Full HTML
Two Decades of Recurrent Granuloma, Due to Foreign Body in the Scalp, Mimicking Bone Tumor
Adel Khelifa1, Muneer Mufadhal Al-Zekri2
Author Affiliation
1Neurosurgeon, Departement of Surgery, EPH Achour Ziane, Ouled Djellal, Algeria,
2Surgeon, Departement of Surgery, Ibn Sina Specialist Hospital, Sanaa, Yemen
Abstract
Foreign bodies (FBs) in the scalp are a common incident following head trauma, especially in traffic accidents, and are detected in the early post-traumatic period. The persistence of these FBs may cause pain and paresthesia.
DOI: 10.32677/yjm.v2i1.3758
Pages: 60-61
View: 4
Download: 7
DOI URL: https://doi.org/10.32677/yjm.v2i1.3758
Publish Date: 10-05-2023
Full Text
Foreign bodies (FBs) in the scalp are a common incident following head trauma, especially in traffic accidents; and are detected in the early post-traumatic period. The persistence of these foreign bodies may cause pain and paresthesia.
We report a case of 41 years old man, whose victim it’s been twenty years of physical aggression, in which the victim was hit by a brick occasioning a frontal wound stitched at the time without sufficient exploration. Months later the patient presented several episodes of a frontal scalp nodular lesion with pus leakage (figure 1).

Figure 1: Aspect of the scalp lesion at admission
The lesions were only treated with local antibacterial agents. Four years before the patient consults at our level, he consulted a dermatologist who performed a removal of the skin lesion. Months later the lesion reappeared. At our level the clinical examination suspected a bone lesion; so CT was performed. Brain imaging was strongly evoking bone tumors or osteitis (figure 2).
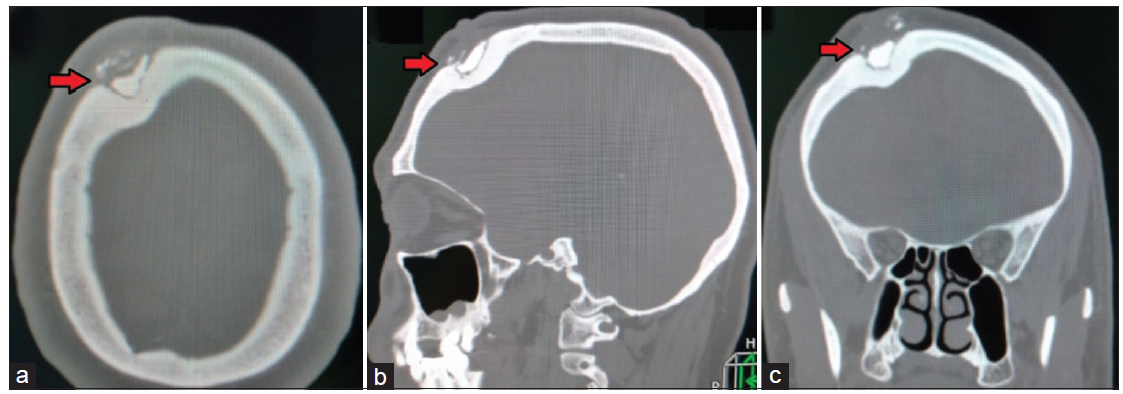
Figure 2: Pre-operative brain CT in the bone window; (a) axial slide, (b) sagittal, and (c) coronal. The arrow points to the location of the foreign body nested in a bone defect
The patient was operated on under general anesthesia. First, a carcinogenic removal of the scalp lesion was performed; then, when reaching the bone, hard red friable bodies well separated from proportionally healthy bone were found. Those findings raise suspicion of the presence of foreign bodies nested in the bone from the first head trauma. So a carcinologic removal of the affected bone was postponed, and simple curettage was performed (figure 3).
.png)
Figure 3: Per-operative photo showing the final aspect of lesion site with removal of cutaneous granuloma and conserving bone integrity (inner table +++)
The postoperative course was without complications. The histological study confirmed per-operative findings: multiple stony foreign bodies associated with inflammatory reaction especially lymphocytes around vessels and the foreign bodies.
Retained foreign bodies after head trauma are common and the diagnosis is made in the emergency room which could be challenging and time-consuming. Wood glass and metal are the most objects retained after a traumatism; rocks are less communally encountered [1]. Most times FBs are found by visual inspection or palpation otherwise the diagnosis is made by imaging; generally by plane radiography; in some times CT is needed to look for small undetected FBs. Unfortunately in one-quarter of cases, radiographs miss the diagnosis. Radiological sensitivity for FBs is around 98.6% for metal 75.5% for glass, and only 7.4% for wood [1]. Missed FBs is among the top three causes of litigation [1]. Retained FBs could cause toxic and allergic reactions, inflammation, or infection. The presence of foreign bodies launches an infinite inflammatory process that will not subside until the foreign body is solubilized or at least contained and isolated in a fibrous capsule; leading to a break in local reaction. A minor trauma could rupture the capsule, and so set off the inflammatory process again [2]. Infections or chronic pain and dysesthesia are the most clinical presentations. Those signs are usually located on the site of a cutaneous defect or subcutaneous mass, misdiagnosed as skin neoplasm. Since we encountered in our experience many serious affections with the only presentation of subcutaneous mass [3] we think that removing such lesions without reliable imaging is risky. Another particularity of our case is the bone involvement; in fact, the rock filled the bone defect in such a shape that evokes strongly a bone tumor. Without extemporaneous histopathological examination, we think that conserving the integrity of macroscopic healthy tissue, and postponing carcinological removal is judicious since per-operative evidence is in favor of non-malignant lesions.
To sum up, the persistence of foreign scalp bodies could be the cause of infinite medical consultations and so enormous physical and psychological suffering for the patient. Evoking the presence of foreign bodies is paramount in every case of open-head trauma. Finally, Scalp lesions are never removed without imaging proof of non-invasion of the bone.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and all accompanying images. The patient understands that while every effort is made to maintain the confidentiality of their identity, names and initials, anonymity cannot be guaranteed.
AUTHORS’ CONTRIBUTION
All authors contributed to the completion of this work. The final manuscript was read and approved by all authors.
References
- Levine MR, Gorman SM, Young CF, et al. Clinical characteristics and management of wound foreign bodies in the ED. Am J Emerg Med. 2008;26(8):918-22.
- Lammers RL. Soft tissue foreign bodies. Ann Emerg Med. 1988;17(12):1336-47.
- Khelifa A, Assoumane I, Bachir S, et al. Skull metastasis of hepatocellular carcinoma in normal liver: Case report. Rom. neurosurg. 2019;33(4):478-481.
