Full HTML
Starr Edwards Ball Caged Mechanical Heart Valves’ Reverberations – Need for a Phoenix of Analysis with a Critical Mindset
Mark Christopher Arokiaraj
Author Affiliation
Professor, Department of Cardiology, Pondicherry Institute of Medical Sciences, Ganapathichettikulam, Kalapet, Puducherry, India.
Abstract
The mechanical heart valve prosthesis with a caged ball has been around for 60 years. It has since experienced changes and adjustments. The Starr Edwards valve was a pioneer and was taken out of clinical use in the late 2000s. Starr Edwards is reportedly close to or has reached the age of 50, according to numerous sources from around the globe. The author's observations and review of the literature about thrombogenicity, pannus formation, left ventricular outflow tract obstructions, and infective endocarditis in the Starr Edwards valves, which were reportedly higher before its clinical ending, was only an overestimation and were not supported by scientific data. However, it was less discussed in the article, along with potential benefits. The main reasons for its demise were its obtrusive size and unattractive shape. There have been several successful implantations of these valves in Asian nations and reports of fewer primary failures and unexpected cardiac fatalities. Therefore, there is a need for extensive data gathering, documentation, and more recent studies on these valves to prepare for a prospective revival of use with newer research, mainly when long-term durability is considered.
DOI: 10.32677/yjm.v2i1.3760
Keywords: Caged Ball valves, Starr Edwards, Thrombogenicity, Durability, Safety
Pages: 8-12
View: 5
Download: 7
DOI URL: https://doi.org/10.32677/yjm.v2i1.3760
Publish Date: 10-05-2023
Full Text
INTRODUCTION
The mechanical heart valve prosthesis is commonly used in the treatment of valvular heart disorders. The biophysics and models of these mechanical heart valves have undergone numerous changes and exist in their current form. Among many mechanical heart valve models, Starr Edwards (SE) is a standard model, and its implantation dates back 60 years or more. The currently used models have replaced the Starr Edwards valves, and it is no longer in clinical use. The article deals with some of the interesting aspects of the Starr Edwards valves, their evolution, general performance, and discontinuation. The report also discusses the literature on clinical performance, thromboembolism, and echocardiographic characteristics.
HISTORY OF STARR EDWARDS BALL CAGED MECHANICAL HEART VALVE
Albert Starr and Lowell Edwards worked and developed the first successful ball cage valve in Oregon medical school.[1] Albert Starr was a young surgeon, and Lowell Edwards was an experienced engineer. They made numerous modifications and finally arrived at the unshielded ball valve used in human beings. Their work offered hope for a large number of patients with rheumatic heart disease and other valvular heart diseases requiring mechanical heart valve replacement. The last model was mitral-6120 extended non-cloth valves, and its aortic counterpart 1260. The metallic cage was made of stellite, and the ball was silastic, which is silicone with 2% barium. Later replaced, the ball with stellite to prevent ball variance. The sewing ring had knitted Teflon with polypropelene cloth. The valve had good durability and hemodynamics. Starr and Edwards founded a company – American Edwards Laboratory, in 1966 and manufactured the valves in the early stages (Figure 1 and 2).
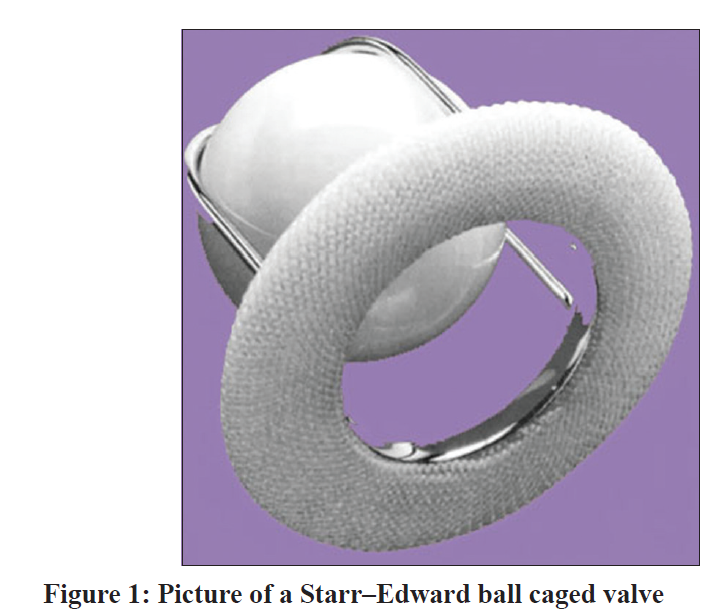
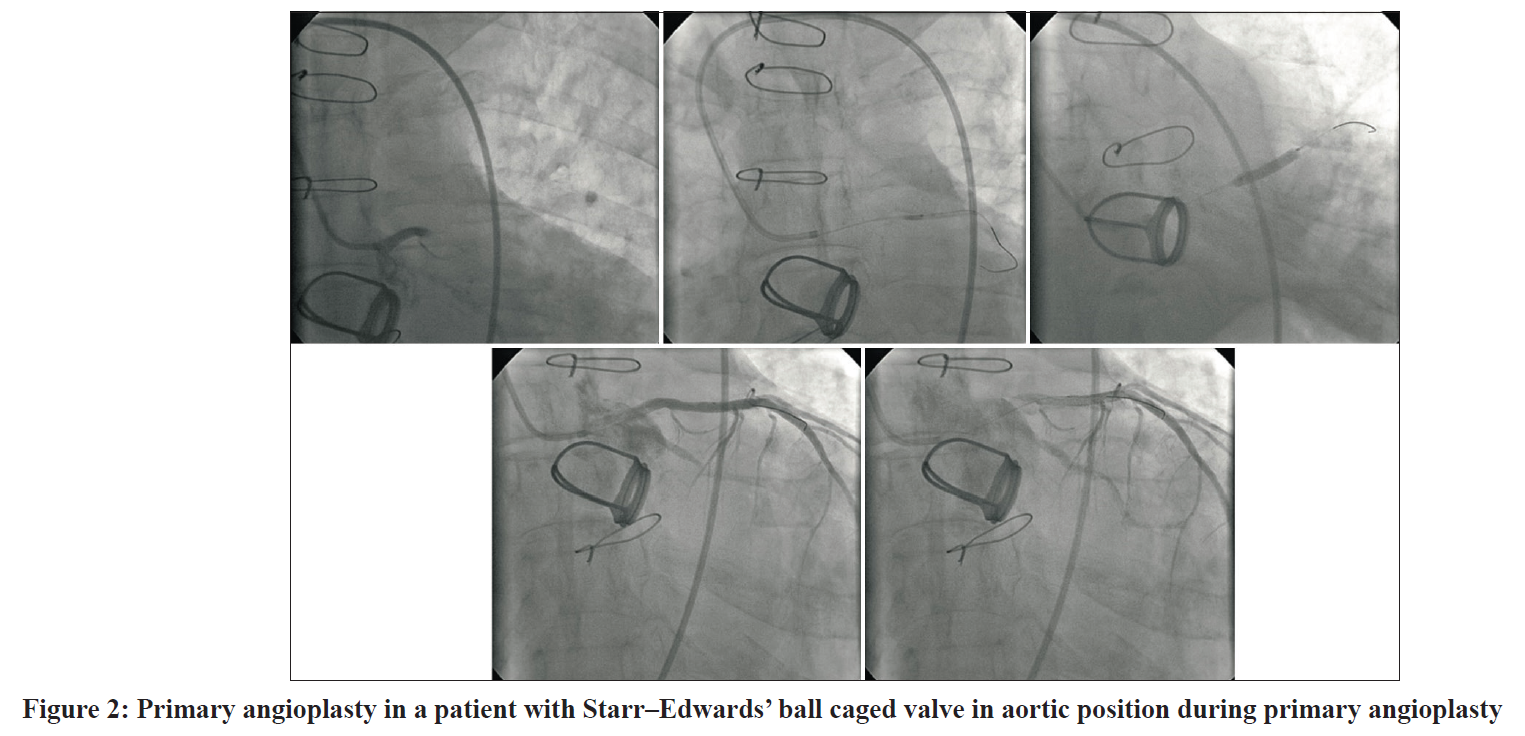
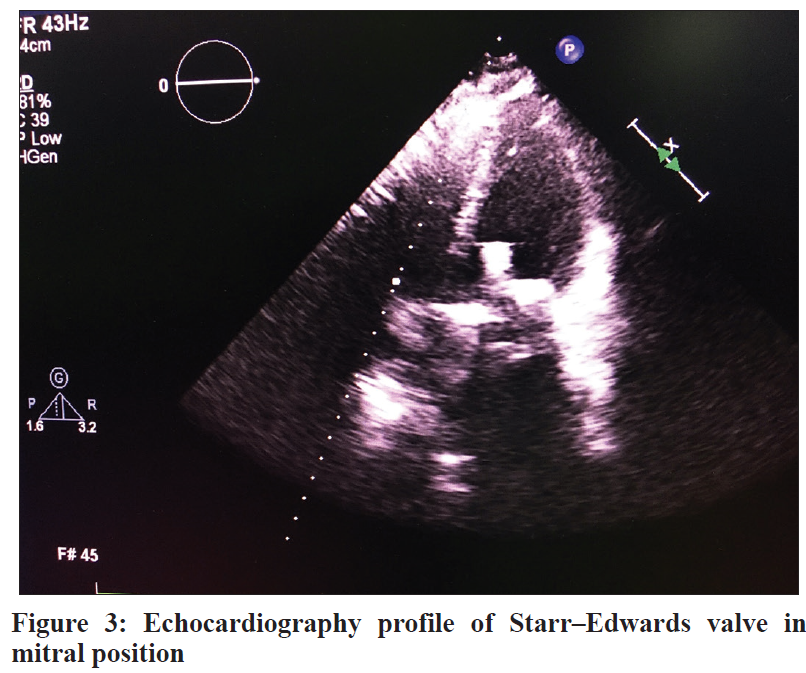
It was further marketed and developed by Edwards Lifesciences till the late 2000s. The mitral prosthesis model 6120 and aortic prosthesis models 1200 and 1260 persisted till its discontinuation. The usage of Starr Edwards’ valves, known for their excellent long-term durability, was common in India and neighbouring countries in the late 1980 and 90s and was stopped in clinical use in the late first decade of 2000. Many of the implanted patients during that time are doing well these days with these valves. These valves were often criticized for their bulky size (Figure 1-3)and also the higher thrombogenicity, which the tilting disc valves have largely reduced in the general purview.
WHY WAS THE STARR EDWARD VALVE ELIMINATED?
At present the Starr Edwards valve is eliminated from the market in the early first decade of 2000. Extensive analysis of the published articles concerning increased thrombogenicity shows the claims are attributed to the earliest and first-generation Starr Edwards (SE) valves. In the subsequent years, many minor modifications were made to the SE valves.[2] By computational fluid-flow dynamics, turbulent annular shear stress has been shown to reach up to 3500dyn/cm2 in ball-caged valves. In contrast, in the tilting disc prosthesis, the maximum turbulent shear stress was 1850dyn/cm2 which is seen at the minor orifice.[3] Though this could be seen as a disadvantage, this hemodynamic could also give a potential vantage point by clearing or ‘self-cleaning’ any microthrombi which happens spontaneously. There are general claims that thrombogenicity is higher in ball-caged valves.[4] However, large studies substantiating the claim with a head-to-head comparison between the valves are not available in reality. In a small single-centre study involving 12 patients with Starr Edwards valve replacement and 50-year follow-up, 66.6 percent survived. Among the patients with mortality, the event started occurring only after 7500 days after implantation.[5] An article which evaluated the Starr Edwards valves was published in 1983, which included 509 patients followed up for 10 to 15 years. In this paper, any event- free all valve-related morbidity and mortality was 38±3%. 22 percent of hospital deaths and 27% of late deaths were SE valve related. A small study in 1991 comparing the Starr Edwards (149 patients) and 87 patients with St Jude valve prosthesis showed better 5 yr. survival statistics with St Jude valve - 94% Vs. 86% for Starr Edwards valves. The study was small, and it was not matched with numbers.[6] In the aortic position the for the silastic ball valve cumulative freedoms at 10 and 25 years were 59 and 20% from all deaths (crude survival), 85 and 80% from thromboembolism, 87 and 70% from bleeding, 98 and 94% from endocarditis, 96 and 95% from redo AVR, and 68 and 51% from all valve-related complications joined (Lund). [7] The published rate of ball variance in the aortic position was 6% and 0% in the mitral position.[8] In the initial stages, the results published by Starr and his team show the patient survival rates were 80%, 58%, and 50% at 5, 10, and 15 years, respectively.[9] Also the report by Starr [10] in 1985, about 110 patients have shown good results, with valve thrombosis rates nearing zero percent and embolism rates of 2.9%/patient years in the mitral position and 1.8% in aortic models. The report also shows a significant improvement in the results from 1973 to 1984, compared to the period of implantation from 1965 to 1972. A study by the team of Christian Bernard published in 1977 shows thromboembolic free event rates, including three models of Starr Edwards, was about 71% at five years; and interestingly, a subset of 52 patients who were not receiving anticoagulants for various reasons also almost had a similar thromboembolism free rates at five years.[11]
In the clinical experience of the author, patients with the SE valves were performing well in the past and in the current juncture; and some patients also come for regular follow-up these days, and the higher thrombogenicity [12] claimed compared to patients with tilting disc valves and also stuck valves, was not seen. The fact is, in some of the patients who have lost follow-up, who had discontinued anticoagulants, and tend to show up in later days - about weeks/months and in some cases, even after many years of non-compliance with anticoagulants, the problems of stuck valve were not seen in the clinical observation of the author. Also, this observation of noncompliance with anticoagulants was not uncommonly seen in the past, even in the mitral valve position of Star Edwards valves. Anecdotal case reports of normal valve functioning after medications default does exist with all types of valves, but the observation mentioned above is a significant number.
Before the stage of exit from the clinical use, the Starr Edwards valves were used in numerous patients and hospitals in the lower socioeconomic strata population in the general hospitals of the Asian countries, and these patients’ sudden cardiac deaths were not known. Also, the primary valve failures after implantations were very few or hardly ever seen. And these patients being from a lower socioeconomic status were also prone to drug default. A thorough discussion from the older generation of cardiovascular surgeons and cardiologists performing echocardiography will shed more light on these caged ball valves and their abrupt ending. Also, during routine follow-up, the usually criticized ball-caged valves for the left ventricular outflow tract (LVOT) tract causing LVOT obstructions were not seen in the echocardiography. Clinically significant LVOT gradients elevations similar to hypertrophic cardiomyopathy were not observed. In the opinion of the author, when the tilting disc valves arrived, the generation of the cardiovascular surgeons was also changed by their age and retirement processes, and the newer generation of cardiovascular surgeons shifted to tilting disc valve usage. Also, as indicated, the claims of higher thrombogenicity of SE valves are primarily concerning the initial models in the early 1960s, and the initial bad reputation silhouetted the SE valves and passed on to the subsequent generation of Starr Edwards valves. Many modifications were performed in the later generations of Starr Edwards, including heat treatment of the silastic ball at high temperatures to prevent ball variance.[1] The silastic ball was changed to stellite alloy ball valve in the later days to prevent ball variance. In some patients presenting with subtherapeutic INR during the routine follow-up also, the thrombogenicity was not seen. Small and older published studies also do not indicate higher thromboembolism.
Freedom from thrombo-embolic events after the implantation of SE valves in the aortic position varied from 76% to 87% at 10 years and 90.8% at 5 years depending primarily on the time frame of the studies, which likely reflected evolutions in anticoagulation protocols.[13-15] In aortic position the mortality is 12±2 in 10 years.[14] Hence, it could be primarily the generation change and the mindset of the cardiovascular surgeons who adopted the tilting disc valves due to the thin profile and physiological appearance of the tilting disc valves than the actual benefit observed. Also, the LVOT (left ventricular outflow tract) obstructions were not seen or over-emphasized, and the pannus formation was also not high in the SE valves.
The traditional recommendation of higher therapeutic INR of 3 to 4 was also based on the older or initial generation SE valves, and it was not supported by any large or randomized controlled studies.
AREAS OF CONTROVERSIES
When an extensive internet search was performed, even small recent studies were not available supporting the claim of increased thrombogenicity. Some of the studies showing head-to-head comparisons were small. A study by Zouaoui et al16 showed increased mortality in patients with Starr Edwards valves in comparison with St Jude’s valve. In this study, the comparison was performed with two groups - Starr Edwards, 127 patients, and 109 patients on St Jude valves. In this study, the 30-day hemorrhagic, conduction abnormalities, infections, pleuropulmonary complications, and overall non-prosthetic related complications were significantly lesser in patients on Starr Edwards valves though the late mortality was higher in Starr Edwards (9.2%) compared to St Jude valves (4.6%). In this study, 67.7% of patients with Starr Edwards had mitral valve disease Vs. 53.2% of patients on St Jude valve.[16] In the aortic valve position, the Starr Edwards had a higher survival rate. 14 In one another study involving 122 patients in each arm, the results of Starr Edwards and St Jude valves were the same, with the baseline characteristics matched in both arms.[17] In a study by Sezai A et al,[18] comparing the Starr Edwards, St Jude, and ATS valves, the results favouring St Jude valves though the results were comparable and Starr Edwards’ patients the longest mean follow-up of 16.9 years, whereas patients with St Jude valves had a follow up of 11.5 years. The survival rates after 10, 20, and 30 years were 62.3, 39.4, and 19.9% after aortic valve replacement and 75%, 36.5%, and 22.6% after mitral valve replacement. The freedom from all valve related complications including valve related causes of death after aortic and mitral valve replacements were – 70% at 10 years, 55.8% at 15 years, 39.4% at 20 years and 19% at 30 years.[19] The 416 patients in this study were enrolled between 1963 and 1977.[19] A large study20 involving 4480 patients with St Jude valves, and the total follow-up was 7±5 years, and patients’ freedom from late mortality was 61% at 10 years, 42% at 15 years, 28% at 20 years, and 20% at 24 years follow-up. The patients were enrolled between 1977 and 2002.[20]
The lack of large studies and randomized controlled studies evaluating the Starr Edwards valves and other valves has also been acknowledged by studies.[21] Worldwide so far more than half a million SE valves have been implanted so far.[22] The higher thrombogenicity by the SE valves have not been a clinical observation by the author. Because of the less contact of the ball with surrounding structures, unlike the joints in tilting disc valves, the pannus formation is also lesser. Hemolysis and valve thrombosis rates were reported as low as 0.1% and 0.06% per patient years, respectively.[9]
Compared with St Jude’s valve, the doppler gradient was highest in Starr Edwards and lowest in St Jude. Mitral regurgitation was in the opposite direction – highest with St Jude, though both the gradients and regurgitation were acceptable levels of physiology in all the tested valves.[23] In comparison with carbomedics valve, for the carbomedics valve the peak pressure gradient (PPG) was 26.1 ± 8.2 mm Hg, and the mean pressure gradient (MPG) was 14.7 ± 5.1 mm Hg; in the Starr-Edwards valve, the PPG was 32.8 ±9.1 mm Hg and the MPG was 19.5 ± 5.6 mm Hg.[24] In another study, the peak calculated transvalvular aortic gradients in normal subjects were 22 ± 10 mm Hg in 33 Björk-Shiley valves, 23 ± 10 mm Hg in 27 porcine valves and 29 ± 13 mm Hg in 6 Starr-Edwards valves.[25] Small studies indicate mildly increased gradients in Starr Edwards compared to St Jude. However, in these studies, the number of Starr Edwards valve patients tested was <10 numbers. [26,27] A large echocardiography study shows mild differences in flow velocities in the aortic position, 3.2±0.6 m/s Vs. 2.5±6 m/s in SE and St Jude valves, respectively.[28] In a large study involving all types of valves, the gradients across the valves were not significantly different across various valve types.[29]
Another concern that eliminated the SE valves was the left ventricular outflow tract (LVOT) obstruction because of the larger size. When an internet search was performed, only three studies showed this concern. One was two case reports,[30,31] another was an animal study involving five heart models and measuring left ventricular outflow tract after SE valve implantation;[32] and the third was a study published in 1973 concluding the possibility of low cardiac output syndrome in 4 patients in a sub-group of 7 patients with smaller left ventricular outflow tract.[33] Hence, an extensive study on LVOT gradients is not available comparing the valves, especially when the implantation worldwide has crossed half a million to date.
The attractive thin profile of the tilting disc valves, a higher market cost and inadequate data, unnatural look of caged ball valves and the thrill of the new arrival of tilting disc valves changed the mindset and emotions of the next generation of younger cardiovascular surgeons. Other parameters like less experience in the initial stages with cardiovascular physicians regarding warfarin and other similar anticoagulants like drug interactions etc., general paucity of data concerning thromboembolism and bleeding, and the late identification of mechanism of warfarin, i.e., epoxide reductase inhibition in the liver were demonstrated in 1978, could have influenced the early clinical outcomes. It is indeed difficult for any valve to fulfill the ‘nine commandments’ for best performance mimicking the native valves.[2]
Nowadays, point-of-care (POC) devices are available for self-testing of INR. Bench testing of the valves is possible in the present times, which can give more information about the valves’ performance to certain exact though the exact physiology in vivo is slightly modified by biological processes like endothelization, pannus and biofilm formation etc. which cannot be studied invitro.
A similar mindset effect is also seen among cardiovascular surgeons for some of the excellent procedures like closed mitral valvotomies, which are going out of vogue these days. Elliot Cutler and Samuel Levine performed the first commissurotomy in 1923 in Peter Bent hospital Brigham hospital in Boston, and later the technique had minor modifications. Closed mitral valvotomies (CMV) yield excellent results in preserving natural anatomy when mitral balloon valvotomy is not suitable.[3] CMV also reduces the need for long-term anticoagulation. Post CMV during echocardiography in long axis and 4-chamber views, the mitral valve tends to be narrow, but the real caliber is visualized in the short axis profiling only. CMV is often replaced by prosthetic valve insertion by the current generation of cardiovascular surgeons. Hence, whenever feasible, the time-tested Starr Edwards valve needs to be evaluated in the present context in a blinded fashion with extensive long-term data and in-depth analysis, especially in the community at risk for non-compliance with long-term oral anticoagulants. The author feels the elimination of the Starr Edwards valves from regular use with inadequate data and hemodynamics understanding needs more evaluation and possible revival of the valve, at least in a few patients who insist on long-term durability.
FUTURE RESEARCH PERSPECTIVES
For the mechanical prosthetic heart valves, warfarin or related anticoagulants is the treatment of choice. Non-vitamin K antagonist oral anticoagulants (NOVCs) are not very effective in these valves, with a higher rate of prosthetic mechanical heart valve failure, irrespective of the prosthetic valve models.[34] The Re-Align study, which was prematurely ended, had a majority of patients on high doses of dabigatran- 220mg twice daily, and the mean trough level in the study was >100ng/ml in the majority of the patients, and the minimum was about 75ng/ml. The target trough level of dabigatran in the study was 50ng/ml. Asprin or clopidogrel can potentiate the action of dabigatran/NOVCs.[35,36] It is worthwhile to evaluate moderate doses of the novel oral anticoagulants with Starr Edwards valves in animal models, as their ‘self -cleaning’ hemodynamics are different, especially with smaller doses of aspirin or clopidogrel on a daily or alternate day basis. This will be better to study 2 to 3 weeks of valve implantation, which is usually required for endothelization.
CONCLUSION
The traditionally durable and well-performing Starr Edwards mechanical ball caged heart valves were withdrawn from the market and clinical use in a preliminary and abrupt context of time. Hence, extensive studies are required to identify the benefits of the latest generation of the Starr Edwards valves for better understanding and revival of its clinical use.
References
- De Martino A, Milano AD, Barbera MD, et al. The Caged-Ball Prosthesis 60 Years Later: A Historical Review of a Cardiac Surgery Milestone. Tex Heart Inst J. 2022;49 (2): e207267.
- Annete MM. The development of Starr Edwards valves. Tex Heart Inst J 1998;25:282-93.
- Dasi L, Simon H, Sucosky P, et al. Fluid mechanics of artificial heart valves. Clinical and Experimental Pharmacology and Physiology. 2009;36(2):225-237.
- Bloomfield P. Choice of heart valve prosthesis. Heart. 2002;87(6):583-589.
- Raymundo-Martinez G, Gopar-Nieto R, Araiza-Garaygordobil D, et al. Risk Factors for Starr-Edwards Prosthetic Valve Dysfunction: New Insights into an Old Prosthesis. World Journal of Cardiovascular Diseases. 2019;09(03):149-157.
- Kafsi N, Trabelsi S, Acar P, et al. Comparaison des résultats à long terme des prothèses de Starr et de Saint-Jude en position mitrale [Comparison of long-term results of the Starr and Saint-Jude mitral valve prostheses]. Arch Mal Coeur Vaiss. 1991 Nov;84(11):1523-7. French.
- Lund O, Pilegaard HK, Ilkjaer LB, el al. Performance profile of the Starr-Edwards aortic cloth covered valve, track valve, and silastic ball valve. Eur J Cardiothorac Surg. 1999 Oct;16(4):403-13. doi: 10.1016/s1010-7940(99)00249-3.
- Starr A, Grunkemeier G. Beyond 24 years with the aortic Starr-Edwards Silastic Ball Valve: A valve of the past? — no! European Journal of Cardio-Thoracic Surgery. 1993;7(3):113–4.
- Macmanus Q, Grunkemeier G, Thomas D, et al. The Starr-Edwards model 6000 valve. A fifteen-year follow-up of the first successful mitral prosthesis. Circulation. 1977;56(4):623–5.
- Starr, A. The Starr-Edwards valve. Journal of the American College of Cardiology. 1985; 6(4): 899–903.
- Forman R, Beck W, Barnard CN. Results after mitral valve replacement with cloth-covered Starr-Edwards prostheses (models 6300, 6310/6320, and 6400). Heart. 1978;40(6):612–6.
- Edmunds LH Jr. Is prosthetic valve thrombogenicity related to design or material? Tex Heart Inst J. 1996;23(1):24-27.
- Orszulak TA, Schaff HV, Puga FJ, et al. Event status of the Starr-Edwards aortic valve to 20 years: a benchmark for comparison. Ann Thorac Surg. 1997 Mar;63(3):620-6.
- Miller DC, Oyer PE, Mitchell RS, Stinson EB, et al. Performance characteristics of the Starr-Edwards Model 1260 aortic valve prosthesis beyond ten years. J Thorac Cardiovasc Surg. 1984 Aug;88(2):193-207.
- Bessell JR, Gower G, Craddock DR. Thirty years experience with heart valve surgery: isolated aortic valve replacement. Aust N Z J Surg. 1996 Dec;66(12):799-805.
- Zouaoui W, Ouldzein H, Drissa MA, et al. Résultats à Court et long terme du remplacement valvulaire mitral par prothèse mécanique à bille et à ailettes (à propos d’une série de 236 patients consécutifs avec un suivi moyen de 11 ans). Annales de Cardiologie et d'Angéiologie. 2009;58(2):86–93.
- Murday AJ, Hochstitzky A, Mansfield J, et al. A prospective controlled trial of St. Jude versus Starr Edwards aortic and mitral valve prostheses. Ann Thorac Surg. 2003;76(1):66-73; discussion 73-4.
- Sezai A, Shiono M, Hata M, et al. 40 Years experience in mitral valve replacement using Starr-Edwards, St. Jude Medical and ATS valves. Ann Thorac Cardiovasc Surg. 2006 Aug;12(4):249-56.
- Gödje O. Thirty Years Survival after double valve replacement with Starr-Edwards prostheses in aortic and mitral position. European Journal of Cardio-Thoracic Surgery. 1997;11(2):391–3.
- Emery RW, Krogh CC, Arom KV, et al. Th St Jude Medical cardiac valve prosthesis:A 25 year experience with single valve replacement. Ann Thorac Surg. 2005;79:776-83.
- Bonow RO, Carabello B, DeLeon AC, et al. ACC/AHA practice guidelines.Guidelines for the management of patients with valvular heart disease. J Am Coll Cardiol. 1998; 32:1486–588.
- Hirji SA, Kaneko T, Aranki S. The revolution and evolution of mechanical valves: The ball has left the cage. The Journal of Thoracic and Cardiovascular Surgery. 2018;155(5).
- Masotti C, De Castro C, Aquilina M, et al. Doppler hemodynamic characteristics of four widely used aortic valve prostheses. Minerva Cardioangiol. 1990;38(11):461-71.
- Chakraborty B, Quek S, Zee D, et al. Doppler Echocardiographic Assessment of Normally Functioning Starr-Edwards, Carbomedics and Carpentier-Edwards Valves in Aortic Position. Angiology. 1996;47(5):481-489.
- Williams GA, Labovitz AJ. Doppler hemodynamic evaluation of Prosthetic (Starr-Edwards and Björk-Shiley) and bioprosthetic (Hancock and Carpentier-Edwards) cardiac valves. The American Journal of Cardiology. 1985;56(4):325–32.
- Grigg, L., Fulop, J., Daniel, L., et al. Doppler Echocardiography Assessment of Prosthetic Heart Valves. Echocardiography. 1990; 7: 97-114.
- Panidis IP, Ross J, Mintz G. Normal and Abnormal Prosthetic Valve Function as Assessed by Doppler Echocardiography. JACC.1986; 8(2):317-26.
- Miller FA, Callhan JA, Taylor et al. Normal aortic valve prostheses hemodynamics: 609 prospective Doppler examinations. (Abstract) Circulation 1989; 80(Suppl II): II–169.
- Rosenhek R, Binder T, Maurer G, et al. Normal values for Doppler echocardiographic assessment of heart valve prostheses. J Am Soc Echocardiogr. 2003;16(11):1116-27.
- Pelikan PCD, Chew PH, Fortuin NJ, et al. Left ventricular outflow obstruction caused by a Starr-Edwards mitral prosthesis. The American Journal of Cardiology. 1983;52(5):652–3.
- Shepherd RL, Glancy DL, Stinson EB, et al. Hemodynamic confirmation of obstruction to left ventricular inflow by a caged-ball prosthetic mitral valve. Case report. J Thorac Cardiovasc Surg. 1973 Feb;65(2):252-4.
- Jett GK, Jett MD, Barnhart GR, et al. Left ventricular outflow tract obstruction with mitral valve replacement in small ventricular cavities. The Annals of Thoracic Surgery. 1986;41(1):70–4.
- Nanda NC, Raymond G, Pravin SM, et al. Echocardiographic assessment of left ventricular outflow width in the selection of mitral valve prosthesis. Circulation. 1973;48(6):1208–14.
- Eikelboom JW, Connolly SJ, Brueckmann M, et al. Dabigatran versus warfarin in patients with mechanical heart valves. New England Journal of Medicine. 2013;369(13):1206–14.
- Mendell J, Lee F, Chen S, et al. The effects of the antiplatelet agents, aspirin and naproxen, on pharmacokinetics and pharmacodynamics of the anticoagulant edoxaban, a direct factor Xa inhibitor. Journal of Cardiovascular Pharmacology. 2013;62(2):212–21.
- Kitano D, Migita S, Li Y, et al. Effect of rivaroxaban and clopidogrel combination therapy on in-stent responses after Everolimus-eluting stent implantation in a porcine coronary model. Journal of Atherosclerosis and Thrombosis. 2022;29(1):69–81.
