Full HTML
Life-threatening side effects of Amphotericin B
Ali Ibrahim Rahil
Author Affiliation
From Senior Consultant, Department of Medicine, Hamad General Hospital, Doha, Qatar
Abstract
A 22-year-old Indonesian woman was admitted through the emergency department with a 10-day history of fever associated with chills. Other medical history was unremarkable. On examination, she appeared ill; BP 95/60 mmHg, pulse 105/min, and temperature 39.5°C. Abdominal examination showed splenomegaly; examination of the heart, lungs, and nervous system was unremarkable.
DOI: 10.32677/yjm.v1i2.3703
Pages: 112-113
View: 5
Download: 12
DOI URL: https://doi.org/10.32677/yjm.v1i2.3703
Publish Date: 29-03-2025
Full Text
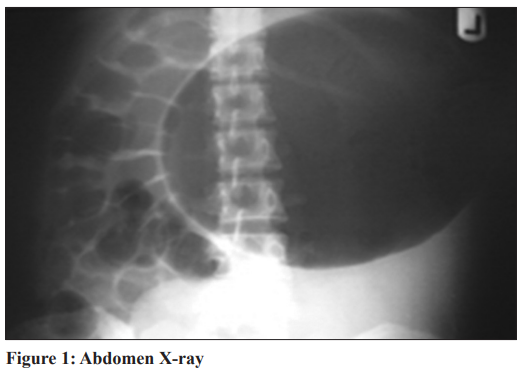
Initial investigations showed hemoglobin level of 9.0 g/dL, total leukocyte count 5000/µL with a normal differential, platelet count of 112,000/µL, and ESR of 66 mm/h. Blood chemistry, liver profile, and coagulations studies were within normal limits. Malaria parasite smear was negative, urine dipstick and microscopy were normal. Blood culture showed candidemia, but urine and stool cultures were negative. Chest and abdominal radiographs were normal. A tuberculin skin test was negative. Apart from splenomegaly, abdominal ultrasound was unremarkable. Although bone marrow aspiration and biopsy showed normal study, leishmaniasis was put in the differential diagnosis. Amphotericin B was started to cover the candidemia and the suspected leishmaniasis. On the 3rd admission day, the fever continued, and the patient developed abdominal distension with complete constipation and vomiting. Radiography of the abdomen and ECG was performed.
Questions:
1. What do the X-ray and ECG show?
2. Which blood test would you recommend?
3. Spot the diagnosis based on the given images.

Answer:
1. ECG shows prominent U wave, while the abdomen X-ray shows gastric dilatation.
2. Serum electrolytes including potassium and magnesium
3. Amphotericin-induced hypokalemia.
DISCUSSION
The patient in the vignette presented with acute febrile illness and splenomegaly and her workup revealed candidemia which is the commonest manifestation of invasive candidiasis, which might disseminate to many areas in the body including the eye causing endophthalmitis, and the heart causing endocarditis [1]. Therefore, prompt initiation of antifungal agents in addition to source control and monitoring with daily cultures to ensure clearance of candidemia is crucial as even a 1–2 days delay in starting treatment is associated with a doubling in risk of mortality [2]. The patient was treated with intravenous amphotericin B at a dose of 4 mg/ kg. On the 3rd day following initiation of amphotericin, the patient developed paralytic ileus manifested as vomiting and constipation and X-ray of the abdomen revealed marked gastric dilatation. Serum electrolytes showed potassium level of 2.5 mmol/L and magnesium of 0.5 mmol/L. Electrocardiogram showed sinus rhythm with prominent U-waves. The diagnosis of amphotericininduced hypokalemia was made. Amphotericin was discontinued and the treatment was switched to anidulafungin along with the replacement of potassium and magnesium with restoration of normal serum electrolytes level and improvement in her symptoms. Amphotericin has been considered as the standard antifungal agent for the past 6 decades and has broad spectrum of activity. However, amphotericin does have several serious adverse effects particularly nephrotoxicity associated with reduced glomerular filtration rate and electrolytes disturbance of which hypokalemia (70–90%) and hypomagnesemia (58%) are considered the commonest [3]. Hypokalemia is induced by renal tubular injury causing potassium leak [4]. Hypokalemia may lead to metabolic consequences including life-threatening arrhythmias and rhabdomyolysis, in addition, paralytic ileus may also occur leading to constipation and vomiting with dilated stomach and bowel loops. This case emphasizes the importance of closely monitoring serum electrolytes and renal function in patients treated with amphotericin to avoid such risk particularly in patients with risk factors such as those with high body weight (>90 kg), using diuretics or other nephrotoxic agents and patients with baseline renal impairment [5].
References
1. Lashof AM, Rothova A, Sobel JD, et al. Ocular manifestations of candidemia. Clin Infect Dis 2011;53:262-8.
2. Magill SS, Edwards JR, Bamberg W, et al. Multistate point-prevalence survey of health care-associated infections. N Engl J Med 2014;370:1198-208.
3. Karimzadeh I, Khalili H, Farsaei S, et al. Role of diuretics and lipid formulations in the prevention of amphotericin B-induced nephrotoxicity. Eur J Clin Pharmacol 2013;69:1351-68.
4. Laniado-Laborín R, Cabrales-Vargas MN. Amphotericin B: Side effects and toxicity. Rev Iberoam Micol 2009;26:223-7.
5. Fisher MA, Talbot GH, Maislin G, et al. Risk factors for amphotericin B-associated nephrotoxicity. Am J Med 1989;87:547-52.
