Full HTML
Risk factors and outcomes of stroke in a tertiary hospital in Hadhramout Governorate, Yemen
Jamal M Basamed1
Author Affiliation
1Consultant, Department of Medicine, IBN SINA Hospital, Hadhramout, Yemen
Abstract
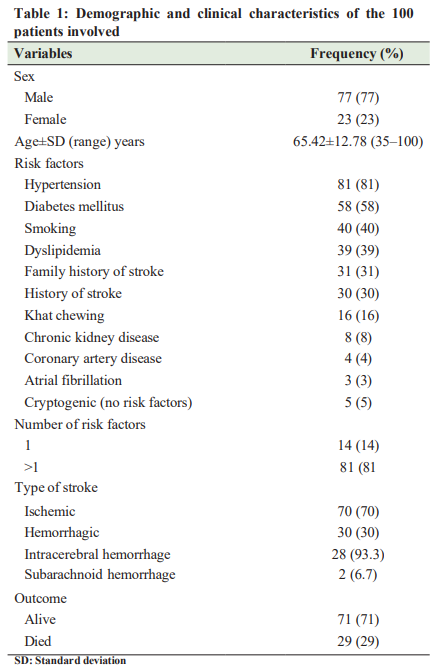
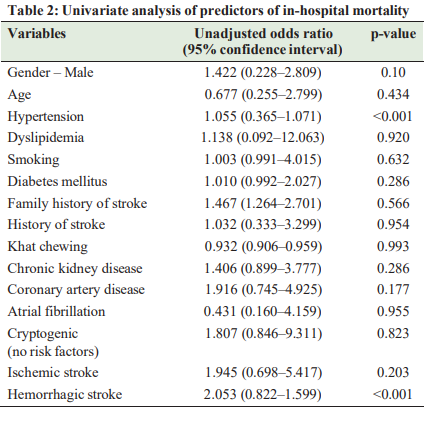
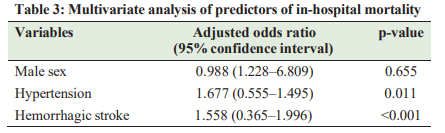
Background: Although stroke is a major problem in Hadhramout Governorate, there is a scarcity of reliable information on risk factors of stroke and predictors of in-hospital mortality. The aim of this study was to explore the risk factors and outcomes of stroke patients admitted to Ibn Sina Hospital, Hadhramout, Yemen, and to identify the predictors of in-hospital mortality. Methods and Materials: This retrospective cross-sectional study was conducted in Ibn Sina Hospital in Mukalla district, Hadhramout Governorate, over a 4-month period (from January 1, 2021, to April 30, 2021). Results: During the study period, we recruited 100 cases of stroke, of whom 77 (77%) were male and 23 (23%) were female. Their mean age was 65.42±12.78 years. Hypertension was the most common risk factor, occurring in 81 (81%) patients, while no risk factors were identified in 5 (5%) cases (Cryptogenic). Ischemic stroke was found in 70 (70%) cases, and hemorrhagic stroke was noticed in 30 (30%) patients. The in-hospital mortality was 29 (29%), and the univariate analysis found male sex, hypertension, and hemorrhagic stroke as probable predictors of in-hospital mortality. Only hemorrhagic stroke (adjusted odds ratio [OR]=2.053 and 95% confidence interval [CI]=0.822–1.599; p<0.001) and hypertension (adjusted OR= 1.677; 95% CI=0.555–1.495; p=0.011) were found to be independent predictors of mortality by multivariate logistic regression analysis. Conclusion: Stroke is a major problem in Hadhramaut Governorate with ischemic stroke being more than hemorrhagic. Men were more likely to have a stroke than women and majority of cases were elderly. Hypertension, diabetes mellitus, smoking, and dyslipidemia were the most commonly identified risk factors that were significantly associated with stroke. Hemorrhagic stroke and presence of hypertension were found to be risk factors for in-hospital mortality; therefore, hypertension should be well-controlled to reduce in-hospital mortality.
DOI: 10.32677/yjm.v1i2.3552
Keywords: Hadhramout Governorate, Hemorrhagic stroke, In-hospital mortality, Ischemic stroke, Risk factors
Pages: 69-73
View: 6
Download: 13
DOI URL: https://doi.org/10.32677/yjm.v1i2.3552
Publish Date: 28-03-2025
Full Text
Stroke is the second leading cause of death worldwide after ischemic heart disease. Each year, there are 15 million strokes and 5.8 million stroke-related deaths, with more than 65% of these deaths occurring in developing countries [1-3]. In addition, stroke is the third most prevalent cause of disability, because it makes victims dependent on society, which affects their personal, social and economic life. Stroke poses a serious threat not only to public health but also to the socioeconomic development of society. The annual cost of treating stroke victims in the United States of America is approximately $34.3 billion [4,5]. The risk factors and lifestyles differ in various countries, requiring investigation of stroke risk factors in each country to identify the pattern of the disease and issue the appropriate educational programs, to reduce the burden of stroke and minimize the high costs of rehabilitation and other unfavorable effects of stroke on the population [6,7]. Stroke is becoming an important cause of premature death and disability in low-income countries like Yemen. The latest figures from the World Health Organization (WHO) show that 13,570 stroke deaths accounting for 8.72% of all deaths occurred in Yemen in 2020. The age-adjusted death rate is 127.49/100,000 population, ranking Yemen 32nd in the world [8]. Part of the reason for this is that the civil war has led to a lack of well-run health-care facilities. In Yemen, there is a scarcity of reliable information on stroke risk factors and outcome predictors, as only a few studies have addressed these issues [9-12]. We conducted this study to explore the risk factors and outcomes of stroke patients admitted to Ibn Sina hospital, Hadhramout, Yemen, and to identify the predictors of in-hospital mortality.
PATIENTS AND METHODS
Study Design, Population, and Setting
A retrospective cross-sectional study was conducted in Ibn Sina Hospital in Mukalla, Hadhramout Governorate, over a 4-month period (January 1, 2021–April 30, 2021). Ibn Sina Hospital is the largest government hospital in Mukalla, in which medical and health institute students get their training and is a tertiary hospital that serves about 4,000,000 people [10]. Mukalla is a seaport and the capital city of Yemen’s largest governorate, Hadhramout. The city lies in the southern part of the Arabian Peninsula on the Gulf of Aden, extending along the shores of the Arabian Sea, about 480 km (300 miles) east of Aden.
Definitions, Inclusion and Exclusion Criteria
Patients were included in the study if they had experienced an acute or a sub-acute stroke confirmed by computed tomography (CT) scans and/or magnetic resonance imaging (MRI) scan. They also had to meet the criteria of the American Heart Association/ American Stroke Association, which define an ischemic stroke as “an episode of neurological dysfunction caused by focal cerebral, spinal, or retinal infarction” and a hemorrhagic stroke as “rapidly developing clinical signs of neurological dysfunction attributable to a focal collection of blood within the brain parenchyma or ventricular system that is not caused by trauma [13]. Patients presented with transient ischemic attack, subdural, or epidural hematoma and symptoms caused by recent trauma were excluded from the study.
We defined the main risk factors as follows. Hypertension was considered positive if the patient is using medication for hypertension or if three consecutive blood pressure estimation readings were above 140/90 mm Hg. Diabetes mellitus was diagnosed if there was a history of diabetes mellitus or if the patient was receiving drugs for diabetes or their random blood sugar levels were above 200 mg (11.1 mmol/L) with symptoms, or if fasting blood sugar scored more than 126 mg (7 mmol/L) or HbA1c >6.5% for more than two readings during hospitalization. Hyperlipidemia was considered positive if lipid profile results show total cholesterol >200 mg/dL and/or triglyceride >150 mg/dL [14]. Heart disease was positive if history, clinical examination, available investigations on admission, or requested investigations during hospitalization yielded one or more of the following: Rheumatic heart disease, ischemic heart disease, atrial fibrillation, and cardiomyopathy. Habits of smoking and khat chewing were positive if patients were using them daily for a duration of at least more than a year.
Data Collection and Source of Data
We obtained the list of the stroke patients from the medical record. We recruited the following variables on a special data collection sheet developed for the sake of the study: Age, gender, risk factors such as hypertension, diabetes mellitus, smoking, dyslipidemia smoking, khat chewing, history of previous attack, and the family history of stroke. Furthermore, we looked for coronary artery disease, and atrial fibrillation. The course of the disease during hospitalization and outcome was recorded as alive on discharge or died during hospitalization (in-hospital mortality)
Ethical Approval and Data Analysis
The study was approved by the administration of Ibn Sina Hospital. Data were reported as means±standard deviation (SD) for quantitative variables, while qualitative variables were described as numbers and percentages. Univariate analysis was performed to determine the probable risk factors for in-hospital mortality. Variables with p<0.10 in the univariate analysis were entered in the multiple logistic regression to identify the independent risk factors for in-hospital mortality at p<0.05. Data analysis was performed with SPSS software (v 23; IBM Corp, Armonk, NY, USA).
RESULTS
During the study period, we recruited 100 consecutive stroke cases, of which 77 (77%) were male and 23 (23%) were female. Their mean age was 65.42±12.78 years (range: 35-100 years). Arterial hypertension was the most common risk factor, occurring in 81 (81%) patients, followed by diabetes mellitus in 58 (58%) patients, smoking in 40 (40%) cases, and dyslipidemia in 39 (39%). Family history was positive for stroke in 31 (31%) patients and history of previous stroke was present in 30 (30%) patients. Risk factors were not identified (Cryptogenic) in 5 (5%) cases (Table 1). COVID-19 preceded stroke in two cases with cryptogenic stroke. Ischemic stroke was identified in 70 (70%) cases, while hemorrhagic stroke was found in 30 (30%) patients. None of the patients were treated with a thrombolytic therapy. The in-hospital mortality was 29 (29%), and all who survived ischemic strokes were prescribed aspirin and statin on discharge. The univariate analysis found the following variables to be probable predictors of in-hospital mortality: Male sex, hypertension, and hemorrhagic stroke (Table 2). Only hemorrhagic stroke (adjusted odds ratio [OR]=2.053; and 95% confidence interval [CI]=0.822–1.599; p<0.001) and hypertension (adjusted OR=1.677; 95% CI=0.555–1.495; p=0.011) were found to be independent predictors of mortality by multivariate logistic regression analysis (Table 3).
DISCUSSION
In Yemen, stroke is a devastating problem, especially after the civil war, which destroyed the fragile pre-existing infrastructures, including the health sector. Only around 51% of the hospitals and health-care facilities are in full working condition [15], while many Yemeni healthcare workers emigrate from the country in search of better salaries and safer conditions elsewhere [16], leaving the population with limited health manpower and little room to respond to stroke or other public health events.
Yemen’s civil war and subsequent humanitarian crises have diverted the attention of the Yemeni authorities away from health
problems such as stroke. The biggest challenge for Yemeni’s health care system, which is to provide care, that is, affordable and accessible to its population is hampered by a lack of humanpower and inadequate resources such as diagnostics, pathology services and stock-outs. Regarding the stroke management in Yemen, the country lacks well-run public health-care facilities such as rehabilitation facilities and stroke units with MRI/CT capabilities. Furthermore, given the state of the economy, the government is unable to provide thrombolysis therapy, which is the gold standard of care for acute ischemic stroke. As a result, most people rely on the private sector for health care, which provides almost 80% of health services. However, the private health sectors are providing some of the facilities such as CT scan and MRI at high prices which are out of reach for most people. The true stroke incidence and prevalence in Yemen is yet unknown, due to lack of stroke data banks and stroke registries. Moreover, with the highly privatized nature of health-care service, most patients are unable to access private health facilities due to financial constraints. Therefore, many people, especially the elderly, are left at home without being diagnosed or counted. In the present study, the mean age of stroke patients was 65.42 years, which is consistent with a study by Dey et al. [17], who reported a mean age of 68.41 years, and Al-Shenqiti [7], who reported a mean age of 67.52 years, but higher than that mentioned by Nour et al., who reported a mean age of 59.61 years [18]. Increased burden of stroke among aged population can be attributed to an increase in risk factors such as cardiovascular disease, hypertension, diabetes mellitus, and ischemic heart disease [17]. As noted, about 77% of the patients involved in this study were male, which is consistent with studies from Saudi Arabia [7], India [17,19], Ethiopia [20], and Kenya [21]. The global trend toward male dominance is not fully understood but could be partly explained by the fact that hypertension, diabetes mellitus, smoking, and alcoholism are more common among male patients. The results of this study are consistent with the previous local studies [9-12], which showed that ischemic stroke was the most frequent form, followed by hemorrhagic stroke. This is consistent with studies from Saudi Arabia [7], India [17,19], Ethiopia [20], and Kenya [21], but unlike a study conducted at St. Paul Hospital, which found that hemorrhagic strokes made up 61.3% of cases, making them more frequent than ischemic strokes [22]. As noted in this study, hypertension, which accounts for 81% of cases, was the major risk factor associated with stroke. This finding is consistent with earlier studies conducted in hospital settings in our country [9-12] and other Arab and African countries [7,18,20-25]. The degree of mental stress brought on by poverty and instability, particularly after the civil war, is probably closely correlated with the frequency of hypertension. The fact that many of our patients had poor blood pressure management caused by non-adherence to treatment due to cost and drug availability certainly increased the significance of hypertension control. As noted in this study, diabetes mellitus ranked second on the list of risk factors as did other hospital studies around the world [7,17-26]. The present study showed that smoking was a significant risk factor, occurring in 40% of all stroke cases, which is high compared to previous local studies conducted earlier in the same hospital [11,12], which reported smoking in 21% and 26% of cases, respectively. The difference in figures between two periods reflects the changes in the lifestyle of the population in this governorate. Dyslipidemia was found in 39% of the cases, which is high as compared with previous local studies [9-12], but consistent with a study by Qawasmeh et al. [24] who reported a frequency of 37% and lower than that reported by Khan et al., who observed a frequency of 52.5% [23]. In the present study, khat chewing was reported in 16% of cases, which is lower than in a prior study [9]. Chewing khat is a common habit in Yemen. It is estimated that up to 90% of adult men and 73% of adult women chew khat for 3–4 h daily in this country. In addition, 15–20% of children under the age of 12 are also daily consumers [27]. Khat is a stimulant made from the leaves of the plant Catha edulis. Some reports from Yemen [28,29] observed a correlation between khat chewing habit and cardiovascular diseases. Although these studies have significant limitations, they highlight the necessity for additional large-scale trustworthy studies to confirm the relevance of khat chewing as a risk factor for cardiovascular disease, including stroke. As previously mentioned, 5% of the cases in this study had no risk factors. Interestingly, two of these instances had ischemic stroke preceded by prior COVID-19, implying that COVID-19 may play a role in stroke pathogenesis. A review of the literature revealed conflicting results, while Qureshi et al. [30] concluded that acute ischemic stroke was uncommon in patients with COVID-19 and typically occurs in the presence of other cardiovascular risk factors, other reports found that the risk of stroke and heart attack increases sharply in the weeks following a COVID-19 diagnosis [31-33], suggesting an interplay of vascular risk factors and immune responses to the SARS-CoV-2 virus as a mechanism. A recent meta-analysis [34] concluded that when a patient is admitted with COVID-19, the risk of ischemic stroke must be considered. In general, the design of the present study was descriptive making it impossible to draw meaningful inferences about the relationship of these factors with stroke. In-hospital mortality ranges between 2.8% and 46% [9,17,18]. In-hospital mortality in the present study was 29%, which falls within the global range. Many risk factors for in-hospital mortality were identified. Russell et al. [35] found the following variables as independent risk factors for in-hospital mortality: hypertension, previous stroke, Glasgow coma scale 75 years as independent predictors of in-hospital mortality. Hemorrhagic stroke and hypertension were revealed to be independent predictors of in-hospital mortality after stroke in the current study. This study has several limitations. First, it is a retrospective hospital-based study, where patient follow-up was not feasible as we mainly depend on the patient’s medical records. Second, the sample size was small, although the original study was designed to include all stroke cases in 2021. However, in the retrospective review of medical records, only 100 medical records were consecutive and contained enough information to be included in the study. Third, denial of alcohol consumption can be incorrect, because it is a social and religious taboo. Finally, cardioembolic work-ups were incomplete. Future studies could include a more complete and rigorous evaluation of possible cardiovascular etiologies by having cardiologists as a part of the investigation team. CONCLUSION Stroke is a major problem in Hadhramout Governorate with ischemic stroke being more than hemorrhagic. Men were more likely to have a stroke than women and majority of cases were elderly. Hypertension, diabetes mellitus, smoking, and dyslipidemia were the most commonly identified risk factors that were significantly associated with stroke. Hemorrhagic stroke and presence of hypertension were found as risk factors for in-hospital mortality; therefore, hypertension should be wellcontrolled to reduce in-hospital mortality. The identification of additional risk factors for stroke is crucial to the improvement of population health.
References
1. Feigin VL. Stroke epidemiology in the developing world. Lancet 200;365:2160-1.
2. Eltemamy MA, Tamayo A, Altarsha E, et al. Cerebrovascular risk profiles in a Saudi Arabian cohort of young stroke patients. Front Neurol 2021;12:736818.
3. El-Hajj M, Salameh P, Rachidi S, et al. The epidemiology of stroke in the Middle East. Eur Stroke J 2016;1:180-98.
4. Roger V, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics 2012 update: A report from the American heart association. Circulation 2012;125:e2-e220.
5. Howard VJ, Cushman M, Pulley L, et al. The reasons for geographic and racial differences in stroke study: Objectives and design. Neuroepidemiology 2005;25:135-43.
6. Boehme AK, Esenwa C, Elkind MS. Stroke risk factors, genetics, and prevention. Circ Res 2017;120:472-95.
7. Al-Shenqiti AM. Types and risk factors of first-time stroke: A Saudi hospitalbased study. Int J Physiother 2019;6:118-22.
8. World Health Rankings. Available from: https://www.worldlifeexpectancy. com/yemen-stroke#:~:text=Yemen%3A%20Stroke&text=According%20 to%20the%20latest%20WHO,Yemen%20%2332%20in%20the%20world [Last accessed on 2022 Jun 15].
9. Sallam A, Al-Aghbari K, Awn H. The clinical profile of stroke: A Yemeni experience. Jordan Med J 2009;43:115-21.
10. Bamekhlah RM, Bin-Nabhan AS, Musaian NS. Risk factors and clinical presentation of stroke in Mukalla, Hadhramout, republic of Yemen. Alandalus J Appl Sci 2014;391:40-57.
11. Bamekhlah RM, Bamekhlah MR, Al-Ghazali HS, et al. Comparative study between haemorrhagic and ischaemic strokes in Hadramout: A hospital-based study. Hamdan Med J 2019;12:29-33.
12. Salah MQ, Aljarmouzi HM, Al-Makdad AM. Prevalence and pattern of stroke among patients attending a teaching hospital in Dhamar governorate, Yemen. Ann Med Health 2019;1:1-4.
13. Sacco RL, Kasner SE, Broderick JP, et al. An updated definition of stroke for the 21st century: A statement for healthcare professionals from the American heart association/American stroke association. Stroke 2013;44:2064-89.
14. Expert Panel on Detection, Evaluation, and Treatment of High blood Cholesterol in Adults. Executive summary of the third report of the national cholesterol education program (NCEP) Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA 2001;285:2486-97.
15. Lutf AQ. COVID-19 in Yemen: The present situation and the future plan to overcome the crisis. Yemen J Med 2022;1:14-6.
16. Hezam HS. Knowledge, attitudes, and practices toward COVID-19 among healthcare workers in Shabwah Governorate, Yemen: A cross-sectional study. Yemen J Med 2022;1:31-5.
17. Dey G, Jyothi R, Pradeep C, et al. A prospective observational study on prescribing pattern and outcome of acute stroke from a tertiary care hospital in Bengaluru, India. J Clin Diagn Res 2022;16:FC01-5.
18. Nour MA, Mrabet S, Maidal MA, et al. Stroke in Djibouti. Afr J Emerg Med 2022;12:141-7.
19. Patne SV, Chintale KN. Study of clinical profile of stroke patients in rural tertiary health care centre. Int J Adv Med 2016;3:666-70.
20. Mulugeta H, Yehuala A, Haile D, et al. Magnitude, risk factors and outcomes of stroke at debre markos referral Hospital, Northwest Ethiopia: A retrospective observational study. Egypt J Neurol Psychiatry Neurosurg 2020;56:41.
21. Jowi J, Mativo P. Pathological sub-types, risk factors and outcome of stroke at the Nairobi hospital, Kenya. East Afr Med J 2008;85:572-81.
22. Temesgen TG, Teshome B, Njogu P. Treatment outcomes and associated factors among hospitalized stroke patients at Shashemene referral hospital, Ethiopia. Stroke Res Treat 2018,2018:8079578.
23. Khan FY, Yasin M, Abu-Khattab M, et al. Stroke in Qatar: A first prospective hospital-based study of acute stroke. J Stroke Cerebrovasc Dis 2008;17:69-78.
24. Qawasmeh MA, Aldabbour B, Momani A, et al. Epidemiology, risk factors and predictors of disability in a cohort of Jordanian patients with the first ischemic stroke. Stroke Res Treat 2020;2020:1920583.
25. Lahoud N, Abbas MH, Salameh P, et al. A retrospective analysis of 254 acute stroke cases admitted to two university hospitals in Beirut: Classification and associated factors. Funct Neurol 2017;32:41-8.
26. Al Harthi HA, Al Kashmiri A, Zakaryia LM, et al. Clinical profile of stroke patients presenting to the emergency department of a major stroke centre in Oman. Sultan Qaboos Univ Med J 2022;22:91-7.
27. Al-Mugahed L. Khat chewing in Yemen: Turning over a new leaf. Bull World Health Organ 2008;86:741-2.
28. Ali WM, Zubaid M, Al-Motarreb A, et al. Association of Khat chewing with increased risk of stroke and death in patients presenting with acute coronary syndrome. Mayo Clin Proc 2010;85:974-80.
29. Al-Motarreb A, Briancon S, Al-Jaber N, et al. Khat chewing is a risk factor for acute myocardial infarction: A casecontrol study. Br J Clin Pharmacol 2005;59:574-81.
30. Qureshi AI, Baskett WI, Huang W, et al. Acute ischemic stroke and COVID-19: An analysis of 27 676 patients. Stroke 2021;52:905-12.
31. Tu TM, Seet CY, Koh JS, et al. Acute ischemic stroke during the convalescentphase of asymptomatic COVID-2019 infection in men. JAMA Netw Open 2021;4:e217498.
32. Siepmann T, Sedghi A, Simon E, et al. Increased risk of acute stroke among patients with severe COVID-19: A multicenter study and meta-analysis. Eur J Neurol 2021;28:238-47.
33. Neurology and Neurosurgery: https://www.mayoclinic.org/medicalprofessionals/neurology-neurosurgery/news/proposed-pathogenesisfor-stroke-in-patients-with-covid-19/mac-20529959 [Last accessed on 2022 Jun 29].
34. Luo W, Liu X, Bao K, et al. Ischemic stroke associated with COVID-19: A systematic review and meta-analysis. J Neurol 2022;269:1731-40.
35. Russell JB, Charles E, Conteh V, et al. Risk factors, clinical outcomes and predictors of stroke mortality in Sierra Leoneans: A retrospective hospital cohort study. Ann Med Surg (Lond) 2020;60:293-300.
36. Kamabu LK, Lekuya HM, Kasusula BM, et al. Risk factors of mortality among patients with stroke in eastern region of the democratic republic of Congo: A retrospective series study. PAMJ Clin Med 2021;4:123.
