Full HTML
The impact of implementing a pharmacy triage system on the reduction of patients’ waiting time in the fourth floor outpatient pharmacy at Hamad General Hospital, Qatar
Abdel-Monem Badawi Yousif, Rania Obaydat, Abdel-Rahman Abbas, Adhem Rezk
Author Affiliation
From Pharmacist, Department of Pharmacy, Hamad General Hospital, Doha, Qatar
Abstract
Background and Objectives: The outpatient department (OPD) pharmacy is a section of the hospital pharmacy that helps patients obtain their prescribed medications. However, on-time delivery of medications and patients’ convenient access to the pharmacy are the hallmarks of a well-designed health-care system. Therefore, he aim of this study was to develop a pharmacy triage tool to improve patient flow and reduce waiting time in the fourth-floor pharmacy at Hamad General Hospital (HGH). Methods: This prospective and observational study was conducted on 14,740 patients who attended the OPD pharmacy (HGH, Qatar) between January 15, 2022 and March 15, 2022. This prospective and observational study consisted of three periods: A root cause analysis, a pre-intervention period of 1 month (January 15, 2021–February 14, 2021) and an intervention period of 1 month (15 February–15 March). We developed a pharmacy triage tool to improve patient flow and reduce waiting time by identifying patients who need their medications to be dispensed, as well as classifying patients to get the right patient to the right place and implementing a patient flow system to improve efficiency spends in pharmacy queues. Results: The results of this study showed that the use of the triage system in the pharmacy reduced the average waiting time of patients from 50 min to 15 min. The results were statistically significant at p<0.0001. Conclusion: We concluded that applying the pharmacy triage tool improved quality of services in health-care systems and decreased waiting time in the OPD pharmacy. The pharmacy triage tool is a new approach to enhancing the quality of healthcare and leads to an increase in the efficiency of OPD pharmacies.
DOI: 10.32677/yjm.v1i2.3667
Keywords: Hamad general hospital, Outpatient pharmacy, Qatar, Triage tool, Waiting time
Pages: 82-84
View: 5
Download: 10
DOI URL: https://doi.org/10.32677/yjm.v1i2.3667
Publish Date: 29-03-2025
Full Text
The waiting time for a patient at an outpatient department (OPD) pharmacy to obtain his medications is a problem in most countries and causes patient dissatisfaction. Most patients leave the various OPD departments at various times and randomly arrive at the pharmacy where they often experience long waiting times, and this long length of stay leads to overcrowding in the hospital waiting area, which is majorly unpleasant for any patient [1].
The World Health Organization has identified patient waiting time as one of the most important measurements of a responsive health-care system. A lengthy waiting time has long been considered frustrating to patients and thus appears to be a consistent and significant potential cause of patient dissatisfaction. A strong inverse relationship between patient satisfaction and length of waiting time has been demonstrated by many studies. Efforts to find health-care solutions to reduce the waiting time become obvious, as a growing number of reports from different countries appeared in the literature [1-3].
Hamad General Hospital (HGH) is the largest tertiary hospital in Qatar in which the OPD pharmacy shares the same waiting area with other clinics. Prolonged waiting time may lead to an increase in the crowdedness of a small waiting area; therefore, this may have an effect on the COVID-infection control measures during the pandemic and lead to patient dissatisfaction [4]. No previous quality work has been conducted to assess this problem in HGH. The aims of this study were to (a) evaluate the length of OPD pharmacy waiting times, (b) perform a root cause analysis to identify factors contributing to the long waiting times, and (c) to assess the impact of implementing a pharmacy triage system on the reduction of patients’ waiting time in the fourth floor OPD pharmacy in HGH.
PATIENTS AND METHODS
Study Setting and Population
This study was conducted on 14,740 patients who attended the fourth floor OPD department pharmacy at HGH between January 15, 2022, and March 15, 2022. The fourth floor OPD dispensed medications to the patients coming from various clinics in the fourth floor, including the internal medicine and nephrology clinics. Patients were randomly observed without prior notification. All hospital staffs not involved in the study were not informed about the existence of the study. We obtained an administrative approval from the Head of the Department of Pharmacy at HGH.
Study Design and Data Collection
This prospective and observational study consisted of three periods: A pre-intervention period of 1 month (January 15, 2021– February 14, 2021), a root-cause analysis and an intervention period of 1 month (February15–March 15).
Intervention
In this study, we developed a triage tool to identify patients who need to have their medications dispensed in the fourth floor OPD pharmacy according to the specified known OPD clinics, and a patient flow project was implemented to improve the efficiency of dispensing and counseling and to reduce the waiting time in the HGH fourth floor pharmacy.
Measure of Intervention
The waiting time (as primary outcome measure) in the OPD pharmacy was defined as the time between receiving the queue number at the counter to the time of calling a patient for drug dispensing using the Queue Management System (QMS) [2]. For the secondary outcome measure (source of prescription): Data were collected for the patients from other facilities before and after the triage system implementation. Data for patients without medication refills and those with expired health cards were also collected.
Data Analyses
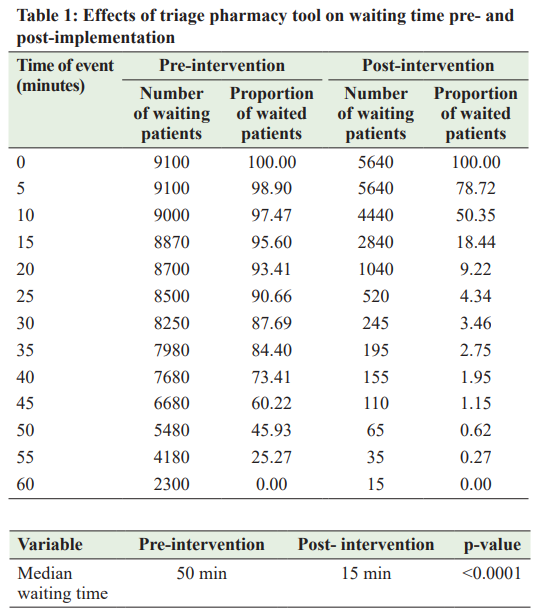
Data were collected 1 month (January 15–February 14) before and 1 month (February 15–March 15) after implementation of pharmacy triage tool using QMS. The collected data on waiting times for both periods were classified into different waiting time frames, starting with a 5-min waiting time, then each waiting time frame increased by 5 min until a 60-min waiting time frame was reached to compare the numbers of patients who still waiting to obtain their medications from those who have obtained the medications. A Mann–Whitney U test was used to compare the differences between median wait times of the two periods. We obtained an administrative approval from the Head of the Quality Management Unit of the Department of Pharmacy at HGH.
RESULTS
Pre-interventional and Interventional Periods
The waiting times of patients at the OPD pharmacy before and after the intervention are described in Table 1. This study showed that the pharmacy triage system effectively reduced the average waiting time of patients from 50 min to 15 min. The results were statistically significant at p<0.0001.
Root-cause Analysis
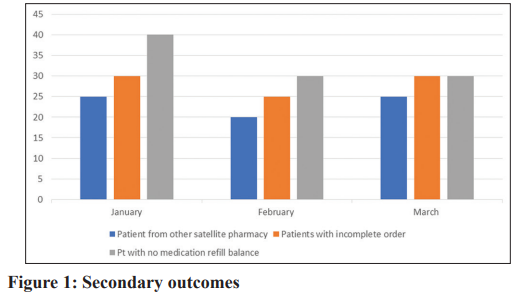
This study identified possible causes of prolonged waiting times for compounded prescriptions, which include the following: (a) Lack of patient categorization; all patients are served from the same window. Every patient consumes the pharmacist’s time differently. For example, the special needs patients and low-immunity patients require more time since the pharmacists need to thoroughly explain the prescription(s). In addition, the refill patients make the crowd worse, and they only need their medications to be refilled without receiving instruction. (b). The pharmacy serves all OPDs from all clinics, and they all attend the same small area in the OPD pharmacy to obtain their medication, which results in long waiting times at the pharmacy. (c) The pharmacy’s space is small and tight compared to the number of patients served and the number of medicines stored, which is uncomfortable for both patients and pharmacists. (d) A group of patients attend to the OPD pharmacy from external health care center and this may extend the waiting time. Fig. 1 describes the secondary outcome measure in both the pre-intervention and the post-intervention periods.
DISCUSSION
Many studies in the literature adopted different managerial tools and techniques to solve health-care services problems and to improve quality. For instance, a study conducted by Arafeh et al. [5] implemented Six Sigma processes as an improvement methodology to reduce patients’ waiting time in an OPD pharmacy located in a local hospital that specialized in cancer treatment in Pakistan. The study found various improvement opportunities that can reduce patients’ waiting time by 50%. Ahmad et al. [6] studied the patients’ waiting time and doctor consultation time in a primary health-care clinic and formulated strategies for improvement. The data were collected and entered using the statistical software SPSS for analysis. They have found that to improve the waiting and consultation time, they should increase the number of staff at the registration counter, enforce the staggered appointment system for follow-up patients, and improve the queuing system for walk-in patients. Rim et al. [7] implemented a quality assessment at an OPD pharmacy services call center by the following: (1) decreasing the call rejection rate, (2) improving the speed of answers, (3) increasing firstcall resolution, (4) centralizing all specialty pharmacy and prior authorization calls, (5) increasing labor efficiency and pharmacy capacities, (6) implementing a quality evaluation program, and (7) improving workplace satisfaction and retention of OPD pharmacy staff. The design and implementation have significantly improved the health system’s patient experiences, efficiency, and quality. Our study showed that the pharmacy triage system effectively reduced the average waiting time of patients from 50 min to 15 min. The results were statistically significant at p<0.0001, and this is better than the results of the previous studies conducted by Fahrurazi et al. [8], which resulted in lowering the waiting time in OPD pharmacy to 23 min. In addition, this system prioritizes patients who need triage indoors and patients who need triage in other appropriate facilities. More testing and more data collection continue. Appropriate results will appear in the coming months. As for the secondary results, it was shown that the application of the triage pharmacy tool reduced the number of patients with no medication refill balance from 40 patients in January to 30 patients in February and March. As well as reduced the patients with incomplete orders from 30 patients in January to 25 patients in the next month.
The short follow-up period is the main limitation of this study. In addition, as this was a hospital-based study, the effectiveness of our approach may not be generalizable. However, our results are promising and represent the first step in the application of this project in other hospitals in Qatar.
CONCLUSION
We conclude that applying the pharmacy triage tool has improved quality of services in health-care systems and decreased waiting time in OPDs’ pharmacy. The pharmacy triage tool is a new approach to enhancing the quality of healthcare and leads to an increase in the efficiency of OPD pharmacies. We recommend conducting more studies on the triage system in more than one health facility and for longer periods of time to find out the results related to the patient and whether its use positively affects patient and staff satisfaction.
AUTHORS’ CONTRIBUTION
Yousif AB designed the study and aided in project administration, project supervision, and manuscript writing. Obaydat R proposed the idea and aided in the literature review and data analysis. Abbas A aided in data collection, data analysis, and manuscript writing. Rezky A aided in data collection, data analysis, and manuscript writing.
References
1. Rahmawati M, Wardhani V. Key strategies to reduce waiting time in outpatient pharmacy. J Kedokteran Brawijaya 2021;31:47-51.
2. Afolabi MO, Erhun WO. Patients’ response to waiting time in an out-patient pharmacy in Nigeria. Trop J Pharm Res 2003;2:207-14.
3. Loh BC, Wah KF, Teo CA, et al. Impact of value added services on patient waiting time at the ambulatory pharmacy Queen Elizabeth Hospital. Pharm Pract 2017;15:846.
4. Sun J, Lin Q, Zhao P, et al. Reducing waiting time and raising outpatient satisfaction in a Chinese public tertiary general hospital-an interrupted time series study. BMC Public Health 2017;17:668.
5. Arafeh M, Barghash MA, Sallam E, et al. Six Sigma applied to reduce patients’ waiting time in a cancer pharmacy. Int J Six Sigma Comp Adv 2014;8:105-24.
6. Ahmad BA, Khairatul K, Farnaza A. An assessment of patient waiting and consultation time in a primary healthcare clinic. Malays Fam Physician 2017;12:14-21.
7. Rim MH, Thomas KC, Chandramouli J, et al. Implementation and quality assessment of a pharmacy services call center for outpatient pharmacies and specialty pharmacy services in an academic health system. Am J Health Syst Pharm 2018;75:633-41.
8. Fahrurazi FE, Ibrahim NH, Mafauzy NM, et al. Factors affecting waiting time in Outpatient Pharmacy at Hospital Raja Perempuan Zainab II (HRPZ II). J Pharm 2022;2:1-7.
