Full HTML
Iatrogenic splenic infarction after embolization of an anomalous artery supplying a pulmonary sequestration: A report of a rare case
Anand Kartha, Theeb O Sulaiman
Author Affiliation
From 1Senior Consultant, Department of Medicine, Hamad General Hospital, Doha, Qatar,
2 Assistant Professor, Department of Clinical Medicine, Weill Cornell Medical College, Ar-Rayyan, Qatar,
2Senior Resident, Department of Clinical Medicine, Weill Cornell Medical College, Ar-Rayyan, Qatar
Abstract
Iatrogenic splenic infarction is a rare clinical entity that can result from various abdominal surgical and invasive procedures. We report a case of iatrogenic splenic infarction in a 29-year-old female who presented with hemoptysis and was found to have pulmonary sequestration. During the embolization of the anomalous artery supplying the pulmonary sequestration, she developed severe pain and was found to have a splenic infarction, caused by a part of the coil that dislodged during the procedure. The patient showed good response to conservative management and was discharged in good condition.
DOI: 10.32677/yjm.v1i2.3535
Keywords: Embolization, Pulmonary sequestration, Splenic infarction
Pages: 97-99
View: 5
Download: 13
DOI URL: https://doi.org/10.32677/yjm.v1i2.3535
Publish Date: 29-03-2025
Full Text
Splenic infarction is a rare condition that clinically mimics other causes of acute abdomen. It is associated with a wide variety of disorders including hematologic disorders, blood borne malignancy, blunt abdominal trauma, infiltrative disorders such as Gaucher disease, hypercoagulable state, or embolic illness [1-3]. Splenic infarction can be achieved as a therapeutic option through splenic embolization to treat traumatic splenic injury bleeding, severe portal hypertension, and to decrease intraoperative blood loss in the pre-operative process of splenectomy [4,5]. Moreover, iatrogenic splenic infarction following diverse abdominal procedures has been reported in the literature [2,6]. İn this report, we presented a very rare case of iatrogenic splenic infarction caused by a piece of the coil that dislodged during an embolization of a pulmonary sequestration. To the best of our knowledge, this is the first case of iatrogenic splenic infarction occurring during an embolization of anomalous artery supplying a pulmonary sequestration.
CASE HISTORY
A 29-year-old woman admitted to our hospital with hemoptysis. She reported a history of several episodes of coughing up small volumes of fresh blood in the past year. From then on, the patient sought medical help, but no diagnosis had been made. She denied any previous malaise, fever, night sweats, weight loss, or smoking. On examination, no notable abnormalities were found. The patient was thoroughly investigated and diagnosed as pulmonary sequestration of the medial basal segment of the right lung supplied by an anomalous systemic artery that arises from the abdominal aorta and is drained by the lower right pulmonary vein (Fig. 1). Endovascular embolization (Endovascular coiling) of anomalous artery was planned but postponed because she became pregnant. After delivery, she developed another attack of hemoptysis. She was admitted and embolization of anomalous artery was planned by the interventional radiologist. During the procedure, the patient developed severe left hypochondrial pain associated with painful breathing. The interventional radiologist advised to start morphine, and embolization was completed. In the ward, the patient was managed conservatively with analgesic paracetamol and morphine. On the next day, the pain became severe and intolerable. On examination, she looked ill and tachypneic, but conscious and fully oriented. Blood pressure was 135/86 mm Hg, temperature 36.5°C, heart rate 106 beats/min, and respiratory rate 20/min. Abdominal examination revealed a tender splenomegaly, without rebound or guarding over the left upper quadrant. The remainder of the examination was unremarkable. An urgent contrast-enhanced abdomen computerized tomography (CT) scan was performed, which showed enlarged spleen with a hypodense wedge-shaped lesion in the superior-posterior part that did not enhance after a contrast injection consistent with splenic infarction (Fig. 2). The infarct was caused by a piece of the coil that was dislodged during the procedure, as reported by our radiologist, who made the diagnosis based on the findings of a very small body with a metallic character that obstructs the splenic artery branch.
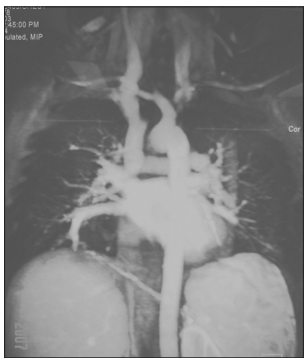
Figure 1: Thoracoabdominal aortography shows a large artery arising from the aorta at the level of D10-11, passing to the right and backward to supply base of the right lung and drained through the venous pulmonary circulation into the right atrium

Figure 2: Contrast-enhanced CT scan showing splenomegaly with sharply demarcated low-density area in the superior-posterior part of the spleen
Initial investigations revealed leukocytes of 11,100/ul (mainly neutrophils); hemoglobin 11 g/dl; and platelets 250,000/ul. Blood sugar, liver function tests, and kidney function tests were within normal limits. Blood samples were sent for culture and sensitivity, and for sickling test, while a bedside transthoracic echocardiography was performed, which showed no vegetation or thrombi. The patient received analgesic, hydration, and empirical intravenous antibiotic therapy. On the 5th day of admission, blood culture and sickling test returned negative and the antibiotic was discontinued. On the following day, the pain subsided and there was no more hemoptysis. Repeat chest radiograph showed coils in the apparent blood vessel (Fig. 3), and the patient was discharged.
DISCUSSION
Splenic infarction is characterized by the sudden onset of pain in the upper left part of the abdomen, sometimes
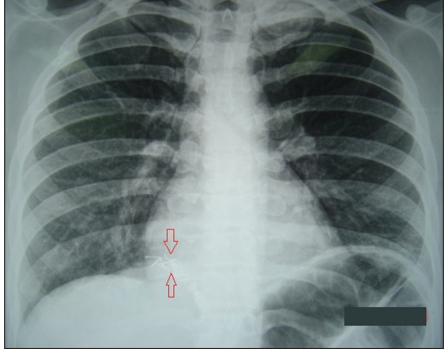
Figure 3: Chest X-ray showing the coil (between red arrows) in apparent blood vessel
associated with splenic tenderness or a painful restriction of breathing [2]. Similarly, our patient developed sudden onset left hypochondrial pain during the embolization procedure with tender splenomegaly and restriction of breathing. Splenic infarction is a rare event that has a variety of causes with sickle cell anemia being the most common [4]. On the other hand, iatrogenic splenic infarction is a very rare clinical entity. Review of the literature revealed few case reports of splenic infarction following various abdominal procedures. One such case described a patient who developed splenic infarction after laparoscopic removal of adrenal carcinoma [2]. While Myung et al. [6] reported a case of cerebral and splenic infarctions after injection of N-butyl-2-cyanoacrylate to treat esophageal variceal bleeding. Our case is unique, as no previous reports showed iatrogenic infarction caused by piece of the coil as described in our report. We made the diagnosis based on the radiological findings and the exclusion of the other causes of splenic infarction such as infection, cardiac embolization, and sickle cell anemia
The spleen receives its blood supply from the splenic artery (which branches from the celiac artery) in combination with the short gastric arteries (which branch from the left gastroepiploic artery). In general, there is considerable anastomotic communication between the stomach arteries and the blood supply systems of the spleen. However, splenic segmental arteries are terminal arteries without any collateral circulation. Therefore, closure of a segmental artery usually leads to infarction of the vascularized splenic segment or splenic pole [7]. In patients with sickle cell disease, the mechanism of splenic infarction is attributed to crystallization of red blood cells and occlusion of the splenic segmental arteries [4]. In our case, a small particle of the coil dislodged and crossed the celiac artery to obstruct one of the splenic segmental artery branches during the anomalous artery embolization. If splenic infarction is suspected as in our case, abdominal CT scan with intravenous contrast is the imaging modality of choice. In the hyperacute phase as in our case, the lesion classically appears as a wedge-shaped area of splenic tissue with the apex pointed toward the helium and the base of the splenic capsule [3,4]. The treatment as in our case is mostly conservative. Analgesia and close follow-up constitute the mainstay of nonoperative treatment. It is important to trace underlying diseases and apply additional management. Surgery is only indicated if there are complications, such as bleeding, pseudocyst formation, and massive abscess [4,8].
CONCLUSION
Iatrogenic splenic infarction after embolization of an anomalous artery supplying a pulmonary sequestration is an extremely rare clinical entity that needs a high index of suspicion. Therefore, clinicians should consider splenic infarction in the differential diagnosis of abdominal pain in patients exposed to embolization of an anomalous artery supplying a pulmonary sequestration. Abdominal CT scan with contrast should be performed as early as possible to establish the diagnosis.
AUTHORS CONTRIBUTION
Kartha A: Data collection, review of the literature, writing final draft. Sulaiman TO: Writing the first draft and reviewing the final draft. All authors read the manuscript and agree to its publication.
References
1. Ozakin E, Cetinkaya O, Kaya FB, et al. A rare cause of acute abdominal pain: Splenic infarct (case series). Turk J Emerg Med 2016;15:96-9.
2. Antopolsky M, Hiller N, Salameh S, et al. Splenic infarction: 10 years of experience. Am J Emerg Med 2009;27:262-5.
3. Cantisani V, Pagliara E, Arduini F, et al. Iatrogenic Splenic Infarction following Laparoscopic Adrenalectomy: Contrast-Enhanced US Findings. Eurorad. Available from: https://www.eurorad.org/case/1942 [Last accessed on 2022 Jun 08].
4. Chapman J, Helm TA, Kahwaji CI. Splenic Infarcts. Treasure Island, FL: StatPearls Publishing; 2021.
5. Weingarten MJ, Fakhry J, McCarthy J, et al. Sonography after splenic embolization: The wedge-shaped acute infarct. AJR Am J Roentgenol 1984;142:957-9.
6. Myung DS, Chung CY, Park HC, et al. Cerebral and splenic infarctions after injection of N-butyl-2-cyanoacrylate in esophageal variceal bleeding. World J Gastroenterol 2013;19:5759-62.
7. Michalik MM, Budziński R, Orłowski M, et al. Splenic infarction as a complication of laparoscopic sleeve gastrectomy. Videosurg Other Miniinvasive Tech 2011;6:92-8.
8. Bokman CL, Sfeir M, Chahwala V, et al. Spontaneous massive splenic infarction in the setting of renal transplant and septic shock: A case report and review of the literature. Case Rep Med 2014;2014:510259.
