Full HTML
Bicuspid aortic valve, aortic coarctation, and infective endocarditis in a young adult male
Nouradden Noman Al-Jaber
Author Affiliation
From Consultant Cardiologist, Department of Medicine, Faculty of Medicine, Sana’a University, Sana, Yemen
Abstract
A 33-year-old young male patient with a history of uncontrolled hypertension was referred to my clinic due to a 2-week fever, generalized body aches, shortness of breath, and easy fatigue. Clinical examination showed a toxic dyspneic patient, but conscious and well-oriented. His blood pressure was 170/100 mm Hg, pulse 90 beat/min, respiratory rate 15/min, and the temperature was 38.6°C. Cardiac examination showed a harsh systolic murmur at the mitral area radiating to the axilla. Abdomen examination revealed moderate splenomegaly and mild hepatomegaly. The rest of the examination was unremarkable.
DOI: 10.32677/yjm.v1i2.3646
Pages: 108-109
View: 4
Download: 11
DOI URL: https://doi.org/10.32677/yjm.v1i2.3646
Publish Date: 29-03-2025
Full Text
A bedside transthoracic echocardiogram revealed mitral valve destruction with large vegetation (Fig. 1) and severe regurgitation consistent with mitral valve endocarditis (modified Duke criteria fulfilled). Furthermore, bicuspid aortic valve (BAV) was viewed (Fig. 2). Suprasternal view showed a picture consistent with aortic coarctation (CoA) (Fig. 3a and b). The patient was diagnosed with subacute endocarditis, CoA of aorta and BAV, and broad-spectrum antibiotics were started. Despite completion of antibiotics, the vegetation persisted, and he was referred to cardiac surgery unit for mitral valve replacement and surgical correction of CoA by end to end anastomosis.
BAV is the most common congenital heart anomaly in adults, and it is well recognized that aortic CoA coexists in such patient at various frequencies [1-3]. Both diseases are connected to aortic vasculopathy which is one of the most common reasons for morbidity and mortality in young patients with congenital heart disease [1]. In patients with suspected CoA, echocardiography is the imaging modality of first choice which helps to visualize the site of the CoA, its length and potential association with other cardiac pathologies (e.g., decreased left ventricular function, left ventricular hypertrophy or presence of BAV). Doppler gradients can be diagnostic, but they are not reliable, since in the case of significant collaterals, the pressure gradient may be absent before and after intervention in the CoA region [1]. Thus, the most reliable sign of a hemodynamically significant CoA is a diastolic run-off. In patients with BAV, the mainstay of diagnosis

Figure 1: Transthoracic echocardiogram. Apical 5-chamber view shows the vegetation (white arrow) on the posterior mitral valve leaflet
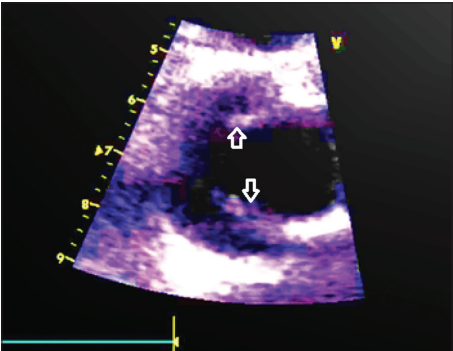
Figure 2: Transthoracic echocardiogram. Two-dimentional study shows bicuspid aortic valve (white arrows)
is echocardiography (transthoracic or transesophageal) which can provide a definitive diagnosis in the majority of patients (Fig. 2). Figures of 92% sensitivity and 96% specificity have been reported if acoustic window allows for a high-quality examination [4].

Figure 3: Transthoracic echocardiogram. Suprasternal view (a) shows turbulence flow (color Doppler) in the descending aorta. (b) Continuous wave Doppler. At the site of the coarctation indicating severe stenosis, the peak gradient = 70 mm Hg
Despite this established link, however, the impact of past CoA repair on the natural history of BAV disease is not well described. Before the advent of repair techniques, aortic dissection accounted for 19% of deaths in patients with CoA, which was amplified when BAV was also present. These patients should be followed by a cardiologist or cardiac surgeon.
References
1. Sinning C, Zengin E, Kozlik-Feldmann R, et al. Bicuspid aortic valve and aortic coarctation in congenital heart disease-important aspects for treatment with focus on aortic vasculopathy. Cardiovasc Diagn Ther 2018;8:780-8.
2. Keshavarz-Motamed Z, Garcia J, Kadem L. Fluid dynamics of coarctation of the aorta and effect of bicuspid aortic valve. PLoS One 2013;8:e72394.
3. Mizutani Y, Tada N, Masuda T, et al. Simultaneous transcatheter intervention for coarctation of the aorta and bicuspid aortic valve. J Heart Valve Dis 2017;26:481-4.
4. Mordi I, Tzemos N. Bicuspid aortic valve disease: A comprehensive review. Cardiol Res Pract 2012;2012:196037.
