed to the completion of this work. The final manuscript was read and approved by all authors
References
- Bianchi M, Sun M, Jeldres C, et al. Distribution of metastatic sites in renal cell carcinoma: a population-based analysis. Ann of Oncol. 2012;23(4):973–80.
- Rautiola J, Donskov F, Peltola K, et al. Sunitinib-induced hypertension, neutropaenia and thrombocytopaenia as predictors of good prognosis in patients with metastatic renal cell carcinoma. BJU Int 2016;117:110–7.
- Ljungberg B, Bensalah K, Canfield S, et al. EAU guidelines on renal cell carcinoma: 2014 update. Eur Urol 2015;67:913-24.
- Ljungberg B. The role of metastasectomy in renal cell carcinoma in the era of targeted therapy. Curr Urol Rep 2013;14:19-25.
- Tapper H, Klein H, Rubenstein W, et al. Recurrent renal cell carcinoma after 45 years. Clin Imaging 1997;21:273-5.
- McNichols DW, Segura JW, DeWeerd JH. Renal cell carcinoma: long-term survival and late recurrence. J Urol 1981;126:17-23.
- Featherstone JM, Bass P, Cumming J, et al. Solitary, late metastatic recurrence of renal cell carcinoma: two extraordinary cases. Int J Urol 2006;13:1525-7.
- Correa AF, Rini BI, Linehan WM, et al. Cancers of the genito-urinary tract. In: DeVita Hellman and Rosenberg’s Cancer principles and practice of oncology. 12th. Edition, Volume 4, section 4, Chapter 43. Publisher Wolters Kluwer 2023; pp 729-755.
- Houk BE, Bello CL, Michaelson MD, et al. Exposure-response of sunitinib in metastatic renal cell carcinoma (mRCC): A population pharmacokinetic /pharmacodynamic (PKPD) approach. ASCO Meeting Abstracts. 2007;25(18 suppl):502.
- Albiges L, Oudard S, Negrier S, et al. Complete remission with tyrosine kinase inhibitors in renal cell carcinoma. J Clin Oncol 2012;30:482–7.
- Kazama A, Katagiri A, Ishikawa S, et al. Continuous remission of renal cell carcinoma with tumour thrombus after severe adverse events following short-term treatment with sunitinib. BMJ Case Rep 2017 Aug 28;2017:bcr2017221494
- Larochelle P, Kollmannsberger C, Feldman RD, et al. Hypertension management in patients with renal cell cancer treated with anti-angiogenic agents. Curr. Oncol. 2012;19:202–208.
- Schwandt A, Wood LS, Rini1 B, et al. Management of side effects associated with sunitinib therapy for patients with renal cell carcinoma. OncoTargets and Therapy 2009;2:51–61.
- Rini BI, Tamaskar I, Shaheen P, et al. Hypothyroidism in patients with metastatic renal cell carcinoma treated with sunitinib. J Natl Cancer Inst. 2007;99(1):81–83.
- Rini BI, Sosman JA, Motzer RJ. Therapy targeted at vascular endothelial growth factor in metastatic renal cell carcinoma: biology, clinical results and future development. BJU Int 2005;96:286-90.
- Motzer RJ, Bukowski RM. Targeted therapy for metastatic renal cell carcinoma. Clin Oncol 2006;24:5601-8.
- Motzer RJ, Hutson TE, Tomczak P, et al. Sunitinib versus interferon alfa in metastatic renal-cell carcinoma. N Engl J Med. 2007;356(2):115–124.
- Chu TF, Rupnick MA, Kerkela R, et al. Cardiotoxicity associated with tyrosine kinase inhibitor sunitinib. Lancet 2007;370(9604):2011–2019
- Telli ML, Witteles RM, Fisher GA, et al. Cardiotoxicity associated with the cancer therapeutic agent sunitinib malate. Ann Oncol. 2008;19(9):1613–1618.
- Sica DA. Angiogenesis inhibitors and hypertension: An emerging issue. J Clin Oncol. 2006;24(9):1329–1331.
- Aparicio-Gallego G, Blanco M, Figueroa A, et al. New insights into molecular mechanisms of sunitinib-associated side effects. Mol Cancer Ther 2011; 10: 2215-23.
- Pelletier K, Škrtić M, Kitchlu A. Cancer therapy-induced hyponatremia: A case-illustrated review. Journal of Onco-Nephrology 2021;5(1):70–78.
- Takasaki S, Kikuchi M, Kawasaki Y, et al. Severe toxicity induced by accumulation of active sunitinib metabolite in a Japanese patient with renal cell carcinoma: a case report. J Med Case Reports. 2017;11(1):1-4.
