Full HTML
First report of post-vomiting subcutaneous peri-lacrimal drainage system emphysema
Maher Mohamad Najm1,2, Bashar Hasan Kayal3, Abdalmalek Mohamad Najm4, Hassan Ahmad Ibrahim5
Author Affiliation
1Consultant, Department of Pediatrics, Pediatric Emergency Center, Hamad General Hospital,
2Clinical Lecturer, Department of Clinical Medicine, College of Medicine, Qatar University, Doha, Qatar,
3Specialist, Department of Pediatrics, Alnoor Hospital, Relief International, Taftanaz, Syria,
4Resident, Department of General Surgery, Ahmad Maher Teaching Hospital, Cairo, Egypt,
5Medical Student, Department of Pediatrics, College of Medicine, Qatar University, Doha, Qatar.
Abstract
Subcutaneous emphysema is defined as a trapped air in tissues under the skin. This entity most often occurs in the chest wall and neck but can infrequently happen in other parts of the body like the orbital area
DOI: 10.32677/yjm.v2i1.3825
Pages: 62-63
View: 5
Download: 7
DOI URL: https://doi.org/10.32677/yjm.v2i1.3825
Publish Date: 10-05-2023
Full Text
Subcutaneous emphysema is defined as a trapped air in tissues under the skin. This entity most often occurs in the chest wall and neck but can infrequently happen in other parts of the body like the orbital area [1]. The main mechanism of subcutaneous emphysema is the traumatic damage of the anatomical air-filled cavities or canals. Most of the rare, reported cases of orbital and periorbital emphysema were described in adults as complications of several types of traumas including direct trauma, recent or previous surgery [2,3], barotrauma secondary to non-invasive ventilation, such as continuous positive airway pressure (CPAP) therapy [4], and even post forceful nose-blowing [5]. In this report, we described the first reported case of post-vomiting subcutaneous emphysema surrounding the medial canthus of the right eye in a 10-year-old boy.
A previously healthy 10-year-old boy presented to the emergency department with an acute history of frequent vomiting and diarrhea but no fever. The child was diagnosed with acute gastroenteritis and the treatment plan was to give the child a stat dose of ondansetron orally and then monitor him for a short time before sending him home if he tolerated the oral intake. The child had suddenly developed an attack of violent vomiting after being given the oral medication and immediately thereafter the nurse noticed a smooth bulge of skin around the inner corner of the right eye and the side of the nose, the event being interpreted by the nurse as an allergic skin reaction of ondansetron. Accordingly, the nurse immediately called the doctor, who evaluated the patient and found him to be stable with normal vital signs and no clinical signs of anaphylactic or hypovolemic shock, but the assessment of the skin lesion that appeared suddenly revealed that subcutaneously trapped air had a C-shape around the right side lacrimal caruncle and connected with a subcutaneous air column on the lacrimal sac measuring about 1 cm in length (Figure 1), the movements of his right eyeball were normal with preserved visual acuity, there was no proptosis, chemosis, subconjunctival hemorrhage, orbital or periorbital pain. The patient and his family were reassured, and gentle pressure on the subcutaneous emphysema toward the lacrimal drainage was sufficient to dislodge the trapped air. Another oral dose of ondansetron was then administered and the patient was observed until the oral intake was tolerated, then the child was discharged home with oral medication and referral to the ophthalmology clinic. At the follow-up the next day, the parents reported no episodes of vomiting or orbital swelling since the discharge. A week later, there was no subcutaneous emphysema observed but the parents did not bring the patient to the ophthalmology clinic.
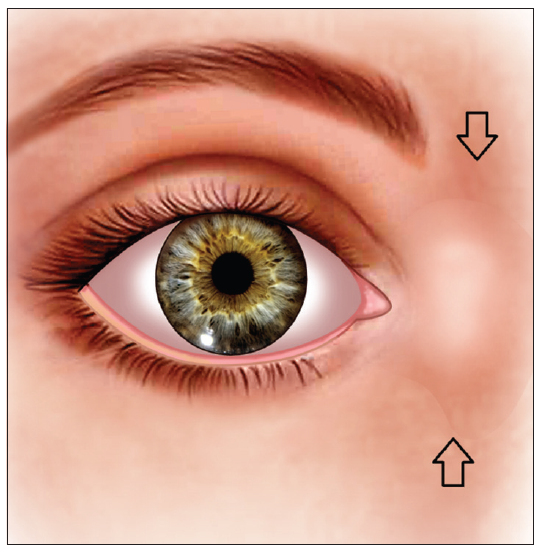
Figure 1: The site of subcutaneous emphysema
Lacrimal drainage system is usually protected against retrograde airflow by a group of one-way valves, the most important valves are valve of Hasner, which is a mucosal flap at the distal tip of the nasolacrimal duct prevents air from entering the lacrimal sac when the nose is blown and valve of Rosenmuller, which prevent reflux of tears from the lacrimal sac into the canalicular system [6]. The subcutaneous emphysema in our case can be described as a layer of air under the skin that envelops the upper part of the lacrimal drainage pathway, i.e., the superior and inferior canaliculi and lacrimal sac. This emphysema has mostly resulted from a leak of air from the nasal cavity to the subcutaneous tissues through a perforated lacrimal excretory system. It is known that forceful vomiting can generate a high pressure which can rarely lead to a rupture of the esophagus (Boerhaave’s syndrome) [7] or even the pharynx [8]. Vomiting is also one of the underlying etiologies of the Valsalva maneuver which is a forced expiration of air against a closed airway, resulting in raised intra-abdominal, intrathoracic, and upper airways pressure including the pharynx and nose. We proposed that the violent sudden vomiting created high pressure in our patient's nasal cavity, exceeding the pressure threshold that the Hasner’s valve can normally withstand, resulting in a sudden regurgitation of high-pressure airflow which caused a perforation in the lacrimal drainage system and air leakage to the subcutaneous area.
.png)
Figure 2: The components of the lacrimal drainage system and pathogenesis of subcutaneous emphysema
Figure 2 describes the lacrimal drainage pathway and the suggested pathogenesis of subcutaneous emphysema in our patient. Air regurgitation through the lacrimal drainage system with Valsalva maneuver have been described in 3 cases, two adults and one child, by Swati Malik et al who hypothesized that the predisposing factor is the valvular dysfunction in the lacrimal excretory apparatus [6].
In conclusion, this is the first case report that described the occurrence of subcutaneous emphysema in the naso-ocular fossa after forceful vomiting. Clinicians should be aware of this complication and its management.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient for publication of this case report and all accompanying images. The patient understands that while every effort is made to maintain the confidentiality of their identity, names, and initials, anonymity cannot be guaranteed.
AUTHORS’ CONTRIBUTIONS
All authors contributed to the completion of this work. The final manuscript was read and approved by all authors
References
- Aghajanzadeh M, Dehnadi A, Ebrahimi H, et al. Classification and Management of Subcutaneous Emphysema: a 10-Year Experience. Indian J Surg. 2015;77(Suppl 2):673-677.
- Casselman JW, Peene PT, Coppens F, et al. Pneumatocele in a traumatic ruptured lacrimal sac mucocele. Rofo. 1989;150(1):106-107.
- Das S, Ali MJ, Bansal S, et al. Lacrimal Sac Pneumatocele Following Blunt Nasal Trauma. Ophthalmic Plast Reconstr Surg. 2017;33(6):e150-e151.
- Singh NP, Walker RJE, Cowan F, et al. Retrograde Air Escape via the Nasolacrimal System: A Previously Unrecognized Complication of Continuous Positive Airway Pressure in the Management of Obstructive Sleep Apnea. Annals of Otology, Rhinology & Laryngology. 2014;123(5):321-324.
- Komro J J, Williams P J, Lin D J. Orbital Defect and Emphysema After Nose Blowing: A Case Report and Literature Review. Cureus. 2022;14(12): e32958.
- Malik S, Ali MJ, Sundararajan M, et al. Retrograde Air Flow through the Lacrimal Drainage System with Valsalva Maneuver. J Otolaryngol Rhinol. 2020; 6:096.
- Chikkappa MG, Morrison C, Lowe A, et al. Paediatric Boerhaave's syndrome: a case report and review of the literature. Cases J. 2009;2:8302.
- Roh JL, Park CI. Spontaneous Pharyngeal Perforation After Forceful Vomiting: The Difference from Classic Boerhaave's Syndrome. Clin Exp Otorhinolaryngol. 2008;1(3):174-176.
