Full HTML
Schwannoma with an unusual anterior chest wall location: A rare case report
Sharad Bharat Sable1, Vitthalrao Chintalwar2, Ketaki Utpat3, Unnati Desai4
Author Affiliation
1Junior Resident, Topiwala National Medical College and B.Y.L. Nair Hospital, Mumbai, Maharashtra, India
2Senior Registrar, Topiwala National Medical College and B.Y.L. Nair Hospital, Mumbai, Maharashtra, India
3Associate Professor, Topiwala National Medical College and B.Y.L. Nair Hospital, Mumbai, Maharashtra, India
4Associate Professor and In-Charge, Department of Pulmonary Medicine, Topiwala National Medical College and B.Y.L. Nair Hospital, Mumbai, Maharashtra, India
Abstract
Chest wall schwannoma is a rare intercostal nerve tumor originating from Schwann cells. Here we present a case of a 44-year-old woman who presented with symptoms of cough, fever, and left-sided chest pain. A plain chest radiograph was unremarkable and was further evaluated with a contrast-enhanced chest computed tomography (CECT) scan, which showed a well-defined, encapsulated soft-tissue mass in the left anterior first intercostal space. The diagnosis of schwannoma was based on histopathological and immunohistochemical studies of tissue biopsies taken from the lesion. The patient was referred to a higher oncology center for further treatment where he received symptomatic treatment for the pain and cough after which he improved. The patient was discharged and followed up in the clinic. Six months later, the patient underwent another chest CECT, which revealed no growth in size from the first one. Therefore, it was decided to keep the patient in regular follow-up since the lesion remained stable in size
DOI: 10.32677/yjm.v2i1.3783
Keywords: Anterior chest schwannoma, Neurogenic tumor, Posterior mediastinal mass
Pages: 48-50
View: 4
Download: 9
DOI URL: https://doi.org/10.32677/yjm.v2i1.3783
Publish Date: 10-05-2023
Full Text
Introduction
Neurogenic tumors arise in tissues derived from the embryonic neural crest and are classified based on whether the tumor cell originates from a nerve sheath, nerve cells (ganglia), paraganglia, or peripheral nerves. Neurogenic tumors can be found throughout the body. In the thorax, neurogenic tumors are most commonly found in the posterior mediastinum, accounting for 75% of all posterior mediastinal neoplasms [1]. In adults, schwannomas and neurofibromas are the most common neurogenic tumors arising from the nerve sheath [2-3].
Schwannoma has several names in the literature, such as neurilemmoma, neurilemoma, or neuroma, which originate in the perineural cell called Schwann's cell. The tumor has a predilection for the head, neck, and flexor sides of the extremities [4]. The chest wall is a very rare site for schwannomas. In this report, we have presented a case of an extremely rare anterior chest wall schwannoma to raise physicians' awareness of this unusual clinical condition and to consider it when evaluating a patient with a similar clinical scenario.
CASE REPORT
A 44-year-old female presented to our outpatient department with a 1-month history of cough with minimal non-bloody expectoration, occasional left-sided non-radiating chest pain, and intermittent fever (not documented). The patient has been receiving treatment for retroviral disease for 12 years (latest CD4 count: 537 cells/µl). she was a non-smoker and had no history of pulmonary tuberculosis or use of anti-tuberculosis drugs prior to this episode. There was no significant past or family history. Physical examination was unremarkable. Routine blood work was done including a complete blood count, renal function test, and serum electrolytes which were within normal limits. Two sputum samples were processed for Gene/ Xpert MTB Rif which turned out to be negative. A standard chest X-ray posteroanterior view was done which was unremarkable. (figure 1).

Figure 1: Unremarkable chest X-ray
The patient was treated with oral broad-spectrum antibiotics with antitussives for five days. Due to persistent symptoms, the patient was further evaluated with a contrast-enhanced computed tomography (CECT) of chest, which revealed a well-defined, iso-dense, slightly lobulated soft-tissue lesion with a post-contrast enhancement measuring 2.5x1.8 cm on the first left intercostal space close to the first costochondral junction, suggesting a peripheral nerve sheath tumor. (figure 2).
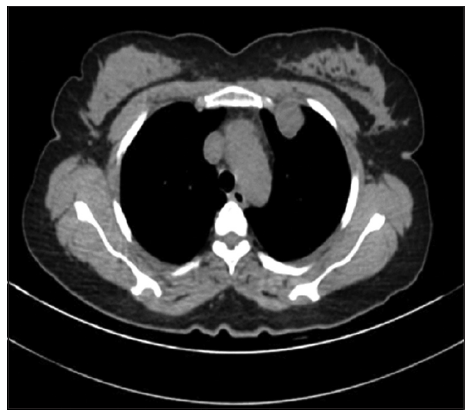
Figure 2: CT thorax suggestive of well-defined, isodense, and mildly lobulated soft-tissue lesion in first intercostal space on the left side
The patient was then subjected to a Fluro-deoxy glucose Positron emission tomography scan (FDG PET) which showed FDG uptake in well-defined, lobulated soft tissue (SUV max 3.4) in the first left intercostal space. (figure 3). After essential workup and counseling of the patient and relatives the patient was referred for a CT-guided biopsy of the suspected lesion. The procedure was well-tolerated under local anesthesia and all aseptic precautions with only minimal pain at the biopsy site as the sole post-procedure complication. A biopsy sample preserved in formalin was sent for investigations namely histopathological examination and acid-fast bacilli culture.
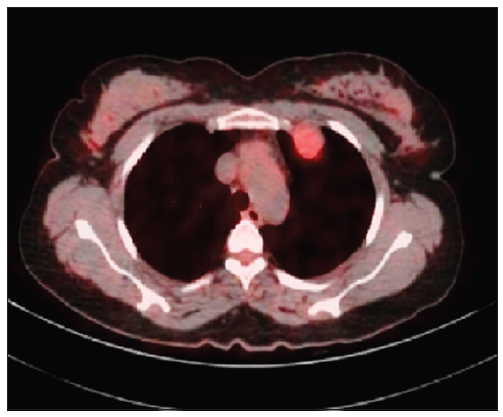
Figure 3: Flurodeoxy glucose positron emission tomography (FDG) scan shows FDG uptake in same lesion with SUV max of 3.4
The histopathological report suggested a low-grade spindle cell tumor that was neurogenic in origin (Figure 4) and the acid-fast bacilli culture was negative. By immunohistochemistry. the tumor cells were positive for S100P (diffuse and strong) and SOX10 (diffuse and strong). They were negative for CD34, EMA, and STAT6. The MIB1/KI67 marker index was 1-2%. Features were consistent with Schwannoma/Neurilemmoma and pointed to a cellular (benign) nerve sheath tumor. The patient was then referred to a higher oncology center for further treatment where he received symptomatic treatment for the pain and cough after which he improved. The patient was discharged and followed up in the clinic. Six months later, the patient underwent another CECT of the chest, which revealed no growth in size from the first one. Therefore, it was decided to keep the patient in regular follow-up since the lesion remained stable in size.
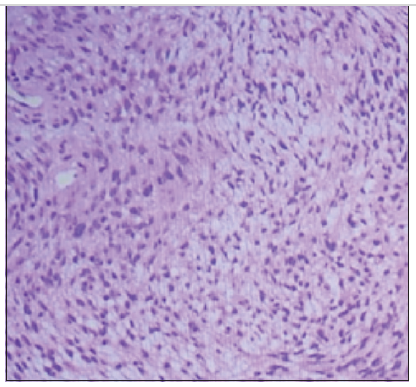
Figure 4: Histopathology slide showing hypercellular areas and spindle cells suggestive of schwannoma
Discussion
Chest wall tumors are mostly metastatic in nature, and primary chest wall tumors are very rare. Only 1% to 2% of chest wall tumors are of primary origin, of which primary pleural schwannoma accounts for about 5% to 10% [4,5]. A chest wall schwannoma is a rare tumor that arises from peripheral nerve sheath Schwann cells of intercostal space. These neurogenic tumors most frequently located in posterior part of mediastinum or chest wall however, in our case the lesion was found in the anterior chest wall, which is extremely unusual site [6]. Schwannomas are usually benign, asymptomatic, and slow-growing. Men and women are equally affected in their third and fourth decades of life [5]. While most are asymptomatic, the most common complaint is invasion of intercostal nerve, bone, and chest wall, or cough and dyspnea from compression of the tracheobronchial tree [7]. Similarly, our patient was a female in her fourth decades of life, who presented with 1-month history of cough with left-sided chest pain.
Given the initial asymptomatic course, most mediastinal schwannomas are found incidentally, and the diagnosis is often delayed or missed. As in our case, the chest X-ray is usually unremarkable. Chest computed tomography and magnetic resonance imaging studies are the main imaging modalities used for this type of pathology [5-8]. Computed tomography often shows sharply defined margins and iso- or slightly hypodense lesions on plain scans that appear heterogeneous on contrast-enhanced imaging due to differentiation in cellularity, xanthomatous changes, and degeneration. Despite this, it is difficult to determine whether a tumor is benign or malignant. Tissue biopsy, fine-needle cytology, or incisional biopsy can be used to make the diagnosis and determine the extent of resection needed. [5,8]. In our case, the diagnosis was based on histopathological and immunohistochemical studies of tissue biopsies taken from the lesion.
The standard of care for chest wall schwannomas is predominantly surgical resection, either by thoracoscopic operation or by open thoracotomy, particularly in the absence of a preoperative diagnosis, development of symptoms, and growing tumor, with most cases reported in the literature showing a good prognosis after tumor resection [5-8]. In our case, there was no surgical intervention as the patient's symptoms had resolved and the lesion was stable.
Conclusion
Anterior chest wall schwannoma is a rare clinical condition with variable presentations. Although usually benign, malignant transformations have been documented, therefore, tissue biopsy with appropriate histopathologic and immunohistochemical studies is required to confirm the diagnosis. Our case showed that non-surgical follow-up is acceptable since the patient's symptoms have resolved and the tumor has been shown to be benign with a stable, unaltered size.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient for publication of this case report and all accompanying images. The patient understands that while every effort is made to maintain the confidentiality of their identity, names, and initials, anonymity cannot be guaranteed.
AUTHORS’ CONTRIBUTIONS
All authors contributed to the completion of this work. The final manuscript was read and approved by all authors
References
- Davidson KG, Walbaum PR, McCormack RJ. Intrathoracic neural tumours. Thorax. 1978;33(3):359–367
- Reeder LB. Neurogenic tumors of the mediastinum. Semin Thorac Cardiovasc Surg. 2000;12(4):261–267.
- Reed JC, Hallet KK, Feigin DS. Neural tumors of the thorax: subject review from the AFIP. Radiology. 1978;126(1):9–17.
- Kale SS, Gosavi VS, Jagadale RV. Ancient chest wall schwannoma: A case report with review of literature. Med J DY Patil Univ 2015;8:505-7.
- Kongjarern S, Tajarernmuang P, Wannasopha Y, et al. Multifocal Ancient Thoracic Schwannomas: A Case Report and Review of Literature. J Med Case. 2017; 8: 277-279
- Kara M, Özkan M, Dizbay Sak S, et al. Giant ancient schwannoma of the posterior mediastinum cytologically misdiagnosed as a malignant tumour. A case report. Acta Chirurgica Belgica. 2002 Jan 1;102(6):464-6.
- Amin R, Waibel BH. An Unusual Presentation of a Posterior Mediastinal Schwannoma Associated with Traumatic Hemothorax. Case Rep Surg. 2015;2015:175645.
- Athanassiadi K, Kalavrouziotis G, Rondogianni D, et al. Primary chest wall tumors: early and long-term results of surgical treatment. Eur J Cardiothorac Surg. 2001;19(5):589-593
