Full HTML
Acute gallbladder disease – The virtue of performing a laparoscopic cholecystectomy in the early stages of case management
Naseralla Juma Elsaadi Suliman1,2
Author Affiliation
1Consultant General Surgeon, Department of Surgery, Benghazi Medical Center, Benghazi, Libya,
2General Surgery Senior Lecturer, Department of Surgery, Faculty of Medicine, University of Benghazi, Benghazi, Libya
Abstract
Background: In a Benghazi Medical Center, this observational study assessed the role of laparoscopic Cholecystectomy in the early stages of acute gallbladder illness.
Methods: From January 2022 to December 2022, all emergency and urgent admissions for acute gallbladder disease were identified, and additionally, data from hospital medical records were then evaluated retrospectively.
Results: Out of a total of 334 patients with gallstone diseases, we found 321 individuals (206 with acute biliary colic, 115 with acute calculous cholecystitis), and 13 with acalculous cholecystitis. Early laparoscopic surgery for acute calculous cholecystitis had a greater conversion rate than procedures for acute biliary discomfort (19% versus 4%; P = 0.002). When surgery was performed 72 hours from the onset of the symptoms for patients with acute calculous cholecystitis, the conversion rate was considerably lower (one out of 25) than when surgery was postponed past 72 hours (14 out of 53) or later performed electively (seven out of 23) (P = 0.014). In comparison to elective surgery for acute biliary colic (three of 66), elective surgery for prior acute cholecystitis was linked to a higher conversion rate (seven of 22 patients) (P = 0.002).
Conclusion: Laparoscopic cholecystectomy for acute calculous cholecystitis needs to be done within 72 hours of the onset of symptoms, and it is worthwhile.
DOI: 10.32677/yjm.v2i1.3883
Keywords: Acute biliary colic, Acute calculous cholecystitis, Conversion rates, Laparoscopic cholecystectomy
Pages: 18-24
View: 4
Download: 7
DOI URL: https://doi.org/10.32677/yjm.v2i1.3883
Publish Date: 10-05-2023
Full Text
INTRODUCTION
In the laparoscopic era, early cholecystectomy has been established as valuable for acute calculous cholecystitis, [1, 2] with a better prognosis shown for early laparoscopic intervention. [2–6] However, many medical institutions worldwide do not have a policy of early laparoscopic cholecystectomy for acute gallbladder disease, likely due to concerns over higher conversion rates, lack of general surgeons trained in laparoscopic cholecystectomy, and resource limitations preventing non-urgent cases from entering the operating room early.
Laparoscopic cholecystectomy (LC) is the standard treatment for cholelithiasis, with increasing evidence supporting its use in early intervention for acute cholecystitis. [7-9] Acute cholecystitis is a common complication of gallstones, diagnosed in 10%-35% of patients admitted for cholecystectomy. [10,11]
Early LC is generally considered the optimal treatment for acute cholecystitis by most surgeons. [12,13] Feasibility and safety of early LC for acute cholecystitis have been documented in both randomized and non-randomized studies in experienced hands. [14] Early cholecystectomy for gallstone disease is beneficial for early recovery and reducing associated complications. [15]
Conversion rates for early laparoscopic cholecystectomy in acute cholecystitis patients vary from 6% to 32%, and the optimal timing for surgery remains unclear due to varying case mix and patient selection in most studies that did not compare different operation points within the same admission. Time elapsed between admission and operation may affect conversion rates. [16-18] Laparoscopic cholecystectomy for inflamed gallbladders is technically more challenging than for acute biliary pain without inflammation (biliary colic or discomfort).
Complicated anatomy, bleeding, inflammation in acute situations, and adhesions in elective settings are the primary causes of conversion to open surgery. Determining conditions that optimize laparoscopic cholecystectomy success would be helpful, although the decision to convert should prioritize overall success and safe completion of the procedure. The aim of this observational study was to evaluate the treatment of all patients with acute gallbladder disease at the Benghazi Medical Center (BMC) in the city of Benghazi over a 12-month period to determine the effectiveness of early laparoscopic procedures.
MATERIALS AND METHODS
Study design, population, and setting
This retrospective observational study was conducted at Benghazi Medical Center (BMC) from January to December 2022. It included patients with acute gallbladder disease requiring emergency or urgent admission. The Lothian Surgery Audit system collects patient data for the General Surgery Department at BMC, a leading department in eastern Libya that handles both emergency and routine surgical cases. The department reports an average of 1480 general surgical cases, with gallbladder removal surgeries accounting for 25% of all cases. This system includes free text for operation notes, discharge summaries, and clinic letters, with specific codes for patient diagnoses and surgical records. We performed a retrospective data review from patient records, ultrasound reports, blood test results, and histopathological findings.
Diagnosis, inclusion, and exclusion criteria
The diagnosis of acute cholecystitis (AC) was made by clinical and abdominal ultrasound findings. Clinical findings included right hypochondrial pain with or without epigastric pain, nausea/vomiting, dyspepsia, and fever. Ultrasound findings included features of a positive sonographic Murphys sign, gallbladder distention, pericholecystic fluid, and gallbladder wall thickness greater than 3 mm. Patients who underwent surgery during acute admission for acute calculous cholecystitis were also diagnosed based on histopathologic evidence of acute inflammatory cells.
Patients with acute gallbladder disease were included (ie, acute acalculous cholecystitis, acute biliary colic, and acute calculous cholecystitis), while patients with other conditions such as gallstone ileus, obstructive jaundice, ascending cholangitis, and gallstone-induced pancreatitis were excluded.
Statistical analysis
The Wilcoxon sum-of-rank test was used for two-sample unpaired quantitative data, and the non-parametric Kruskal-Wallis test was used for three-sample data. Fisher's exact test was used to analyze qualitative data with a two-tailed P value. A statistically significant result was defined as P < 0.050. Data analysis was performed using SPSS software (v.21; IBM Corp, Armonk, NY, USA)
Ethical approval
The BMC administration granted permission to carry out this study. The data were therefore gathered retrospectively from the Medical Registry Department's patient file record.
RESULTS
During the study period, 334 cases of acute gallbladder disease were recruited, of whom 321 (96.0%) had acute gallstone disease and 13 (4%) had acute acalculous cholecystitis. Of the 321 cases of acute gallstones, 115 (35.8%) cases had acute calculous cholecystitis, and 206 (64.2%) patients had acute biliary colic.
Management and outcome
Seventy-three (63%) of the 115 patients with acute calculous cholecystitis (women; 60%) underwent cholecystectomy during the same acute stay, and of these, 64 patients (88%) underwent laparoscopic cholecystectomy, whereas 9 (12%) underwent open cholecystectomy. Three patients who did not receive an early cholecystectomy underwent a percutaneous cholecystostomy. 45 patients in total were sent home without having surgery right now; of these, two received follow-up care in the city’s hospitals, 18 underwent elective surgery, 14 were well enough to decline surgery, and 10 needed additional emergency admission (two with acute cholecystitis, seven with acute biliary pain, and one with gallstone-induced pancreatitis).
Table 1 displays histopathological findings for patients who underwent early surgery, while Table 2 shows ultrasonographic and laboratory results for those who did not. Two elderly patients with extensive co-morbidities died from multiorgan failure and were deemed unfit for cholecystectomy.
Seventy-four patients (36%) of the 206 patients with acute biliary pain (50 women and 23 men) underwent an early cholecystectomy during the same acute admission; 71 had attempted laparoscopic cholecystectomy, and three underwent an open procedure because they had undergone a significant prior abdominal procedure. Of those who were discharged without surgery, 56 had an elective laparoscopic cholecystectomy, 46 improved with conservative treatment, and 30 required further emergency readmissions. Of these emergency readmissions, five of the 14 patients with acute acalculous cholecystitis (seven women) underwent surgery at the same acute hospitalization (three attempted laparoscopic and two open cholecystectomies). One patient who did not have an early cholecystectomy underwent a percutaneous cholecystostomy. Eight patients were discharged: two went on to later elective surgery, five recovered with conservative care, and one needed an additional emergency stay. In this group of patients, there were two fatalities: one from septic shock and one from venous thromboembolism (VTE). Flowcharts in figures 1 and 2, describes the management and outcomes of acute calculous cholecystitis and acute biliary colic cases.
Table 1: Patients with acute calculous cholecystitis who underwent early surgery, histopathological results
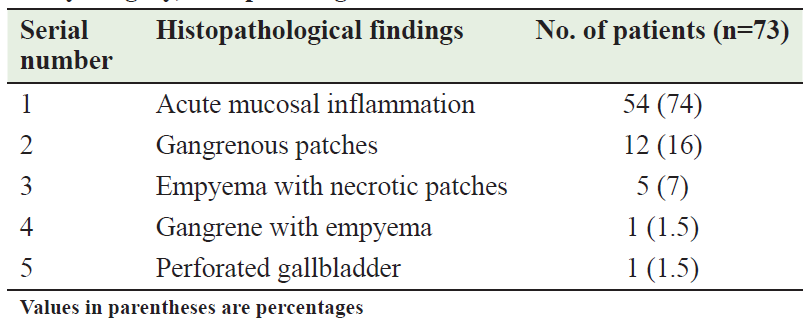
Table 2: Patients with acute calculous cholecystitis who were discharged without early surgery, ultrasonographic, and laboratory findings
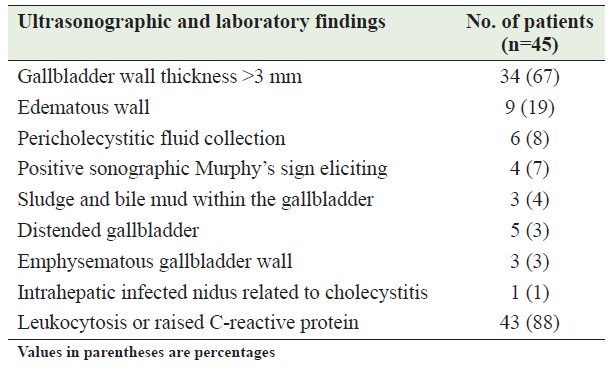
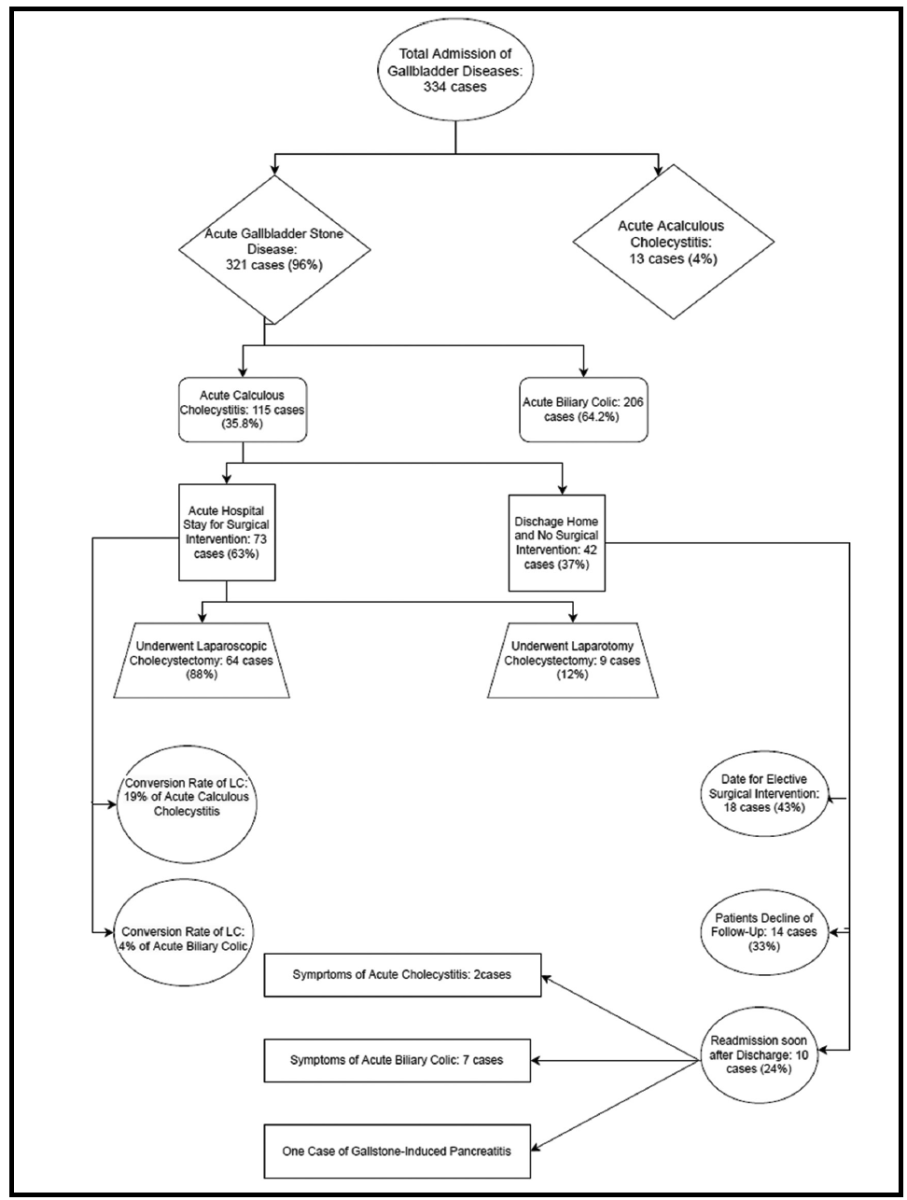
Figure 1: Flowchart describing the management and outcomes of acute calculous cholecystitis cases
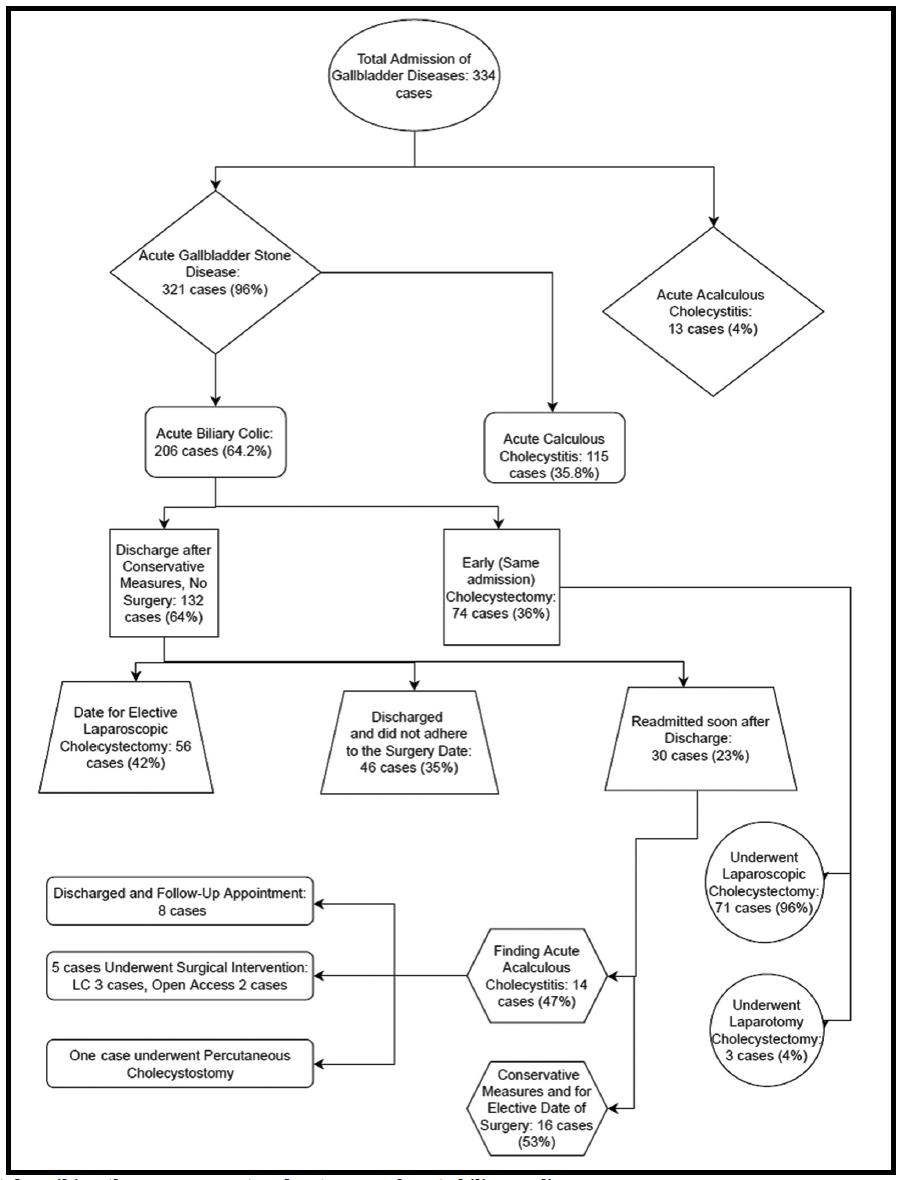
Figure 2: Flowchart describing the management and outcomes of acute biliary colic cases
Effect of age
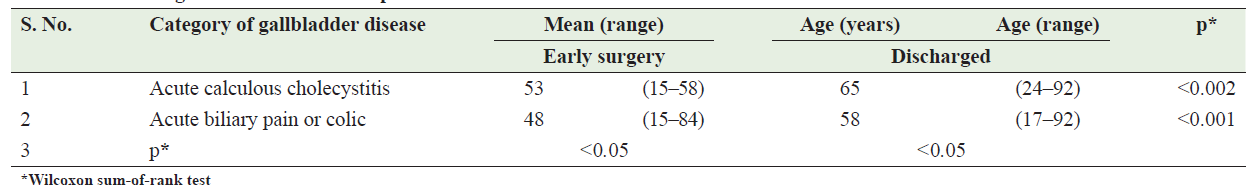
Patients with acute biliary colic/pain (n=53) and acute calculous cholecystitis (n=59) had similar age ranges (15-92 and 16-90 years, respectively) with no statistically significant difference (P ≤ 0.096). The mean age of patients with acute acalculous cholecystitis was 59 years (range: 35-93 years). Younger patients underwent early surgery for acute calculous cholecystitis (P ≤ 0.002) or acute biliary colic/pain (P ≤ 0.0003) compared to those who had a surgery postponed (Table 3).
Table 3: Patient age and the time of the operation
Existing extrahepatic bile duct stones
Overall, it was discovered that 34 (16.5%) of 206 patients with acute biliary pain and 9 (7.7%) of 118 patients with acute calculous cholecystitis had common bile duct stones. Preoperative endoscopic retrograde cholangiopancreatography (ERCP) was performed on 27 patients who had a high suspicion of having choledocholithiasis (abnormal liver function test findings and/or an aberrant biliary tree on ultrasound). The methods of stone retrieval were postoperative ERCP (8 patients), laparoscopic exploration of the common bile duct with choledochoscopy (three patients), conversion to open surgery (two patients), and in two patients, the filling defects found on cholangiography were bereft without intervention.
Laparoscopic conversion rate
Compared to 5% of patients with acute biliary discomfort, 22% of patients who underwent early procedures for acute cholecystitis had laparoscopic cholecystectomy converted to open surgery (P = 0.002). The conversion rate was higher (35%) in patients with prior acute calculous cholecystitis compared to those with prior acute biliary colic (6%) who had non-operative early therapy and subsequent readmission for elective cholecystectomy (P = 0.002). Three patients with acalculous cholecystitis underwent early laparoscopic cholecystectomy, and one of them required conversion.
Reason for conversion
In fourteen cases of acute calculous cholecystitis requiring early conversion, severe inflammation (in 11 cases) and complications such as bile duct stones (in 2 cases) or uncontrolled bleeding (in 1 case) obscured the anatomy around Calot's triangle, necessitating conversion. Strong adhesions were encountered during the procedure, but prior acute cholecystitis was not the sole cause as three patients had prior abdominal surgery.
Four patients with acute biliary pain required conversion during early treatment due to various reasons such as unclear anatomy caused by a greatly dilated common hepatic duct in one patient, adhesions in another, and a common bile duct stone in a third. Elective surgeries for biliary pain were complicated by adhesions in three patients with prior abdominal surgeries and a common bile duct stone in one patient. One patient with acute acalculous cholecystitis required conversion due to acute-on-chronic inflammation.
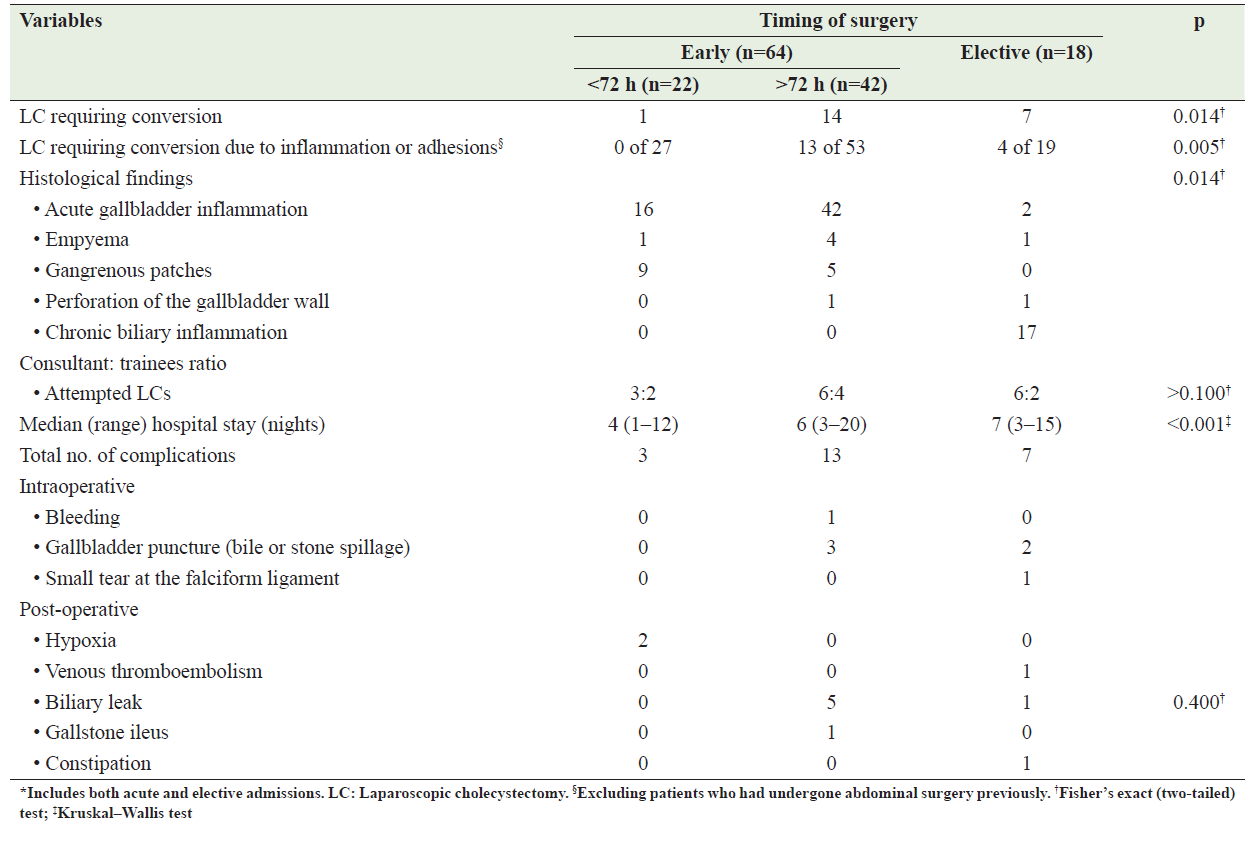
Timing of laparoscopic surgery
For patients with acute gallstone cholecystitis, the conversion rate was much higher when surgery was performed more than 72 hours after symptom onset or as elective surgery. Of the 22 patients who underwent laparoscopic cholecystectomy within 72 hours of symptom onset, only one required conversion due to a bile duct stone. However, in the group of 42 patients who underwent surgery after 72 hours or as elective surgery, 14 required conversion. When patients with prior abdominal surgeries were excluded, and only conversions due to adhesions or inflammation were considered, the conversion rates were zero out of 27, thirteen out of 53, and four out of 19, respectively, with a statistically significant difference (P = 0.005) as shown in Table 4.
There was no significant difference in the conversion rate between patients with acute cholecystitis who underwent surgery within 72 hours of symptom onset (2 out of 26), and those with acute biliary pain who underwent surgery in either an acute (4 out of 85) or elective (3 out of 65) setting (P = 1.000). The mean ages and sex ratios were also not significantly different among patients who received elective surgery within 72 hours, after 72 hours, or later (P = 0.117 and P = 0.890, respectively) as shown in Table 4.
Complications and hospital stay
Operations for acute calculous cholecystitis performed within 72 hours of symptom onset were associated with a lower overall rate of complications compared to those performed beyond 72 hours (13 out of 42) or in an elective setting (7 out of 18) as shown in Table 4. However, there was no statistically significant difference in the rate of postoperative biliary leakage between early procedures and elective operations or surgery within 72 hours (P = 0.400). The postoperative complications observed in the study were biliary injury, bleeding, port site infection or abscess, and gallbladder puncture (bile or stone spillage).
Hospital stays for patients varied up to 8 days, with the majority being discharged on the fourth day (56%) or the third day (40%), and only 5% requiring stays of 4-7 days. Those who experienced complications after surgery or laparoscopic conversion had even longer stays. For patients with acute calculous cholecystitis, surgery within 72 hours resulted in significantly shorter hospital stays compared to elective surgery or surgery after 72 hours (P < 0.001), with a mean stay of 2.5±0.4 days, as shown in Table 4.
Eighty-seven % of the 73 laparoscopic procedures for acute calculous cholecystitis, in both acute and elective settings, were performed by trainees (supervised and unsupervised). However, there was no significant difference in the conversion rate between trainees and consultants in either setting, as shown in Table 4.
Table 4: Comparison of acute calculous cholecystitis patients who underwent laparoscopic cholecystectomy both before and after 72 h of admission, as well as those who underwent elective (interval) procedures
Discussion
This study confirms previous studies [3, 5, 6, 19, 20] that early laparoscopic cholecystectomy is beneficial for patients with acute calculous gallbladder disease. [1, 3-6, 19, 20] There is strong evidence supporting early laparoscopic surgery in eligible patients. Acute cholecystitis is mainly caused by gallstones and is the leading reason for emergency cholecystectomy. [21]
Early surgical intervention is recommended even if the operation cannot be performed within 72 hours due to the risk of developing dense inflammatory adhesions. [20,21] Delayed surgery, either beyond 72 hours after the onset of symptoms or as elective surgery, carries a greater risk of complications and may require readmission and emergency surgery after discharge. [21,22] The current trial showed that 21% of patients required readmission and emergency surgery.
Early surgical intervention is recommended within 72 hours of acute pain onset, during the edema phase of inflammation. Delayed intervention during the hypervascular phase, abscess formation, necrosis, and scarring is not recommended. This study supports the use of surgical intervention within 72 hours of symptom onset.
Early laparoscopic cholecystectomy is safe and beneficial in randomized trials. [3, 5[ However, there is no consensus on the optimal timeframe between admission and surgery, and discrepancies in study findings may be due to methodological variables such as time delay from symptom onset or admission to surgery. Most studies suggest waiting 72-96 hours before surgery, [7-9, 23-26] but some studies have found no impact on conversion rates with longer waiting for times. [27,28] Two other investigations suggest an ideal maximum wait of 72 hours, consistent with current findings. [7, 29]
In this study, a dedicated emergency operating room was provided, but not always available during regular working hours. Therefore, some patients with simple biliary pain were discharged with instructions for elective surgery. Postponing surgery in patients with no inflammation did not increase the conversion rate, but it appeared to worsen technical problems in cases of inflammation.
High-risk patients with calculous or acalculous cholecystitis may not be suitable for early cholecystectomy and can pose challenges for surgeons. A recent study suggests that such patients, who often have comorbidities, [30] should undergo cholecystectomy early and may not require a subsequent procedure if no stones are found. [31] The authors recommend this approach unless the patient's clinical condition improves significantly with non-operative care and diagnosis confirmation.
Laparoscopic cholecystectomy can be technically difficult in several conditions22, including acute cholecystitis, empyema gall bladder, gangrenous cholecystitis, and porcelain gall bladder. Situations with previous laparotomies, postoperative adhesions, portal hypertension, cirrhosis of the liver, and surgery in pregnant patients. [32] Additionally, bile leakage after cholecystectomy is a major cause of postoperative complications and extended hospital stays. [33]
According to Tokyo guidelines, to decrease the complication of gallstone disease we have to observe surgical difficulty appropriately and standardized the treatment options accordingly. [34]
Early surgery for acute calculous cholecystitis and acute biliary pain has better outcomes compared to delayed surgery, according to this study. Laparoscopic procedures had similar conversion rates in both contexts, but early surgery reduced hospitalizations. The choice between early and delayed surgery will depend on available resources and patient/surgeon preferences. Early surgery is becoming more popular worldwide due to better resource utilization and shorter waiting lists with dedicated emergency and elective teams. [35] There was no difference in conversion rates between consultants and trainees, but most operations by trainees were supervised by consultants.
The retrospective design was the main limitation of this study and therefore the analysis relied on secondary data that did not allow for an adequate assessment of some variables such as the experience of the surgeons performing the procedures.
Conclusion
Early laparoscopic cholecystectomy performed within 72 hours of symptom onset in acute cholecystitis is a feasible, safe, and cost-effective option. This approach also results in a shorter hospital stay without affecting morbidity and mortality rates.
References
REFERENCES
- van der LindenW, Sunzel H. Early versus delayed operation for acute cholecystitis. A controlled clinical trial. Am J Surg 1970; 120: 7–13.
- McArthur P, Cuschieri A, Sells RA, et al. Controlled clinical trial comparing early with interval cholecystectomy for acute cholecystitis. Br J Surg 1975; 62: 850–852.
- Wilson RG, Macintyre IM, Nixon SJ, et al. Laparoscopic cholecystectomy is a safe and effective treatment for severe acute cholecystitis. BMJ 1992; 305: 394–396.
- Lo CM, Liu CL, Lai EC, et al. Early versus delayed laparoscopic cholecystectomy for treatment of acute cholecystitis. Ann Surg 1996; 223: 37–42.
- Lo CM, Liu CL, Fan ST, et el. Prospective randomized study of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Ann Surg 1998; 227: 461–467.
- Lai PB, Kwong KH, Leung KL, et al. Randomized trial of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg 1998; 85: 764–767.
- Gurusamy K, Samraj K, Gluud C, et al. Meta-analysis of randomized controlled trials on the safety and effectiveness of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg. 2010; 97(2): 141-50.
- Banz V, Gsponer T, Candinas D, et al. Population-based analysis of 4113 patients with acute cholecystitis: defining the optimal time-point for laparoscopic cholecystectomy. Ann Surg. 2011; 254(6): 964-70.
- Barcelo M, Cruz-Santamaria DM, Alba-Lopez C, et al. Advantages of early cholecystectomy in clinical practice of a tertiary care center. Hepatobiliary Pancreat Dis Int. 2013; 12(1): 87-93.
- Qureshi A, Haider J, Aziz A. Early Laparoscopic Cholecystectomy for Acute Calculous Cholecystitis: What is the Optimal Timing? J Surg Pak (Int) 2012; 17(1): 2012: 12-15.
- Afzal M, Rehman S, Mian MA, et al. Rate and reasons of conversion of laparoscopic cholecystectomy to open cholecystectomy? A prospective analysis of 450 consecutive laparoscopic cholecystectomies. PAFMJ. 2016; 66(1): 117-121.
- Engin O, Yildirim M, Cengiz F, et al. Laparoscopic anterograde cholecystectomy in acute cholecystitis. J Clin Med Res. 2009;1(3):186-7.
- Casillas RA, Yegiyants S, Collins JC. Early laparoscopic cholecystectomy is the preferred management of acute cholecystitis. Arch Surg. 2008; 143(6): 533–7.
- Gonz´alez-Rodr´ıguez FJ, Paredes-Cotor´e JP, Pont´on C. Early or delayed laparoscopic cholecystectomy in acute cholecystitis? Conclusions of a controlled trial. J Hepato- Gastroenterol. 2009; 56(89): 11–16.
- Imbisat MZ, Rizvi SAA, Ali I. An evaluation of early and delayed laparoscopic cholecystectomy for acute cholecystitis. Int Surg J. 2019; 6.
- Madan AK, Aliabadi-Wahle S, Tesi D, et al. How early is the early laparoscopic treatment of acute cholecystitis? Am J Surg 2002; 183: 232–236.
- Koo KP, Thirlby RC. Laparoscopic cholecystectomy in acute cholecystitis. What is the optimal timing for operation? Arch Surg 1996; 131: 540–545.
- Rattner DW, Ferguson C, Warshaw AL. Factors associated with successful laparoscopic cholecystectomy for acute cholecystitis. Ann Surg 1993; 217: 233–236.
- Papi C, Catarci M, D’Ambrosio L, et al. Timing of cholecystectomy for acute calculous cholecystitis: a meta-analysis. Am J Gastroenterol 2004; 99: 147–155.
- Cheema S, Brannigan AE, Johnson S, et al. Timing of laparoscopic cholecystectomy in acute cholecystitis. Ir J Med Sci 2003; 172: 128–131.
- Coccolini F, Allegri A, Ceresoli M, et al. Acute Cholecystitis and Cholangitis. In Acute Care Surgery Handbook. 2016; 171-193.
- Ahmad I. Cholecystectomy in acute cholecystitis. J Pak Med Assoc. 1992; 42(5): 112-5.
- 23 Eldar S, Sabo E, Nash E, et al. Laparoscopic cholecystectomy for acute cholecystitis: a prospective trial. World J Surg 1997; 21: 540–545.
- Eldar S, Sabo E, Nash E, et al. Laparoscopic versus open cholecystectomy in acute cholecystitis. Surg Laparosc Endosc 1997; 7: 407–414.
- Pessaux P, Tuech JJ, Rouge C, et al. Laparoscopic cholecystectomy in acute cholecystitis. A prospective comparative study in patients with acute vs. chronic cholecystitis. Surg Endosc 2000; 14: 358–361.
- Garber SM, Korman J, Cosgrove JM, et al. Early laparoscopic cholecystectomy for acute cholecystitis. Surg Endosc 1997; 11: 347–350.
- Knight JS, Mercer SJ, Somers SS, et al. The timing of urgent laparoscopic cholecystectomy does not influence the conversion rate. Br J Surg 2004; 91: 601–604.
- Bhattacharya D, Senapati PS, Hurle R, et al. Urgent versus interval laparoscopic cholecystectomy for acute cholecystitis: a comparative study. J Hepatobiliary Pancreat Surg 2002; 9: 538–542.
- Willsher PC, Sanabria JR, Gallinger S, et al. Early laparoscopic cholecystectomy for acute cholecystitis: a safe procedure. J Gastrointest Surg 1999; 3: 50–53.
- Lo LD, Vogelzang RL, Braun MA, et al. Percutaneous cholecystostomy for the diagnosis and treatment of acute calculous and acalculous cholecystitis. J Vasc Interv Radiol 1995; 6: 629–634.
- Sugiyama M, Tokuhara M, Atomi Y. Is percutaneous cholecystostomy the optimal treatment for acute cholecystitis in the very elderly? World J Surg 1998; 22: 459–463.
- Cianci P, Tartaglia N, Fersini A, et al. Acute Cholecystitis: Diagnostic Pitfall and Timing of Treatment. In Updates in Gallbladder Diseases 2017. Intech Open. 23-45.
- Dominguez-Rosado I, Sanford DE, Liu J, et al. Timing of surgical repair after bile duct injury impacts postoperative complications but not anastomotic patency. Ann Surg. 2016; 264(3): 544-53.
- Wakabayashi G, Iwashita Y, Hibi T, et al. Tokyo Guidelines 2018: Surgical management of acute cholecystitis: safe steps in laparoscopic cholecystectomy for acute cholecystitis (with videos). J Hepatobil Pancreat Sci. 2018; 25: 73-86.
- Addison PDR, Getgood A, Paterson-Brown S. Separating elective and emergency surgical care (the emergency team). Scott Med J 2001; 46: 48–50.
