Full HTML
Recurrence patterns of acute colonic diverticulitis among patients admitted to Benghazi Medical Center, Benghazi, Libya: A retrospective and hospital-based study
Naseralla Juma Elsaadi Suliman1, Marei Omar Ali Jahany2
Author Affiliation
1Consultant General Surgeon, Department of Surgery, Benghazi Medical Center,
2Consultant General Surgeon, Department of Surgery, Hawari General Hospital, Benghazi, Libya
Abstract
Background: The normal pattern of acute colonic diverticulitis is still unknown, and prophylactic surgery after conservative treatment of diverticulitis is a topic of growing debate. The aim of this study was to investigate the patterns and frequency of recurrences and the likelihood of complications in conservatively treated uncomplicated and complicated diverticulitis in our epidemiological setting. Methods: This retrospective study was conducted to investigate 98 inpatients admitted to Benghazi Medical Center with acute colonic diverticulitis between February 2021 and August 2022. Acute diverticulitis discharge summaries were reviewed to identify eligible patients, and their medical records were meticulously reviewed retrospectively to confirm that their clinical presentation was consistent with colonic diverticulitis. Results: A retrospective study of 98 patients with acute colonic diverticulitis found that uncomplicated diverticulitis was associated with younger age, better 2-year survival rates, and more conservative management. Recurrence rates were almost similar between uncomplicated and complicated diverticulitis (23% vs. 25%) and typically occurred within 12 months of the initial attack. Surgical intervention was necessary for patients with perforations, while conservative management was used for other cases. Complications included abscesses in 44% of cases and perforations in 38% of cases. Conclusion: This study found that acute diverticulitis has a low recurrence rate and a limited propensity for progression into complications. It is recommended that elective surgery is used as a preventive measure against recurrences and associated complications. These findings have implications for clinical practice.
DOI: 10.32677/yjm.v2i2.4013
Keywords: Colonic diverticulitis, Conservative treatment, Elective surgical procedures, Natural history, Retrospective studies
Pages: 99-104
View: 3
Download: 5
DOI URL: https://doi.org/10.32677/yjm.v2i2.4013
Publish Date: 28-09-2023
Full Text
INTRODUCTION
Colonic diverticula, which are protruding pouch-like structures in the colon, represent a frequently encountered anatomical abnormality within the gastrointestinal tract. Diverticulosis is a common condition in Western countries, affecting up to two-thirds of the US population by age 80, [1] and it is predominantly left-sided. In contrast, the prevalence rates of diverticulosis in Africa and Asia were less than 0.5%, with right-sided diverticulosis predominating among Southeast Asians [2].
Studies suggest that up to 10–25% of patients with diverticulosis may develop diverticulitis [2–4], with a significant proportion (between 10% and 30%) presenting with symptoms such as sepsis, bowel obstruction, or perforation. fistula formation and bleeding [5-8]. Although the proportion of deaths attributed to diverticular disease has shown a decline over the past 12 years as well as the last two decades, rates of hospital admissions and surgical interventions have witnessed a notable increase of 15%. [9] The prevalence of the perforated sigmoid diverticular disease has increased in developed nations. [10,11] In light of the recent data on the natural progression of diverticulitis, which suggest that recurrence rates are relatively low [12], the rising prevalence of diverticulitis and the burden associated with it have sparked intense scientific discussion about the best method for treating patients with recurrent episodes, particularly those with complicated forms of the disease [13,14]. Due to the lack of articles on this topic in our country, it becomes difficult to cite the results of previous studies. The aim of this study was therefore to investigate the patterns and frequency of recurrences and the likelihood of complications in conservatively treated uncomplicated and complicated diverticulitis in our epidemiological setting.
METHODS
Study design setting and population
This retrospective study was conducted to investigate 98 inpatients admitted to Benghazi Medical Center with acute colonic diverticulitis between February 2021 and August 2022. Acute diverticulitis discharge summaries were reviewed to identify eligible patients, and their medical records were meticulously reviewed retrospectively to confirm that their clinical presentation was consistent with colonic diverticulitis. Classification systems have been developed for complicated diverticulitis; We use the Hinchey classification [13,15,16].
Hinchey’s classification of complicated colonic diverticulitis.
- Grade I Mesenteric or pericolic abscess
- Grade II Pelvic abscess
- Grade III Purulent peritonitis
- Grade IV Fecal peritonitis
Symptoms such as localized left iliac fossa abdominal pain, fever, or a raised white blood cell count were considered, and the presence of computed tomography (CT) evidence of acute diverticulitis was also taken into account. [17] Various patient details were recorded, including demographic data, management plan, readmission, complications, and subsequent surgery.
Exclusion criteria
Diverticular disease patients who have previously undergone surgery, those with a history of inflammatory bowel disease, those who have had radiation therapy to the abdomen or pelvis, those who have a known bleeding disorder, those who are taking anticoagulant therapy, and pregnant women are among were excluded from this study.
Statistical analysis
The gathered information was entered and analyzed using SPSS software (v 20.0; IBM Corp, Armonk, NY, USA). Descriptive statistics of qualitative and quantitative data were expressed in the form of frequency along with percentage and mean± Standard Deviation (SD). Fisher exact test or Chi Square test will be used when appropriate to compare between two groups. The level of statistical significance was set at 5% and the difference was considered significant if p<0.05.
Ethical Approval Statement
This study received ethical approval from the Libyan Research Ethics Committee before commencement. The study was conducted in accordance with the ethical principles set out in the Declaration of Helsinki and the guidelines of the International Conference on Harmonization and all data recorded were kept confidential.
RESULTS
Demographic characteristics of patients
A total of 98 patients with acute colonic diverticulitis were enrolled in the study. Their mean age was 51.8+12.9 years (range 28-87 years). Females constitute 58 % of the study population while 42% of the patients were males. The disease was uncomplicated in 67% of the patients, while 76% of the study population were on conservative treatment (Table 1). However, patients with uncomplicated diverticulitis were observed to be younger and were more likely to be managed conservatively compared to those with complicated diseases. (Table 2).
Table 1: Patient demographic characteristics and management outcomes

Table 2: Age, treatment, recurrence, and 2-year survival rates among uncomplicated and complicated diverticulitis patients

Recurrence pattern of acute diverticulitis
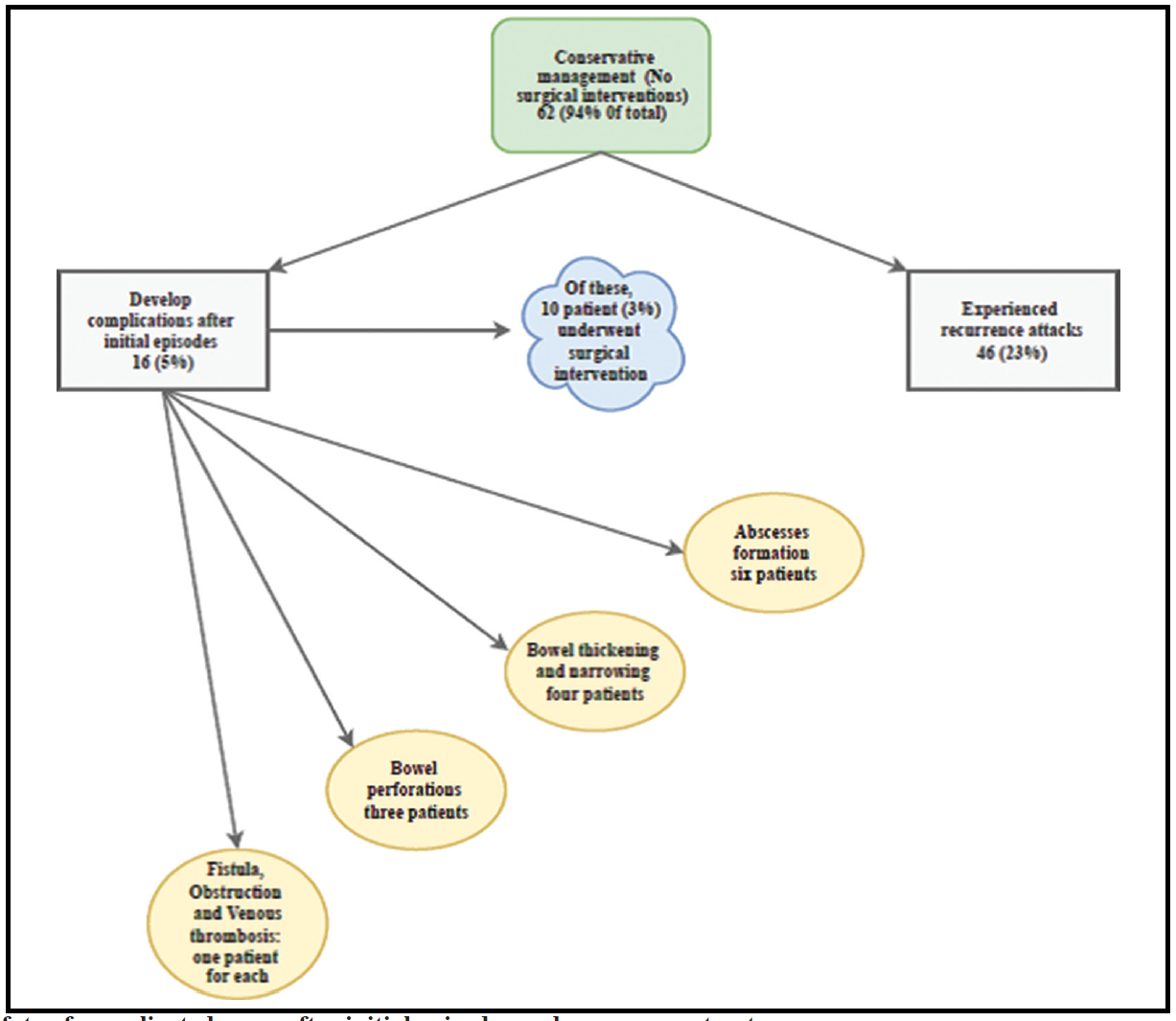
Of those with uncomplicated diseases, 62 (94%) were managed without surgery, with 46 (23%) of these experiencing recurrence bouts, and 16 (5%) developed complicated disease after their initial episode of diverticulitis (Flowchart 1). The complications observed in these patients included abscess formation in six cases, scarring in four cases, perforation in three cases, and a combination of complications including fistula, obstruction, and mesenteric vein thrombosis in one case. Among these 16 patients who developed complications, 10 patients (3%) required surgical interventions, including the formation of a stoma in three cases (Flowchart 2). Notably, no mortality was recorded in this patient cohort. Surgery was primarily performed in 4 (6%) patients with diagnostic uncertainty, with sigmoid diverticulitis being the most common finding (Hinchey 3 or 4 peritonitis), 2 of these underwent a laparoscopic operation, one had laparotomy without resection and one had laparotomy with bowel resection,

Flowchart 1: Uncomplicated acute colonic diverticulitis with conservative management
Flowchart 2: The fate of complicated cases after initial episodes and management outcomes
Complications of acute diverticulitis and study outcomes
The present study again investigated the outcomes of a cohort of 32 patients diagnosed with complicated diverticulitis, which accounted for approximately 33% of the total study population. Abscesses were the most prevalent among the observed complications, occurring in 44% of cases (n=14), followed by perforations in 38% (n=12). Other complications included obstruction (6%, n=2), enterocutaneous fistula (6%, n=2), and bowel thickening (6%, n=2). Surgical intervention was deemed necessary for patients with perforations (75%, n=9) due to the presence of peritonitis upon presentation, while the remaining cases were managed conservatively. Of the 14 patients with abscesses, 50% (n=7) achieved successful resolution without the need for surgery. Four patients underwent percutaneous abscess drainage, two experienced recurrences, and one required laparotomy (Flowchart 3). There were no statistically significant differences between uncomplicated and complicated diverticulitis regarding recurrence and 2-year survival rates (Table 2).
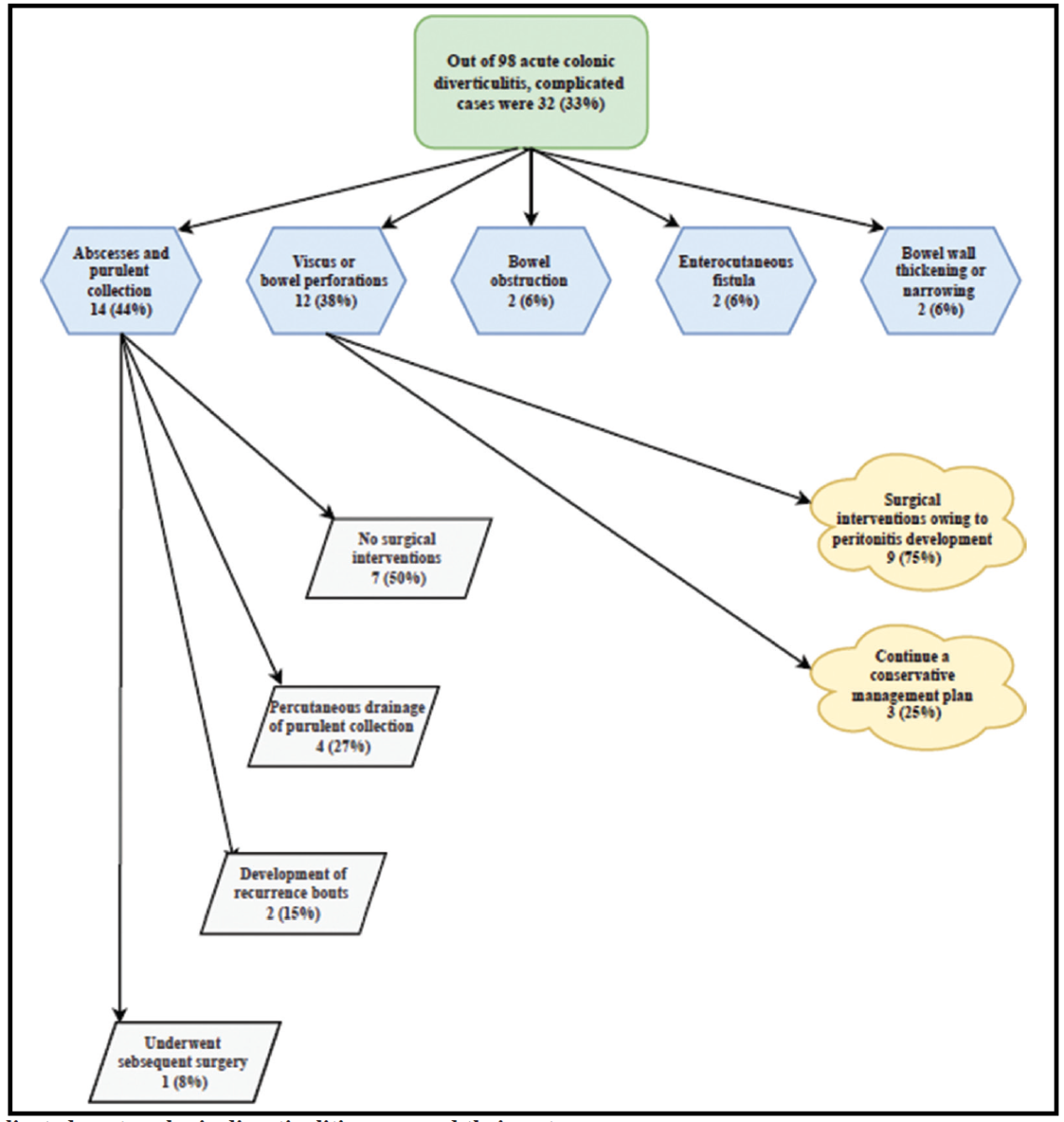
Flowchart 3: Complicated acute colonic diverticulitis cases and their outcomes
DISCUSSION
This study provides average-term follow-up data on a large cohort of patients with colonic diverticulitis, which is consistent with previous studies. The recurrence rate observed in the study is almost similar to previous studies published in 1970 and supports the notion that most patients with diverticulitis will not experience recurrent bouts. The study also found that the demographics of the patients in the cohort nearly resembled previously published data [1,17,18], with most patients (67%) having uncomplicated diverticulitis that was managed conservatively (94%). Therefore, this study adds to the understanding of the natural history of diverticulitis and reinforces the need for the cautious use of elective surgery to prevent a recurrence.
As noted, this study found that 23% of patients with conservatively treated uncomplicated diverticulitis experienced recurrence attacks, but most had just one recurrence, 37 (19%), and only 9 (4%) had more than two episodes. These findings are in line with earlier studies that reported a 7–25% recurrence rate [19,20]. Elective colectomy is often performed to prevent recurrent acute disease, [21] but the current study suggest that most patients will not experience recurrence, and therefore surgery to prevent recurrence should only be used in selected cases.
A previous study suggests that recurrent episodes of diverticulitis usually occur early, within the first few months after the initial episode, and then decrease to a low but persistent rate after 12 months. The early recurrence may be due to the failure of the initial episode to resolve rather than a de novo recurrence. The study also questions the assumption that the risk of recurrence increases with each episode of diverticulitis, as the proportion of patients suffering further recurrence did not significantly increase with each recurrent episode. [22] However, a larger population-based study demonstrated a significant increase in the risk of further recurrence with each episode (29.3 versus 13.3 percent). [23] Therefore, the decision to offer elective colectomy should consider not only the natural history of conservatively managed diverticulitis but also the operative morbidity and mortality associated with elective colectomy and its effectiveness in preventing recurrence. [2,24]
Previous observational studies have shown that the rate of recurrence of diverticulitis after elective colectomy is between 5%-11%, [25] with generally low mortality rates of 0.8% in large reviews. However, elective surgery for diverticular resection has been associated with a higher mortality risk of up to 4%. [23,26] Some authors have proposed models for determining the optimal timing of colectomy after acute diverticulitis, with one study suggesting operating after three episodes is the most cost-effective and yields greater quality-adjusted life years [27]. Another study showed that operating electively after additional episodes of diverticulitis yielded fewer deaths and colostomies, more quality-adjusted life years, and was less costly than operating earlier. [28] The present study's natural history findings support the proposal that the number of attacks of diverticulitis alone should not be used as an indication for surgery, and the decision to recommend a sigmoid colectomy should be made on a case-by-case basis.
The need for elective surgery for diverticulitis is often justified by preventing serious complications and recurrence. However, this study found that surgery was necessary in only 4 (6%) of the 66 patients with the uncomplicated disease (67%) and there was no significant difference in survival between patients with and without recurrence. Therefore, the data do not support the need for elective surgery after acute diverticulitis to prevent serious complications.
The previous assumption that young patients with diverticulitis have a more severe course and require early surgery after a single attack is based on misclassification and selection bias. Young patients are more likely to undergo surgery to clarify an uncertain diagnosis and unexpected, uncomplicated cases of diverticulitis are often discovered during surgery, with most cases tending to be severe or complicated at this point. However, Vennix et al. concluded in their systematic review that age is not necessarily a predictor of disease severity or recurrence, but that CT scan findings are a more accurate indicator [29].
CT is the most reliable diagnostic tool for diverticulitis, surpassing the accuracy of bioclinical parameters. However, a recent study revealed no significant difference in recurrence rates between patients diagnosed with CT and those diagnosed with bioclinical parameters. [30] Although CT scanning has a high sensitivity (up to 98%) and specificity (70–100%), it can still miss some cases (false negatives) and occasionally produce false-positive results. Although CT is preferred, clinicians should use caution when interpreting its results and take bioclinical factors into account when diagnosing diverticulitis. There are several limitations to this study that must be acknowledged. First, it was a retrospective analysis with a short follow-up period of patients. Therefore, we were unable to obtain additional information on recurrence rates. Second, the study has limitations related to the use of readmission data to estimate recurrence, as these may not capture all cases of recurrent diverticulitis. Third, although CT is considered the benchmark diagnostic method for diverticulitis, it has its limitations and can produce false positive results. This implies that some cases identified as diverticulitis based on CT scans may not be truly positive cases, which may impact the accuracy of the study results. Fourth, this was a hospital-based study and therefore we may not be able to generalize our results to the general population. Fifth, the sample size was relatively small.
Despite these limitations, the study provides valuable insights into the natural history of complicated diverticular disease and suggests that the decision to perform elective surgery after acute diverticulitis should be made on a case-by-case basis. Researchers and clinicians can gain a deeper understanding of the study's findings and their implications for clinical decision-making in the treatment of acute colonic diverticulitis by acknowledging these limitations.
CONCLUSION
In conclusion, this study found that acute diverticulitis has a low recurrence rate and a limited propensity for progression into complications. When recurrences occur early and suggest failure of initial treatment, the results highlight the importance of early identification and treatment of risk factors to prevent disease progression and improve patient outcomes. Moreover, they emphasize the importance of considering age and gender factors in the management of acute colonic diverticulitis, as well as the predominance of uncomplicated cases and the preference for conservative treatment approaches. Future studies with larger sample sizes and longer follow-up periods may provide more insight into the long-term patterns and predictors of disease recurrence in acute diverticulitis. These results may have implications for clinical practice guidelines and could inform personalized treatment plans for patients with this condition.
.ACKNOWLEDGEMENTS
The authors acknowledge the contributions of postgraduate students and colleagues who collect data and reviewed the article, as well as the staff of the IT and medical registry archives.
AUTHORS’ CONTRIBUTION
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, data collection, data analysis and interpretation, or all these areas; also, they took part in drafting, revising, or critically reviewing the article; and gave final approval of the version to be published
References
- Strate LL, Modi R, Cohen E, et al. Diverticular disease as a chronic illness: evolving epidemiologic and clinical insights. Am J Gastroenterol. 2012 Oct;107(10):1486-93.
- Weizman AV, Nguyen GC. Diverticular disease: epidemiology and management. Canadian Journal of Gastroenterology. 2011;25(7):385-9.
- Bharucha AE, Parthasarathy G, Ditah I, et al. Temporal trends in the incidence and natural history of diverticulitis: a population-based study. Am J Gastroenterol. 2015;110(11):1589.
- Stollman N, Smalley W, Hirano I, et al. American Gastroenterological Association Institute guideline on the management of acute diverticulitis. Gastroenterology. 2015;149(7):1944-9.
- Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143(5):1179-87.
- Feingold D, Steele SR, Lee S, et al. Practice parameters for the treatment of sigmoid diverticulitis. Diseases of the Colon & Rectum. 2014;57(3):284-94.
- Peery AF, Sandler RS, Ahnen DJ, et al. Constipation and a low-fiber diet are not associated with diverticulosis. Clinical gastroenterology and hepatology. 2013;11(12):1622-7.
- Humes DJ, West J. Role of acute diverticulitis in the development of complicated colonic diverticular disease and 1-year mortality after diagnosis in the UK: population-based cohort study. Gut. 2012;61(1):95-100.
- Mosadeghi S, Bhuket T, Stollman N. Diverticular disease: evolving concepts in classification, presentation, and management. Current opinion in gastroenterology. 2015;31(1):50-5.
- Sallinen VJ, Mentula PJ, Leppäniemi AK. Nonoperative management of perforated diverticulitis with extraluminal air is safe and effective in selected patients. Diseases of the colon & rectum. 2014;57(7):875-81.
- Tursi A, Elisei W, Franceschi M, et al. The prevalence of symptomatic uncomplicated diverticular disease could be lower than expected: a single-center colonoscopy-based cohort study. European Journal of Gastroenterology & Hepatology. 2021;33(1S):e478-83.
- Kruis W, Germer CT, Leifeld L. Diverticular disease: guidelines of the german society for gastroenterology, digestive and metabolic diseases and the german society for general and visceral surgery. Digestion. 2014;90(3):190-207.
- Binda GA, Cuomo R, Laghi A, et al. Practice parameters for the treatment of colonic diverticular disease: Italian Society of Colon and Rectal Surgery (SICCR) guidelines. Techniques in coloproctology. 2015;19:615-26.
- Regenbogen SE, Hardiman KM, Hendren S, et al. Surgery for diverticulitis in the 21st century: a systematic review. JAMA surgery. 2014;149(3):292-303.
- Sartelli M, Weber DG, Kluger Y, et al. 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World Journal of Emergency Surgery. 2020;15(1):1-8.
- Klarenbeek BR, Samuels M, van der Wal MA, et al. Indications for elective sigmoid resection in diverticular disease. Annals of surgery. 2010;251(4):670-4.
- Shahedi K, Fuller G, Bolus R, et al. Long-term risk of acute diverticulitis among patients with incidental diverticulosis found during colonoscopy. Clinical gastroenterology and hepatology. 2013;11(12):1609-13.
- Hjern F, Wolk A, Håkansson N. Obesity, physical inactivity, and colonic diverticular disease requiring hospitalization in women: a prospective cohort study. Official journal of the American College of Gastroenterology| ACG. 2012;107(2):296-302.
- Søreide K, Boermeester MA, Humes DJ, et al. Acute colonic diverticulitis: modern understanding of pathomechanisms, risk factors, disease burden and severity. Scandinavian Journal of Gastroenterology. 2016;51(12):1416-22.
- Sartelli M, Catena F, Ansaloni L, et al. WSES Guidelines for the management of acute left sided colonic diverticulitis in the emergency setting. World journal of emergency surgery. 2016;11(1):1-5.
- Salem L, Flum DR. Primary anastomosis or Hartmann’s procedure for patients with diverticular peritonitis? A systematic review. Diseases of the colon & rectum. 2004; 47:1953-64.
- Vennix S, Musters GD, Mulder IM, et al. Laparoscopic peritoneal lavage or sigmoidectomy for perforated diverticulitis with purulent peritonitis: a multicentre, parallel-group, randomised, open-label trial. The Lancet. 2015;386(10000):1269-77.
- Andeweg CS, Mulder IM, Felt-Bersma RJ, et al. Guidelines of diagnostics and treatment of acute left-sided colonic diverticulitis. Digestive surgery. 2014;30(4-6):278-92.
- Angenete E, Thornell A, Burcharth J, et al. Laparoscopic lavage is feasible and safe for the treatment of perforated diverticulitis with purulent peritonitis: the first results from the randomized controlled trial DILALA. Annals of surgery. 2016;263(1):117.
- Biondo S, Golda T, Kreisler E, et al. Outpatient versus hospitalization management for uncomplicated diverticulitis: a prospective, multicenter randomized clinical trial (DIVER Trial).
- Angenete E, Bock D, Rosenberg Jet al. Laparoscopic lavage is superior to colon resection for perforated purulent diverticulitis—a meta-analysis. International journal of colorectal disease. 2017;32:163-9.
- Margolin DA. Timing of elective surgery for diverticular disease. Clin Colon Rectal Surg. 2009 Aug;22(3):169-72.
- Salem L, Veenstra DL, Sullivan SD, et al. The timing of elective colectomy in diverticulitis: a decision analysis. Journal of the American College of Surgeons. 2004;199(6):904-12.
- Vennix S, Morton DG, Hahnloser D, et al. Research Committee of the European Society of Coloproctocology. Systematic review of evidence and consensus on diverticulitis: an analysis of national and international guidelines. Colorectal Disease. 2014;16(11):866-78.
- Hall JF, Roberts PL, Ricciardi R, et al. Long-term follow-up after an initial episode of diverticulitis: what are the predictors of recurrence?. Diseases of the colon & rectum. 2011;54(3):283-8.
