Full HTML
Evidence for immunothrombosis according to some markers of thromboinflammation in women with unexplained recurrent reproductive failures
Alphonsus Ogbonna Ogbuabor
Author Affiliation
Hematologist, Department of Medical Laboratory Sciences, Faculty of Basic Medical Sciences, College of Medicine, Enugu State University of Science and Technology, Enugu State, Nigeria
Abstract
Background: Unexplained recurrent reproductive failures (URRF) is a term that describes three different conditions of infertility namely, unexplained infertility (UI), Unexplained recurrent miscarriage (URM) and unexplained recurrent implantation failures (URIF). It is a global reproductive health problem. The aim of the present study was to compare some systemic markers of thromboinflammation in women with unexplained recurrent reproductive failures to controls. Methods: This was a case-control study involving 70 subjects (35 cases of URRF and 35 healthy control women). The systemic cellular markers of immunothrombosis involving the Platelet Count (PLT), Mean Platelet Volume (MPV), Platelet Distribution Width (PDW), Plateletcrit (PCT), Neutrophil to Lymphocyte Ratio (NLR) and the Platelet to Lymphocyte Ratio (PLR) were determine using the Sysmex XN-10 Automated Hematology Analyzer, Sysmex Corporations Japan. Data was analyzed using One Way Analysis of Variance in GraphPad Prism version 8.0 (Graphpad Software, San Diego, CA, USA) and presented as mean + SD. Statistical significance was defined as p<0.05. Result: The MPV, PDW and NLR were significantly increased (p = 0.002, 0.007 and 0.028) respectively in the subjects with Unexplained Recurrent Reproductive Failures compared to the healthy controls. Conclusion: This finding supports an evidence for immunothrombosis in patients with Unexplained Recurrent Reproductive Failures.
DOI: 10.32677/yjm.v2i2.4241
Keywords: Low-grade chronic inflammation, Low-grade intravascular coagulation, Unexplained infertility, Unexplained recurrent implantation failures, Unexplained recurrent miscarriage
Pages: 95-98
View: 3
Download: 5
DOI URL: https://doi.org/10.32677/yjm.v2i2.4241
Publish Date: 28-09-2023
Full Text
INTRODUCTION
Unexplained Recurrent Reproductive Failures (URRF) is a clinical term that broadly defines the inability to conceive or the incapacity to maintain pregnancy to term in a healthy woman during her reproductive age (1-3). It comprises three different clinical conditions of infertility namely repeated pre-implantation failures that occurs in a natural reproductive cycle (Unexplained Infertility, UI) repeated implantation failures that occur in assisted reproductive therapy cycles (Unexplained Recurrent Implantation Failures, URIF) and repeated post-implantation failures that occur in a natural reproductive cycle (Unexplained Recurrent Miscarriages, URM, (4,5). It accounts for 80% of all cases of reproductive failures and 50% of all cases of infertility (6,7). The etiology of Unexplained Recurrent Reproductive Failures is considered a maternal disease involving failure of alloimmune crosstalk between the mother and the conceptus due to an underlying chronic inflammation which results in a thrombotic state. Immunothrombosis describes the intricate crosstalk between Low Grade Chronic Inflammation and Low Grade Intravascular Coagulation. Research is currently geared towards understanding the role of immunothrombosis in maternal predisposition to microvascular failure and non specific inflammatory reaction against the deposited sperm cells, the newly formed zygote, the implanting embryo or the fetal allograft (8,9). The Platelet Count (PLT), Mean Platelet Volume (MPV), Platelet Distribution Width (PDW), Plateletcrit (PCT) Neutrophil to Lymphocyte Ratio (NLR) and the Platelet to Lymphocyte Ratio (PLR) are efficient systemic cellular markers of Low Grade Chronic Inflammation and Low Grade Intravascular Coagulation (immunothrombosis) (10). There is currently a paucity of data on the levels of these parameters in Nigerian women with Unexplained Recurrent Reproductive Failures. The present study was therefore conducted to determine the levels of PLT, MPV, PDW, PCT, NLR and PLR determined from the routine complete blood count in women with different categories of unexplained recurrent reproductive failures compared to healthy controls.
MATERIALS AND METHODS
Study Design, population and setting
This was a case-control study involving 70 subjects (35 women with unexplained recurrent reproductive failures and 35 healthy controls).The 35 cases of Unexplained Recurrent Reproductive Failures comprised 12 women with Unexplained Infertility (UI), 13 women with Unexplained Recurrent Miscarriage (URM) and 10 women with Unexplained Recurrent Implantation Failures (URIF). This study was carried out at the Enugu State University of Science and Technology Teaching Hospital between November 2022 to May 2023.
Subjects Exclusion Criteria
- Women diagnosed with hematological disorders, hormonal disorders, infectious disease, thyroid disorders, autoimmune disorders and systemic disorders such as diabetes mellitus.
- Women with existing or previous ultrasonographic evidence of uterine malformations.
- Women with history of smoking, contraception, alcohol or substance abuse.
- Rhesus negative women with rhesus positive partners.
- Women with Body Mass Index (BMI) > 24.99kg/m2 and/or age > 40 years.
Subjects Inclusion Criteria
- A total of 35 apparently healthy women with good obstetrics and gynecology history who had recorded normal live births were chosen as the controls.
- A total of 12 women who failed to achieve clinical pregnancy after at least 2 years of unprotected sexual intercourse who has been diagnosed with normal results of fertility with normal partners were chosen as the cases for unexplained infertility (UI).
- A total of 13 women with a history of > 3 repeated miscarriages were chosen as the cases for unexplained recurrent miscarriage (URM).
- A total of 10 women who failed to achieve clinical pregnancy after a transfer of at least 3 good quality embryos in at least 3 assisted reproduction therapy cycles were chosen as the cases for unexplained recurrent implantation failures (URIF).
Sample Size
The sample size for the study was calculated using the Leslie Kish formula.11
n = Zα2 PQ
D2
Where
n = minimum required sample size when the population of study is greater than
10,000.
Zα = the α level of the coefficient interval or the standard normal deviate set at 1.96
corresponding to 95% confidence interval.
P = the proportion in the target population estimated to have unexplained recurrent
reproductive failures (12).
D = the width of the confidence interval set at 0.05.
Q = (1-p); the proportion of non-occurrence.
Substituting
n = 1.96 x 1.96 x 0.58(1-.0.58)
0.05 x 0.05 = 374
But an estimate of 26 women with unexplained recurrent reproductive failures attended the clinics in the last one year. Since this is less than 10,000 the sample size was adjusted using the formula.
nf = n + (n)
1 N
Where
nf = calculated sample size
n = minimum sample size
N = population size
Substituting
nf = 1 + 347
26 = 24
Considering anticipated response rate of 90%, the sample size was further adjusted to accommodate attrition using the formula
Ns = nf/r
Where
Ns = adjusted sample size for response rate
Nf = calculated sample size
Substituting
Ns = 24 = 27
0.9
Sample Collection and preparation
Ten milliliters (10ml) of venous blood samples were collected from each subject following standard venipuncture techniques. Five milliliters were dispensed into Ethylene Diamine Tetra Acetic (EDTA) bottles for the determination of the Platelet count (PLT), Mean Platelet Volume (MPV), Platelet Distribution Width (PDW), Platelecrit (PCT) and Neutrophil to Lymphocyte Ratio (NLR).
Determination of the Parameters
The hematological parameters involving the Platelet Count (PLT), Mean Platelet Volume (MPV), Platelet Distribution Width (PDW), Plateletcrit (PCT), Neutrophil to Lymphocyte Ratio (NLR), and the Platelet to Lymphocyte Ratio (PLR) were determined using the Sysmex XN-10 Automated Hematology Analyzer, Sysmex Corporations, Japan. The sample were aspirated by letting the machine sample probe into the blood sample bottle and then pressing the probe button. Approximately 20ml of blood was aspirated by the machine. The values of the PLT, MPV, PDW, PCT were displayed in the screen after 30 seconds as part of the full blood count result. A printout copy of results was released on the thermal printing paper while the values of the NLR and PLR were calculated manually from the values of the neutrophils, lymphocytes and platelet counts.
Statistical Analysis
Data was analyzed using One Way Analysis of Variance in GraphPad Prism version 8.0 (San Diego, California, USA) and presented as mean + SD with statistical significance set at p<0.05
Ethical Consideration
Ethical clearance was obtained from the Hospital Management Ethical Committee (ESUT/C-MAC/Vol 4/43) and informed consent from the subjects.
RESULTS
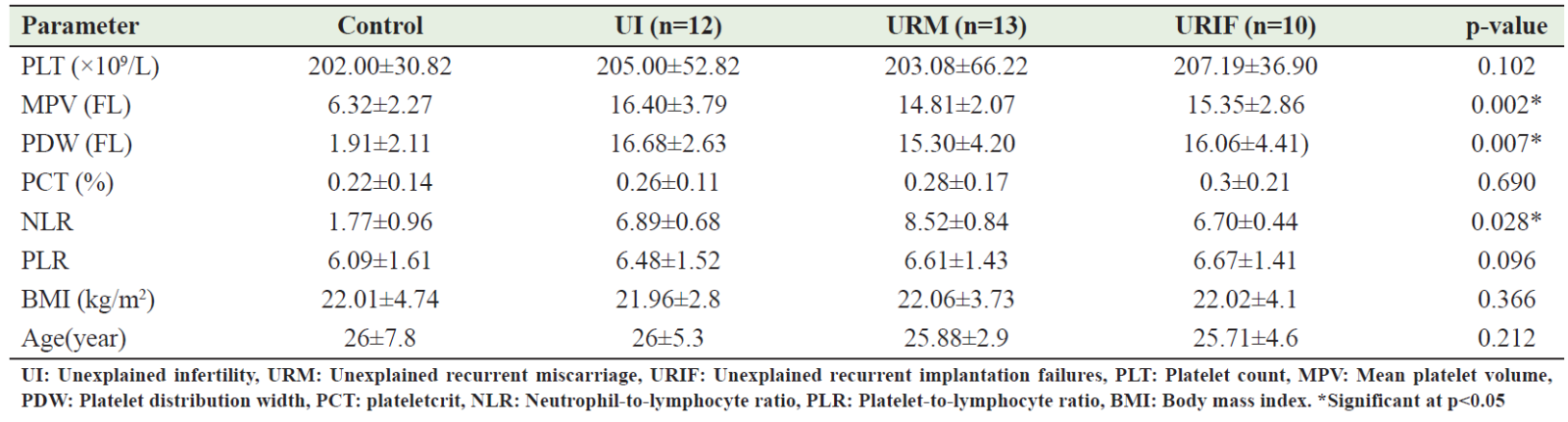
The results of the demographic information showed no significant differences for the Age and BMI (p=0.212, 0.366 respectively) between the subjects and controls (Table 1) .The MPV, PDW and NLR were significantly increased (p = 0.002, 0.007 and 0.028) respectively in the women with different categories of unexplained recurrent reproductive failures (Unexplained infertility, unexplained recurrent miscarriage and unexplained recurrent implantation failures) compared to the control (Table 1).We also observed a non significant increase in the PLT, PCT and PLR (p = 0.102, 0.690 and 0.096) respectively for the women with different categories of unexplained recurrent reproductive failures compared to the control (Table 1).
Table 1: Markers of immunothrombosis in women with different categories of unexplained recurrent reproductive failures and healthy controls
DISCUSSION
Unexplained Recurrent Reproductive Failures (URRF) occurs both in the natural and assisted cycles of reproduction. In a natural cycle of reproduction, it is estimated that 60% of conceptions are lost in healthy women from fertilization to birth. On the other hand, it is estimated that the maximum chance of pregnancy per cycle in assisted reproductive therapy is as low as 20% in healthy couples (13). Although it has been suggested that the coagulation cascade and inflammation pathways are closely linked together, the data on the role of low grade intravascular coagulation and low grade chronic inflammation in unexplained recurrent reproductive failures is still a puzzling issue (14). Low grade chronic inflammation and low grade intravascular coagulation are both pathological states lacking overt inflammation and coagulation but are characterized by continuous and unresolved activation of inflammation and coagulation respectively (15). The observed increase in the platelet count (PLT), plateletcrit (PCT) as well as the platelet lymphocyte (PLR) ratio in the women with different categories of unexplained recurrent reproductive failures and a significant increase in the platelet distribution width (PDW), mean platelet volume (MPV) and the neutrophil lymphocyte ratio (NLR) are suggestive of the occurrence of both low grade chronic inflammation and low grade intravascular coagulation in these patients. This could trigger an adverse maternal immune response to the deposited sperm cell, zygote, implanting embryo and/or the fetal allograft (16). During alloimmune response, inflammatory mediators particularly proinflammatory cells induce the activation of coagulation proteins, cause a decrease in natural anticoagulation proteins and a decrease in fibrinolytic activity resulting in a prothrombotic state (16). The outcome of this is a failure of microvascular circulation which may result to failure of implantation, placental abruption, fetal growth restriction and spontaneous abortion (17). Some studies have reported that the in vitro fertilization program may induce coagulopathy in subjects which may affect the process of implantation during assisted reproductive therapy cycles (17,18). This has been suggested to be intrinsic or due to the hormone treatment preceding the in vitro fertilization program (14). This may actually account for the increased concentrations of the markers of low grade chronic inflammation and low grade intravascular coagulation particularly the PDW, MPV and NLR recorded for our subjects with unexplained recurrent implantation failures (URIF). The significant increase in the PDW, MPV and NLR recorded for subjects with URRF is not consistent with the findings of some studies which reported no significant differences in these parameters in subjects with recurrent pregnancy loss and recurrent implantation failures compared to healthy controls (19,20). However, our finding is consistent with the findings of another study which recorded significant increase in these parameters in Yemeni subjects with recurrent pregnancy loss compared to healthy controls (10). A combined increase in the PDW, MPV and NLR as recorded in the present study has been identified as an efficient marker of nonspecific systemic inflammation and coagulation activation (10,21). Thus, a combined effect of low grade chronic inflammation and low grade intravascular coagulation may be a common underlying mechanism responsible for the different conditions of unexplained recurrent reproductive failures namely Unexplained infertility, unexplained recurrent miscarriage and unexplained recurrent implantation failures.
Small sample size and the fact that the study was conducted in a single center are its limitations, which may have an impact on the validity of the data and the applicability of the findings.
Conclusion
The significant increase in the NLR, MPV and PLR in the subjects with different categories of unexplained recurrent reproductive failures in the present study suggests a role for immunothrombosis in patients with unexplained recurrent reproductive failures however; further randomized prospective studies are required to support the present findings. The combination of subjects from the three different categories of unexplained recurrent reproductive failures namely unexplained recurrent miscarriage (URM) unexplained infertility (UI) and unexplained recurrent implantation failures (URIF) could be considered a strength in the present study as there are limited studies that has considered these three cases in a single study in literature. However, the small sample size as well as the use of single centre for the present study could be considered a limitation. Further large-scale studies are needed to support the present findings.
References
- Agenor A, Bhattachrya S. Infertility and miscarriage: common pathways in manifestation and management. Women’s Health 2015; 11(4):527-541.
- Medina RR, Segovia AG, Leon AJ, et al. New decision-tree model for defining the risk of reproductive failure. Am J Reprod Immunol.2013; (1):1-10.
- Choudhry SR, Knapp LA. Human reproductive failure 1: immunological factors. Hum Reprod Update. 2000; 7(2):113-134.
- Kumar P, Mahajan S. Pre-implantation and post-implantation therapy for the treatment of reproductive failures. J Hum Reprod Sci. 2013; 6(2):88-92.
- Coulam CB, Acacio B. Does immunotherapy for treatment of reproductive failures enhance live birth? Am J Immunol. 2012; 67(4):296-303.
- Pandey D, Gupta S. Current update on recurrent pregnancy loss. J Basic Clin Reprod Sci. 2019; 8(1):1-6.
- Stevenson EL, Hershbberger EP, Bergh PA. Evidence-based care for couples with infertility. J Obstet, Gynecol, Neonatal Nurs 2016; 45(1): 199-110.
- Conran N, De Paula EV. Thromboinflammatory mechanisms in sickle cell disease: challenging the hemostatic balance. Hematologica. 2020; 105(10): 2380-2390.
- Jayarangiah A, Kariyanna PT, Chen X, et al. Covid 19-associated coagulopathy: an exacerbated immunothrombosis response. Clin Appl Thromb Hemost. 2020; 26:1-11.
- Al-Aghary AR, Almorish MAW, Jaffer DWM, et al. Platelet indices in evaluation of patients with recurrent pregnancy loss. Asian Pac J Reprod . 2018; 7(1): 15-18.
- Ogbuabor AO, Onyia NL, Ohotu EO. Evidence for platelet activation according to some platelet indices in a cohort of type 2 diabetic mellitus patients. Saudi J Biomed Res. 2022; 7(11): 299-303.
- Okafor IA, Saanu OO, Olayemi O, et al. Characterization of primary female infertility in a Nigerian tertiary hospital: a case control study. Afr J Reprod Health. 2022; 26(8): 66-82.
- Sadeghi M. The 40th anniversary of IVf; has ART success reached its peak? Journal of Reprod Infertil. 2018; 19:67-68.
- Gerotziatas GT, Dreden PV, d’Argent EM, et al. Impact of blood hypercoagulability on in vitro fertilization outcomes: a prospective longitudinal observational study. Thromb J. 2017; (9): 1-11.
- Pino MD, Ruberto MF, Costanzo G, et al. Chonic spontaneous urticarial: low grade disseminated intravascular coagulation only partially reversed Omalizumab. Clin Exp Med. 2022; 10238: 1-8.
- Foley JH, Conway EM. Cross talk pathways between coagulation and inflammation. Circ Res. 2016; 118(9): 1392-1408.
- D’Angels G. Inflammation and Coagulation: a continuum between coagulation activating and prothrombotic state. J Blood Disord. 2015; 2(1): 1023.
- Dankova N, Aleksandrovna MO, Borisovna TT,et al. Genetic and hemostasiological Predictors of IVF pregnancy. Gynecol Endocrinol. 2017; 33(51): 32-35.
- Avcioglu SN, Altinkaya DO, Kucuk M, et al. The association between platelet indices and clinical parameters in recurrent pregnancy loss. Gynecol, Obstet, Reprod Med. 2014; 20:146-149.
- Engin-Ustun Y, Ozgu-erdinc AS, Yilmaz N, et al. Human chitinase-3-like protein:a pathogenic role in recurrent implantation failure. Medeniyet Med J 2018;33(2):100-104
- Niraimathi M, Renu GV, Anand M. Evaluation of platelet counts and indices in various clinical conditions using automated hematology analyzer in a tertiary care hospital. Annals of Pathol Lab Med. 2018; 5(7): 626-630.
