Full HTML
Virtual reality experiences in medical education: A systematic literature review
Jacob Lahti1,2, Kartik Akkihal3, Randall Ordovich-Clarkson1, Kelli Kosako Yost2,4,5, Thomas C Varkey2,4,5,6
Author Affiliation
1The College of Science, Engineering, and Technology, Grand Canyon University,
2Banner Health, Phoenix,
3Center for Health Equity Research, Northern Arizona University, Flagstaff,
4Department of Neurology, The College of Medicine, University of Arizona,
5Banner University Medical Center - Phoenix,
6The Colangelo College of Business, Grand Canyon University, Phoenix, Arizona
Abstract
background: Some studies suggested that teaching anatomy with a virtual reality simulator would greatly enhance medical education. The purpose of this work is to analyze the available literature to determine the effectiveness of virtual reality as a learning tool for anatomy teaching in medical schools. Materials and Methods: This literature review was completed in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines on 7.9.2022. The three databases that were utilized were Google Scholar, Cochrane, and PubMed. After performing the search utilizing the listed guidelines, two independent researchers shared and debated their individual lists, ultimately combining them and applying further exclusion criteria. This resulted in two remaining articles which addressed the research question. Results: One of the most notable findings in both articles is that students who utilized virtual reality in their anatomy learning demonstrated improvement in their understanding of structure locations and spatial relationships. Additionally, student’s ability to read and understand diagnostic imaging markedly improved for images presented both on exams and in face-to-face settings following virtual reality-based learning interventions. Virtual reality technology also increased interest in anatomy when utilized in the anatomy classroom, though this interest was limited to the anatomic region(s) in which the virtual reality sessions focused. Discussion/Limitations: Due to the scarcity of topically relevant results, this particular systematic review is unable to express anything beyond potential promise in the use of virtual reality-based interventions in the medical school anatomy classroom. As virtual reality technologies have been shown to potentially add benefit in these applications, there is reason to believe that new literature will become available in the near future.
DOI: 10.32677/yjm.v2i2.4070
Keywords: Anatomy education, Learning tools, Medical school, Virtual reality
Pages: 68-74
View: 6
Download: 7
DOI URL: https://doi.org/10.32677/yjm.v2i2.4070
Publish Date: 28-09-2023
Full Text
INTRODUCTION
Over the last several decades, the interest in utilizing different technologies to enhance medical student education has increased drastically. These technologies include video products such as “Osmosis”, “Picmonic”, “Pathoma”, and “Sketchy”, digital flashcard services like “Anki”, and large question banks, like “UWorld” and “AMBOSS” [1, 2]. These digital products serve to augment the current curriculum at major medical institutions and are now considered the go to resources for many medical students - often replacing more traditional methods of education such as attendance of lectures, peer studying group sessions, tutoring services, or office hours [1, 2]. One such technological intervention that has garnered a substantial amount of student, educator, and administrative excitement is that of virtual reality technology for fully immersive learning experiences [3-5]. The main idea of this intervention is that students can utilize virtual reality resources to simulate those hard to replicate experiences such as cadaver dissection or studying with prosected specimens as either adjunctive experiences or in place of these hands-on experiences entirely [3-5]. There have even been suggestions that these products might be able to serve as high quality stand-in training and practice options for surgical residents and students interested in surgery. One such example is that of Meta’s “The Impact Will Be Real” commercial, in which a surgeon practices performing heart surgery in a virtual reality space as training prior to performing the actual procedure on a living patient in the operating room [6]. A real-life example of this virtual reality integration is in the replication of code events in hospital settings, like that seen with the Oxford Medical Education’s 360-degree virtual simulations [7]. Such software technologies, at least in theory, would allow for improved action in real life scenarios as the students or residents would have had a much greater amount of exposure earlier on as compared to their colleagues who are undergoing traditional training under current methods. Thus, giving these students the chance to make mistakes and learn by trial and error without additional risk to the life and the overall physical well-being of patients.
One particular area of great interest for the application of virtual reality technologies is that of virtual anatomy laboratories in the medical education space. The primary role of the virtual reality anatomy labs would be as a replacement to, or to be used in conjunction with, the traditional gross dissection and anatomy laboratory classrooms in medical schools around the globe. The goal with the implementation of these interventions would be to hopefully enhance the overall learning of the students in these courses, as well as their understanding of anatomical structures and their spatial relationships to each other. Unlike with traditional cadavers or plastic models, these three-dimensional (3D) images have the added benefit of being far easier to rotate and manipulate in space without the natural restrictions that would prevent one from freely rotating a cadaver, or even a prosected specimen which may require additional support to prop up in place. Additionally, these students would have a direct increase in the overall time spent with the subject matter because of the asynchronous and portable nature of the virtual reality technologies. In theory, this ease of manipulation and increase in time spent with the materials should help to improve test scores for these students compared to colleagues who did not utilize such technology. This subsequently should lead to greater anatomical understanding and overall betterment of later clinical practice. However, these theories are insufficient at best without evidence-based backing. The research question that this review addresses is, “What does the current literature say about the use of virtual reality technologies in the human anatomy classroom for teaching medical students?” The purpose of this paper is to analyze the available literature to determine the efficacy of virtual reality as a learning tool for medical school anatomy education.
Materials and Methods
This systematic literature review was completed in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines as defined by Moher et al. on 7.9.2022 [8]. We mimicked the specific guidelines utilized by Tremmel et al., in their systematic literature review on obesity [9].
Search Strategy
Relevant articles were obtained by performing a systematic search across three major databases. This systematic search was performed on 7.09.2022 and the three databases utilized were Google Scholar, Cochrane, and PubMed. To ensure that results can be reproduced with ease and that openness in regards to data collection is clear, the search parameters are detailed below:
Google Scholar: Results published between 1.1.2018-7.09.2022. Search terms were “VR” or “Virtual Reality” and “Medical Students” and “Anatomy” and “Randomized Control Trial”
Cochrane: Results published between 1.1.2018-7.09.2022. Search terms were ““VR” or “Virtual Reality” and “Medical Students” and “Anatomy”. This database allowed the team to filter exclusively for Randomized Control Trials and as such, it was unnecessary to add it as a tertiary search term.
PubMed: Results published between 1.1.2018-7.09.2022. Search terms were “VR” or “Virtual Reality” and “Medical Students” and “Anatomy”. This database allowed the team to filter exclusively for Randomized Control Trials and as such, it was unnecessary to add it as a tertiary search term.
Inclusion and Exclusion Criteria
To be included within this systematic review, the extracted articles were assessed utilizing the following criteria: (1) The articles must have been written in the English language; (2) Studies were written and published on or after 1.1.2018 and on or before 07.09.2022; (3) Full-text copies of the studies were available via open-access or through library access via an affiliated organization; (4) Must be a randomized control trial. Exclusion criteria included: (1) Studies that did not look at VR OR that looked at an alternative intervention such as augmented (AR), extended (XR) or mixed (MR) realities; (2) Studies that did not look at medical students; (3) Review articles; (4) Articles that were not in peer reviewed journals; (5) Studies that were not randomized control trials; (6) Reports or articles that were not peer reviewed.
The reason that the articles were limited to the last five years of publication was due to the rapid increase in the type, use, and adoption of virtual reality technologies by different schools and organizations. Therefore, it was determined by the research team that articles published before 1.1.2018 would have a lighter likelihood of being out of date with the current trends in the use of the technology and therefore would not be of use in answering relevant questions moving forward. This narrow view, while appropriate, may have limited the total number of articles aimed at those medical schools which utilized earlier versions of the virtual reality technologies.
Selection and Data Extraction
Two authors (J.L. and T.V.) independently performed the aforementioned steps of the systematic review as outlined by PRISMA guidelines by first analyzing all three databases for potential matches. The initial screening step had the researchers independently read the title and abstract of each potential match and compare it to the inclusion and exclusion criteria that were listed above. Lists were then subsequently screened for potential duplicates and these duplicate articles were removed. These authors then compared their individual lists of potentially acceptable articles, challenging each other until a single, agreed-upon list was formulated and developed into a singular Excel spreadsheet. Remaining articles that the authors could not come to consensus on were brought to a third author (K.A.) for review and were included or excluded based on his judgment after he read the title, abstract, and full text as necessary. Figure 1 illustrates each step of the review process, along with how many papers were eliminated at each phase.
.png)
Figure 1. Demonstrated here is the PRISMA Flow Sheet with the number of papers eliminated at each step of the total process for the Virtual Reality Systematic Literature Review
RESULTS
Collected within Table 1 is the final list of articles utilized in the systematic review. Each of the articles are broken down for the reader’s benefit and include the topics that were tested by each study, the study sizes of the trials, and the main results. Other results of each of the studies can be found within the original articles.
Table 1. Listed here are the results of the search and a summary of each of the major studies included from the systematic review.
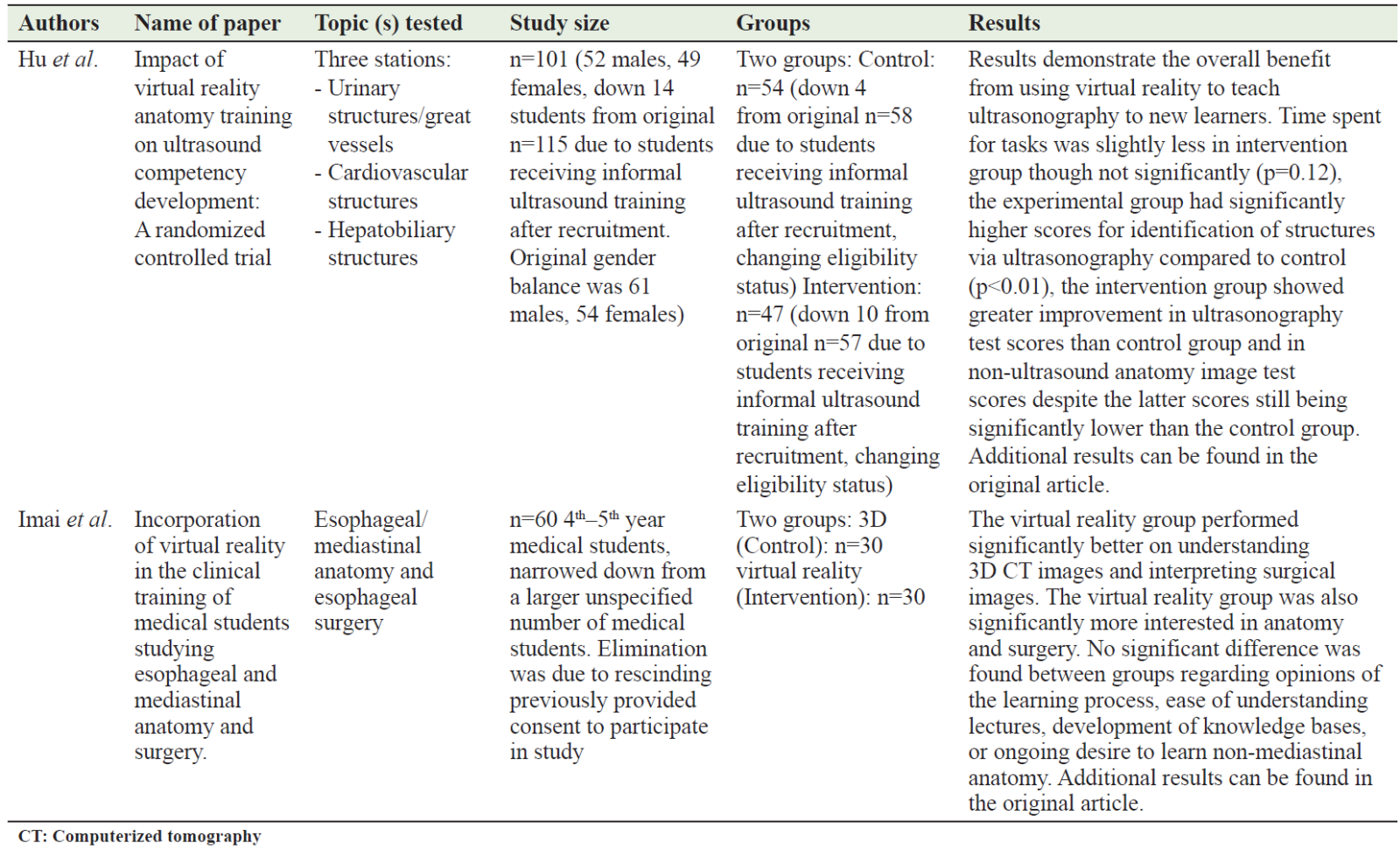
The two studies of interest obtained their data through specific means of testing after randomization. In the Hu et al. study [10], the researchers recruited the participants through email and were randomly assorted into either the control or the VR group. Those that received informal ultrasound training within three months (14 total participants) were removed. To ensure that randomization was preserved the groups remained from that point forward the same and were compared based on completion. The outcome of interest for the Hu et al. study [10], was performance on a 10-question multiple choice 2D anatomic imaging test. In the Imai et al. [11] paper, the researchers recruited the participants through including all the students that rotated through their department between June 2020 and March 2021. These students were split into two groups randomly with 30 participants each. The students were only included after they provided written consent for participation in the study. The outcome of interest for the Imai et al. [11] paper was the ability for the students to correctly answer 4 questions on anatomical knowledge and positioning, these questions are further detailed in the original study.
The two articles obtained through the systematic review process each looked at different anatomical areas and had a focus on different teaching points. The Hu et al. study [10] looked at the effects that the educational experience had both on teaching anatomy and on ultrasound competency for those students involved in the experience. The researchers focused on three separate regions of anatomical significance for their research - the hepatobiliary tree, cardiovascular structures, and urinary structures and great vessels. This particular study found that the virtual reality experience improved the students' aptitude both with ultrasound tests and non-ultrasound anatomy images. However, the testing group still scored poorly compared to their control group counterparts. Whether or not the results may have been subject to some degree of self-selection bias (i.e. selecting only for those students who were desirous to do anything to increase scores or students that perceived a greater need for help also being those who were more likely to volunteer) was not explained.
In the Imai et al. [11] paper, the researchers focused on the use of three dimensional (3D) computerized tomography (CT) images of the mediastinal structures (specifically that of the esophagus). The researchers looked at how the students interacted with these 3D images and their understanding of the anatomy both in surgical images and with the 3D CT scans. The researchers found that there was no major statistically significant difference found between the two groups regarding opinions of the learning process, the ease of understanding the materials that were presented during the lectures. Additionally, there was no major ongoing desire to learn non-mediastinal anatomy afterwards despite an increased interest in mediastinal anatomy. This particular study was small, with a total of only 60 students utilized. This brings into question both the power of the overall study, and the validity of the conclusion that the null hypothesis (that there was no difference between the two groups) should be accepted.
Key Highlights
One of the most notable findings in both articles is that students who utilized virtual reality in their anatomy learning demonstrated improvement in their understanding of structure locations and spatial relationships. Additionally, student’s ability to read and understand diagnostic imaging markedly improved for images presented both on exams and in face-to-face settings following virtual reality based learning interventions. Virtual reality technology also increased interest in anatomy when utilized in the anatomy classroom, though this interest was limited to the anatomic region(s) in which the virtual reality sessions focused.
Reasons for Exclusion of Some Promising Articles
Expanding on the exclusion criteria already presented, it is worthwhile to analyze particular applications of these criteria that led to four of the final six papers being excluded during data extraction. These four papers seemed promising upon initial cursory screens of the full-text, but upon more analytic review in the data extraction phase, it was found that each of them individually failed to meet full inclusion criteria or did indeed meet one or more exclusion criteria. Greuter et al. looked at the applicability of virtual reality as a teaching tool for students learning to locate and classify aneurysms in various arteries of the cerebral circulation, and while students were required to know these arteries to classify aneurysm location, anatomy was not the primary focus, leading to the ultimate exclusion of this paper [12]. Pickering et al. used virtual reality to help medical students learn sensory and motor pathways of the central nervous system, and while the paper actually met all inclusion criteria, there was a significant lack of clarity and consistency surrounding the methods and results. Specifically, inconsistencies were found in the number of participants throughout the study, the conclusions of the authors regarding the significance of certain pieces of data, and finally the interchangeable use of the phrases ‘modified reality’ and ‘virtual reality’. As a result, the authorial team of this paper felt that this made the article unfit for inclusion [13]. Ruthberg et al. used modified reality as a direct opposition to virtual reality, and so even an analysis of the virtual reality component of their modified reality intervention would have been inappropriate, if even possible [14]. Lastly, Weyant et al. actually focused on guidance for librarians who were looking to install virtual reality systems for studying, and while they selected medical students to be their primary focus in the study they performed, their guidance was not to medical school librarians nor specific to assisting medical students in learning anatomy [15]. For these reasons, these papers were all excluded from the final assessment and results of this particular paper.
DISCUSSION/LIMITATIONS
Due to the scarcity of topically relevant results, this particular systematic review is unable to express anything beyond potential promise in the use of virtual reality based interventions in the medical school anatomy classroom. Based on the two papers that fulfilled criteria and looked into the use of these technologies in teaching anatomical sciences, there is evidence that this intervention increases the interest in the anatomical structures and regions studied. However, not much else is known and the total sample size in these studies is very small (with a sum total between the two included studies being less than 200 individuals). This makes these findings inherently unreliable to those trying to generalize the results found to the general population of medical students. As virtual reality technologies have been shown to potentially add benefit in these applications, there is reason to believe that with the full return of students to the classroom following the hopeful conclusion of the COVID-19 pandemic, that new literature will become available in the near future. Until then, the current literature remains lacking in regards to the utilization of this technology as a novel supplement or replacement to traditional medical school anatomy education methods.
As is the case with any systematic review, there are naturally going to be other papers that are released on the topic after the initial date of database search, and during and after the writing and publication process. This literature review only looks at those papers which were published up until 07.09.2022. There may have been other papers published in databases to which the authors did not have access, that were unavailable because of a language barrier, or that were in peer review and have since come into the literature after the specific date of 07.09.2022. Lastly, this paper only looked into the use of virtual reality technologies within the anatomical classroom, as opposed to the broader use of virtual reality in medical school education at large, which may have led to different conclusions. This self-limitation of scope was done as the anatomical classroom has often been theorized as the area where virtual reality could provide the greatest benefit in medical school education. Nevertheless, this did naturally limit the total number of papers which fulfill our search criteria and as a result those which were included in our final assessment of the current body of literature.
One final limitation which may have limited the utility of the review was restricting the literature search to only those papers that were published in the English language. This as a consequence may have reduced important research from those non-English speaking centers where VR technology may be currently in use such as medical education centers in nations such as China, Japan, and Germany. The main reason for this limitation was the lack of access to these non-English sources. However, future research may need to examine other non-English sources to ensure no significant references have been missed.
Theoretical Engagement
One area of theoretical engagement is that of student interest and its positive effects on motivation and learning. Student interest is a smaller sub-portion of the larger Self-Determination Theory originally postulated by Ryan and Deci in the early 2000s [16]. In Self-Determination Theory, a student’s motivation is affected by three major components - competence, autonomy, and relatedness. These components can be affected by social positioning, lack of ability to choose either in what they engage with or with the level at which they engage with the materials, and difficulty with social relationships. Nevertheless, when these areas are utilized appropriately or enhanced by an educational intervention this leads to an enhancement of both the student’s mental well-being and their self-motivation to learn the course materials at hand [16].
According to the papers by Weber [17] and Schiefele [18], interest in the topics that are being presented increases the levels of engagement that the students have in the materials, and this by nature increases the level of learning that occurs for the students. The theoretical reason that this might lead to an increase in the level of engagement by the students might be similar in nature to the reason that any novel learning device - whether mnemonic, game, or other new intervention, increases the learner’s engagement [19]. This engages in the student’s autonomy to choose inherently increasing their self-motivation to engage with the course materials. The novelty of the object (which in this case is the virtual reality technology) increases the intrinsic desire to interact or play with the object. This model of utilizing the intrinsic curiosity of the learner to increase their interest, motivation, and learning has been demonstrated in numerous settings [20-23]. Such settings are inclusive of the elementary school classroom, the community college or university classroom, graduate school, and professional school settings including medical school, law school, and dentistry classrooms [20-23]. This support of relevant learning theories should serve as strong backing for the need for further research into these virtual reality interventions.
Another area in which the use of virtual reality technologies engages with Self-Determination Theory is that it can be performed asynchronously from normal course materials like that of cadaver laboratories or other laboratory sections. This again increases the autonomy of the students increasing their self-determination and, as a result, motivation as they are now able to decide for themselves how much time and effort they can and will devote to the anatomical materials at hand. This also engages with the two most well documented scientific enhancements in learning spacing and interleaving as students can intersperse other learning activities in between engagement with the anatomy materials that they learn through virtual reality technologies [24-29].
Considerations From Field Work and Dissection Experience
Two of the authors (J.L. and T.V.) have extensive experience in the fields of both full-body cadaver dissection as well as specialty organ removal and dissections for educational purposes in both the undergraduate, graduate, professional schooling, and continual educational spaces. Additionally, author J.L. continues to work as an instructor of cadaver-based undergraduate anatomy labs. This collectively provides a unique perspective for the authorial team on the role and background of cadavers and prosections in the classroom and the areas in which VR may provide benefit not just for the students, but for educators as well.
No two cadavers are ever the same as each other, which is logical as no two humans are, but these differences can be a point of difficulty for dissectors, instructors, and students when trying to learn to identify the same structures on several different bodies. What is more, the events leading up to end of life and those immediately following can play a significant role in determining the starting quality of the cadaver, which a dissector despite their best efforts still may struggle to work with in certain scenarios. Such examples from authorial experience include severe contractures inhibiting clean dissection access to parts of limbs, venous pooling from bedridden states leading to messy or poorly embalmed or poorly visible muscles, atrophied or severely destroyed muscles due to lack of use or advanced stage pressure ulcers, cancers leading to erosion or other destruction of structures especially in the cranial, thoracic, and abdominopelvic cavities. All of these issues provide a substantial challenge for even high-level dissectors to work with the existing structures and clean and present them in the best, most accurate way possible. This extensive list, which becomes more prevalent especially in geriatric patients who tend to make up a large portion of body donors, focuses just on pathological conditions that impair effective dissection and teaching and does not begin to consider the other major issues of anatomical variation and flaws in the embalming process.
Anatomical variation can be a great source of confusion especially to the newer dissectors and newer students. Both the presence and absence of accessory muscles that vary in prevalence such as the palmaris longus and the plantaris may be misleading, as students have pre-set expectations for the presentation or lack thereof of these muscles based on their study materials whether they are past cadavers, photographs, or other resources. Other common anatomical variations that can lead to confusion for dissectors include arterial differences such as that seen in bovine heart, variants of the presentation of the brachial plexus (particularly as they relate to the terminal branches), and inconsistencies in veins, such as veins dividing into two veins that run parallel for a short length before rejoining, instead of running as one continuous vein, or named tributaries draining in to larger veins at abnormal locations.
Additionally, while the embalming and preservation process for body donors is fairly consistent and well-established, there are areas of particular note that are difficult to consistently embalm thoroughly which can lead to great difficulty for the dissector looking to prepare clean prosections that will be beneficial for students to learn from and appropriate for instructors to teach from. Perhaps the most noted area of difficulty to embalm consistently is the cranial cavity. This is due to historically poor penetration of the embalming fluid across the walls of the cerebral vasculature into the neural tissue. Oftentimes, this will lead to brains that are at best, in a highly gelatinous-like state free of stability, making dissection or structure identification practically impossible, or brains that are at worst, fully degenerated and present essentially as a puddle of semi-solid brain matter. Because of this, each year in different laboratories there is often a loss of said specimens for the use of students. For dissectors, the procedure of brain removal can sometimes be a lengthy process, and this time could arguably be better spent on other dissections. One of the potential areas in which virtual reality may play a role is in the standardization or supplementation of the course materials for neural anatomy courses. This could include virtual reality brain dissectors, neuroanatomy and physiology simulators, and other virtual reality technologies which improve and augment the students’ learning experience.
An additional consideration should be of the physical limitations placed by cadavers and prosections. Cadavers for obvious reasons must be kept in either a generally supine or prone position and the rotation from one position to the other often requires the work of at least two to three people and places extra wear and strain on the cadaver. Additionally, many organs are often kept relatively in place even if they are freed from fascia and connective tissue or other similar connections, and so some structures and aspects cannot be viewed or rotated easily, if at all, on cadavers. Such examples include the hepatic veins and the caudate and quadrate lobes of the liver, unless the liver has been removed from the body and kept as a separate organ, to which there are pros and cons. Prosections also are not always the most convenient either because they require the student to be away from their laptop, tablet, or other similar materials, to help maintain cleanliness.
However, none of this should be perceived to state that the authorial team does not support the validity or substantial benefit provided by cadaver-based learning. On the contrary, this is to make a case from firsthand experience about the need for supplementary interventions to provide for the students the greatest and most thorough learning experience possible. Virtual reality technology is a very strong contender for such a supplementary intervention as it may help provide opportunities to students that combine the ‘ideal’ view demonstrated in textbook illustrations with a semi-’hands-on’ approach that is more reminiscent of cadaver and organ use, effectively bridging the two.
Future Research Directions
While virtual reality has been around for some time, the specific role of this technology in healthcare and medicine, particularly in medical school anatomy education, is poorly researched and understood. Like other new devices and technologies over the years, virtual reality has shown some potential to improve how medical students engage with the topics and materials they are learning, alongside their overall understanding of anatomical structures and spatial relationships. Some specific research directions that would greatly enhance the quality of the relevant literature include: (1) Looking into the relationships between the utilization of virtual reality interventions and test scores on board exams, (2) the use of virtual reality technologies and mastery of more complex anatomical subspecialties such as neuroanatomy, (3) comparison of virtual reality only anatomy classrooms versus classrooms that are strictly cadaver-based and those that implement a blend of cadaver and virtual reality learning, and lastly, (4) the use of virtual reality interventions and student interest, motivation, and engagement as compared to the typical anatomical classroom with cadavers only.
CONCLUSIONS
This particular review analyzed the available literature from the last four-and-a-half years to determine the effect that virtual reality has on learning in the medical school anatomy classroom. The main idea of this intervention is that students can utilize virtual reality resources to simulate those hard-to-replicate experiences such as cadaver dissection or studying with prosected specimens as either adjunctive experiences or in place of these hands-on experiences entirely. Based on the currently available papers from the last four-and-a-half years, there is very little known about the effects of virtual reality, other than that it increases student interests in the topics and specific anatomical regions of study. As seen from the authorial team’s personal experience, there might be strong benefit in the standardization of the materials specifically in the neuro-anatomic educational space. It is the hope of the authorial team that the integration of this relatively novel virtual reality intervention into medical school anatomy education be the subject of further research, particularly for the benefit of the students in these courses and their future patients.
AUTHORS’ CONTRIBUTIONS
All authors contributed to the completion of this work. The final manuscript was read and approved by all authors
References
- Varkey TC, Merhavy ZI, Varkey RM, et al. Learning or memorization: self-directed medical school curriculum and the dangers of overemphasizing student selected ancillary resources. Galician Med J 2022;29:E202211–E202211..
- Wu JH, Gruppuso PA, Adashi EY. The Self-directed Medical Student Curriculum. JAMA. 2021 Nov 23;326(20):2005-2006.
- Pottle J. Virtual reality and the transformation of medical education. Future Healthc J. 2019 Oct;6(3):181-185.
- Pantelidis P, Chorti A, Papagiouvanni I, et al. Virtual and augmented reality in medical education. Medical and Surgical Education-Past, Present and Future. 2018 Mar 28:77-97.
- Lai P, Zou W. The application of virtual reality technology in medical education and training. Global Journal of Information Technology: Emerging Technologies. 2018. 8(1), 10–15.
- The impact will be real: Surgical training (YouTube): https://www.youtube.com/watch?v=wcb7kMvDHss [Last accessed on December 19, 2022].
- Oxford Medical Education. Virtual reality medical simulation. 360-DEGREE SIMULATION VIDEOS: https://oxfordmedicaleducation.com/simulation/360-degree-videos/ [Last accessed on July 10, 2022].
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009 Jul 21;339:b2535.
- Tremmel M, Gerdtham UG, Nilsson PM, et al. Economic Burden of Obesity: A Systematic Literature Review. Int J Environ Res Public Health. 2017 Apr 19;14(4):435.
- Hu KC, Salcedo D, Kang YN, et al. Impact of virtual reality anatomy training on ultrasound competency development: A randomized controlled trial. PLoS One. 2020 Nov 23;15(11):e0242731.
- Imai T, Tanaka Y, Hatanaka Y, et al. Incorporation of virtual reality in the clinical training of medical students studying esophageal and mediastinal anatomy and surgery. Surg Today. 2022 Aug;52(8):1212-1217.
- Greuter, L., De Rosa, A., Cattin, P., et al., (2021). Greuter L, De Rosa A, Cattin P, Croci DM, et al. Randomized study comparing 3D virtual reality and conventional 2D on-screen teaching of cerebrovascular anatomy. Neurosurgical Focus. 2021 Aug 1;51(2):E18
- Pickering JD, Panagiotis A, Ntakakis G, et al. Assessing the difference in learning gain between a mixed reality application and drawing screencasts in neuroanatomy. Anat Sci Educ. 2022 May;15(3):628-635.
- Ruthberg JS, Tingle G, Tan L, et al. Mixed reality as a time-efficient alternative to cadaveric dissection. Med Teach. 2020 Aug;42(8):896-901.
- Weyant EC, Carroll M, Walden RR. Lessons Learned: Medical Library Pilot Testing of a Virtual Reality Anatomy Lab. Journal of Electronic Resources in Medical Libraries. 2021 Jan 2;18(1):20-34.
- Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000 Jan;55(1):68-78.
- Weber K. The relationship of interest to internal and external motivation. Communication Research Reports. 2003 Sep 1;20(4):376-83.
- Schiefele U. Interest, learning, and motivation. Educational psychologist. 1991 Jun 1;26(3-4):299-323.
- Varkey T. “Watch Your Language”: A Literature Review on the Use of Dirty words in Improving Memory for Adult Learners. Proclins Psychiat. 2021;1(1).
- Kusurkar R A. Autonomous motivation in medical education. Medical teacher.2019. 41(9), 1083-1084.
- Triarisanti R, Purnawarman, P. The Influence of Interest and Motivation on College Students’ Language and Art Appreciation Learning Outcomes. International Journal of Education.2019. 11(2), 130-135.
- Allen J, Robbins S. Effects of interest-major congruence, motivation, and academic performance on timely degree attainment. J Couns Psychol. 2010 Jan;57(1):23-35.
- Puspitarini YD, Hanif M. Using Learning Media to Increase Learning Motivation in Elementary School. Anatolian Journal of Education. 2019 Oct;4(2):53-60.
- Firth J. Boosting learning by changing the order and timing of classroom tasks: implications for professional practice. Journal of Education for Teaching. 2021 Jan 1;47(1):32-46.
- Li C, Yang J. Role of the hippocampus in the spacing effect during memory retrieval. Hippocampus. 2020 Jul;30(7):703-14.
- Kim AS, Wiseheart M, Wong-Kee-You AM, et al. Specifying the neural basis of the spacing effect with multivariate ERP. Neuropsychologia. 2020 Sep 1;146:107550.
- Badgaiyan RD, Fischman AJ, Alpert NM. Striatal dopamine release in sequential learning. Neuroimage. 2007 Nov 15;38(3):549-56.
- Varkey TC, Varkey JA, Ding JB, et al. Asynchronous learning: a general review of best practices for the 21st century. Journal of Research in Innovative Teaching & Learning. 2022 Dec 12;16(1):4-16.
- Sisti HM, Glass AL, Shors TJ. Neurogenesis and the spacing effect: learning over time enhances memory and the survival of new neurons. Learn Mem. 2007 May 10;14(5):368-75.
