Full HTML
Analysis of perinatal mortality in Aden General Hospital: A hospital-based study from Yemen
Nada Yusuf Khan1 , Sami Bawazeer2,3
Author Affiliation
1Consultant, Department of Obstetrics and Gynecology, Aden General Hospital, Aden, Yemen,
2 Senior Consultant, Department of Obstetrics and Gynecology, AlSadaka Teaching Hospital, Aden, Yemen,
3Professor, Department of Obstetrics and Gynecology, Faculty of Medicine, Aden University, Aden, Yemen
Abstract
Background: Perinatal mortality remains high in developing countries, including Yemen. However, information on perinatal mortality in Yemen is lacking. This study aimed to find out the perinatal mortality rate in Aden General Hospital and to analyze the causes of perinatal mortality.
Materials and Methods: This descriptive study was conducted at the Obstetrics and Gynecology Department of Aden General Hospital during the period from January 1, 2003 to June 30, 2004. It was a retrospective study for the first 6 months (January–June 2003) and prospective for the remaining period (July 2003–June 2004).
Results: During the study period from January 1, 2003 to June 30, 2004, there were a total of 3770 births at Aden General Hospital, out of which there were 2976 births during the period from January to December 2003 and a further 794 births in the 6-month period from January to June 2004. The perinatal deaths were 166 (4.4%) giving a perinatal mortality rate of 44/1000 normal deliveries. Further analysis showed a total of 105 perinatal deaths in 2003 with a perinatal mortality rate of 35.3/1000 normal deliveries and 61 deaths in the period from January to June 2004 with a rate of 77/1000 normal deliveries. Unclassified deaths including premature cases accounted for 29% (n=48) of all causes, followed by mechanical causes 36 (21.7%). The mechanical causes are divided as follows, 33 (19. 9%) due to fetal distress and 3 (1.8%) due to breech presentation. Uncertain origin causes accounted for 19.3% (n=32) of all cases of death and toxemia was observed in 16 cases (9.6%), while malformation was found in 13 (7.8%) cases.
Conclusion: The perinatal mortality rate in our center was 44/1000 deliveries. The major cause of perinatal mortality was prematurity, followed by mechanical causes. The most of the mortalities occurred outside the health facilities (extra-hospital).
DOI: 10.32677/yjm.v1i1.3327
Keywords: Extra-hospital delivery, Perinatal mortality rate, Perinatal mortality, Premature delivery
Pages: 22-26
View: 3
Download: 8
DOI URL: https://doi.org/10.32677/yjm.v1i1.3327
Publish Date: 27-03-2025
Full Text
Perinatal mortality remains a serious global public health problem with high burden and intrapartum complications being major contributors, especially in low-income countries [1-3]. Perinatal death is associated with many preventable factors which can be avoided by providing highquality care and timely interventions, especially during labor and delivery. These factors include poor maternal health care, inadequate care during pregnancy and childbirth, inappropriate management of complications, poor hygiene during the 1st critical h after birth, and poor newborn care [2,3]. The concept of a perinatal period emerged in the late 1940s as clinicians and researchers became increasingly aware of the relatively large number of deaths occurring in the period immediately before and after delivery [4]. Perinatal mortality is an important indicator of the quality of antenatal, intrapartum, and newborn care in any health-care system. Globally, the true burden of perinatal death is unclear, particularly in developing countries, due to the lack of reliably reported quality of data on the causes of perinatal death. The most of the global data comes from the developed countries. Yemen is no exception as the true perinatal mortality figures are not available for the whole country. In the North of the country, the average perinatal mortality rate was 24/1000 live births in 1983–1984 [5]. An important first step in the analysis of perinatal death is to identify the case circumstances, including relevant details regarding maternal history, obstetric history, and current pregnancy (complications are evaluated and recorded). In the next step, the placental examination is suggested in all cases, together with molecular cytogenetic evaluation and fetal autopsy [6]. In Yemen and before the war between the Saudi-led coalition government and the Houthi rebels escalated in early 2015, the health system was inadequate, lacking medical staff and supplies. Efforts to estimate the perinatal mortality rate in parts or across the country have been hampered by a lack of facilities as well as traditions that discourage autopsy. This study aimed to find out the perinatal mortality rate in Aden General Hospital and to analyze the causes of perinatal mortality.
MATERIALS AND METHODS
Study Design, Population, and Setting
This descriptive study was conducted at the Obstetrics and Gynecology Department of Aden General Hospital during the period from January 1, 2003 to June 30, 2004. It was a retrospective study for the first 6 months (January–June 2003) and prospective in the remaining period (July 2003–June 2004). Aden General Hospital was a referral hospital located at Aden governorate in the South and it used to receive cases from different governorates of the Southern parts of Yemen. It is one of the governorate’s largest public hospitals with 200 beds capacity. It includes all specialties including pediatrics, obstetrics, and gynecology. Unfortunately, the hospital has been closed in 2005 for renovation before the last war. Since then, the hospital remained closed.
Data Source, Data Collection, and Ethical Clearance
For the first 6 months, data were collected from the case sheets from our hospital archives alongside the monthly reports of the Perinatal Mortality Committee, while for the remainder of the study period, data were collected through a face-to-face interview with the mothers and by completing the questionnaire, which previously prepared by the author for the purposes of this study. The primary outcome of this study was assessment of perinatal mortality. Permission for this study was obtained from the hospital management.
Definitions of the Main Variables and Terminology Used in this Study
We applied the World Health Organization (WHO) definitions of perinatal mortality, perinatal mortality rate, fetal death, early neonatal, and late fetal deaths [7-9]. Perinatal mortality (weightspecific) is defined as the number of fetal stillbirths and 1st-week death of babies weighing 1000 g or more at birth. The perinatal mortality rate in our study was computed as the sum of the number of perinatal deaths (still births and early neonatal deaths) divided by the number of total births (all live births plus still births) multiplied by 1000. Fetal death is defined as death before the complete expulsion or extraction from the mother of a product of conception and irrespective of the duration of pregnancy; the death is indicated by the fact that after such separation, the fetus does not breath or show any other evidence of life such as the beating of the heart, pulsation of the umbilical cord, or any definite movement of voluntary muscles. Live birth is defined as the complete expulsion or extraction from its mother of a product of conception, irrespective of the duration of the pregnancy, which after such separation, breathes or shows any other evidence of life, such as the beating of the heart, pulsation of the umbilical cord, or definite movement of voluntary muscles, whether or not the umbilical cord has been cut or the placenta is detached. Late fetal death is the fetal death at 28 completed weeks of gestation and over. Early neonatal death is the death of a live-born baby in the first 7 completed days (168 h) of life and for the purpose of this work with a birth weight of 1000 g or more. Normal birth weight (NBW) is defined as the weight of newborn infants at the birth of 2500 g or more. Low birth weight (LBW) is defined as the weight of a newborn at birth when it is <2500 g. (Up to and including 2499 g). It is classified into two groups: LBW ≥1500 and <2500 g and very LBW <1500 g (1000–1499 g). Regarding the mother, her age was expressed in years according to her birthday. If the mother does not know her age, we tried to obtain the estimated age by asking her some relevant questions such as her age at marriage, the age of her first baby, and her age at first delivery. We also applied the WHO definitions of parity and quality of antenatal care [10-12]. Antepartum late fetal death is defined as the fetal death in which the heartbeat ceased before labor. Intrapartum late fetal death is defined as the fetal death in which the heartbeat ceased during labor. Extrahospital and intra-hospital fetal death is defined as the fetal death when the cessation of heartbeat occurred outside or inside the hospital, respectively [7,10-12]. We used Aberdeen classification to describe the causes of perinatal mortality [12].
Statistical Analysis
The gathered information was transferred to the computer utilizing SPSS software (v 11.0; IBM Corp, Armonk, NY, USA). A simple descriptive analysis using frequency tabulation was conducted.
RESULTS
During the period of our study from January 1, 2003 to June 30, 2004, there were 3770 births at Aden General Hospital, divided into 2976 in 2003 and 794 in the period from January to June 2004. The perinatal deaths were 166 (4.4%) giving a perinatal mortality rate of 44/1000 normal deliveries divided into 105 in 2003 with a perinatal mortality rate of 35.3/1000 normal deliveries and 61 from the period January to June 2004 with a rate of 77/1000 normal deliveries.
The Perinatal Mortality Rate in Relation to Weight, Time, and Place of Death
Early neonatal deaths accounted for 57.2% (n=95) of all deaths and the rate was 26.4/1000 live births, while late fetal deaths accounted for 42.8% (n=71) of all deaths and the rate was 18.8/1000 live births. The antepartum fetal deaths were 61 (85.9%) with a rate of 16.1/1000 deliveries of which 34 cases were reported in 2003 with a rate of 11.4/1000 deliveries and 27 cases in the period from January to June 2004 with a rate of 34/1000 deliveries. Intrapartum cases were 10 (14.1%) and the rate was 2.7/1000 deliveries. The intra-hospital late fetal death was 7 in 2003 with a rate of 2.4/1000 deliveries, while in the period between January and June 2004, there were five deaths and the rate was 6.3/1000 deliveries, giving a total of 12 cases and a rate of 3.2/1000 deliveries. Table 1 summarizes the perinatal mortality rate in relation to weight, time of death (Antepartum vs. intrapartum), and place of death (intra-hospital vs. extra-hospital) in Aden General Hospital during the study period.
Causes of Perinatal Mortality According to the Aberdeen Classification
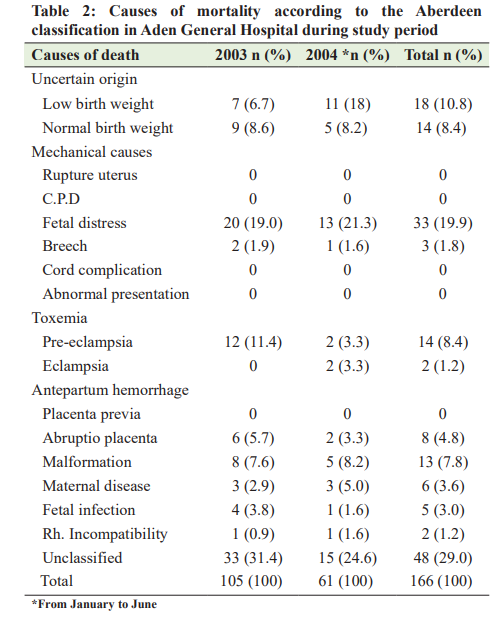
Unclassified deaths including premature cases accounted for 29% (n=48) of all causes, followed by mechanical causes 36 (21.7). The mechanical causes are divided as follows, 33 (19.9%) due to fetal distress and 3 (1.8%) due to breech presentation. Uncertain origin causes accounted for 19.3% (n=32) of all cases of death, and toxemia was observed in 16 cases (9.6%), and malformation was found in 13 (7.8%) cases. Table 2 describes the causes of perinatal mortality according to the Aberdeen classification.
Perinatal Mortality in Relation to Body Weight at Birth
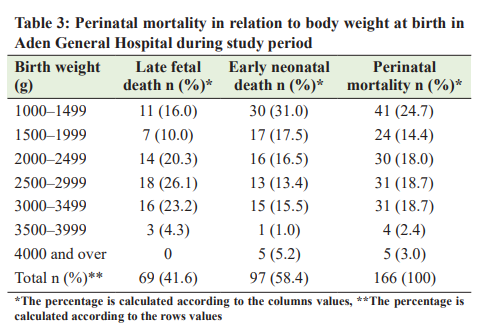
The majority of deaths occurred in the birth weight group between 1000 and 1499 g, accounting for 24.7% (n=41) of all deaths. There is a decrease in the percentage of deaths with increasing birth weight group reaching 4 (2.4%) in birth weight 3500–3999 g and 5 (3.0%) in birth weight 4000 and more. Table 3 summarizes the perinatal mortality in relation to body weight at birth.
Perinatal Mortality in Relation to Maternal Age, and Parity Groups, and the Antenatal Care Received by Mothers
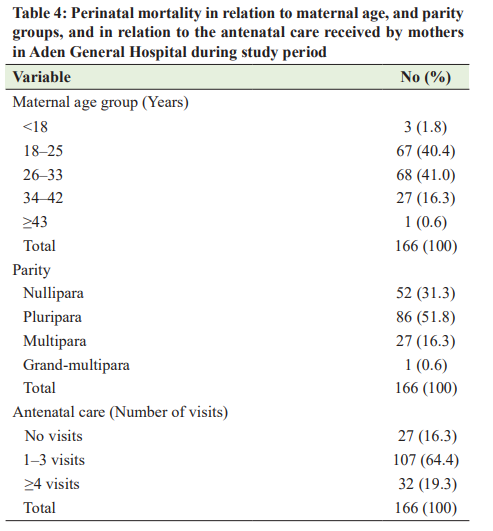
Most cases occurred in mothers in the 26–33 age group accounting for 41% (n=68) of all cases, followed by the 18–25 age group with the death of 67 (40.4%), then 34–42 years old, 27 (16.3%), and then <18 years old with 3 deaths (1.8%), whereas in the age group 43 years and over, there is no that there was only 1 death (0.6%). Perinatal mortality in relation to mother parity showed that the majority of deaths occur among pluripara, 86 (51.8%), followed by nullipara 52 (31.3%), then in multipara 27 (16.3%), and finally grand-multipara 1 (0.6%). The most of the mothers with perinatal deaths had 1–3 visits to the antenatal care centers [107 (64.4%)] and about 32 (19.3%) had four or more visits and 27 (16.3%) did not receive antenatal care at all. Table 4 explores the perinatal mortality in relation to maternal age, parity groups, and the antenatal care received by mothers.
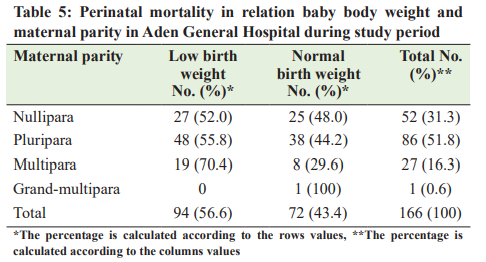
Perinatal Mortality in Relation to Baby Bodyweight and Maternal Parity
The distribution of perinatal deaths by birth weight (LBW <2500 g vs. normal weight 2500 g and more) is shown in Table 5. It showed that the LBW group has higher mortalities compared with NBW [94(56.6%) vs. 72(43.4%)].
DISCUSSION
This study was conducted in 2004, as a prerequisite for the final examination of the Arab board certificate in obstetrics and gynecology, but it has not been published since then. Having revised the definitions and discussion with the references updated, I still believe that this is a novel work that will add to the current efforts to estimate the burden of perinatal mortality in Yemen and worldwide. To the best of our knowledge, this is the first work describing perinatal mortality in Aden General Hospital, Yemen. To overcome the obstacles of lack of facilities and the tradition that discourages autopsies, we used the clinic-epidemiological classification of Aberdeen for the evaluation and classification of the causes of perinatal mortality. Reports from developing and rich countries have shown improvements in perinatal and neonatal outcomes with increased coverage by health services and skilled birth attendants [13- 16]. In our study, the perinatal mortality rate was 44/1000 deliveries (Table 1), which is higher than other countries such
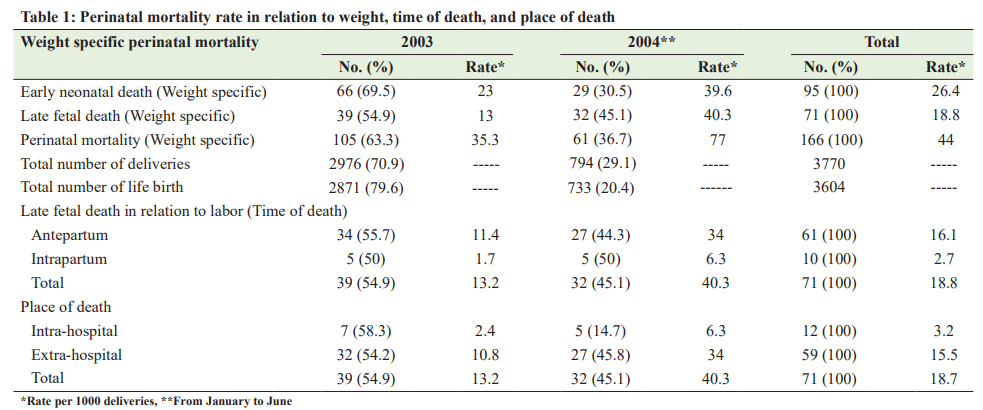
as the UK, Australia, USA, Saudi Arabia, and Iraq, but lower than that recorded in Sudan, Turkey, Pakistan, Brazil, and India [8,9,12,17-19]. Our study also showed in Table 1, that extrahospital late fetal deaths were 5 times more than the intra-hospital late fetal deaths, indicating that most of the deliveries occurred at home and not in the public health facilities. These figures were obtained before the civil war started, when Aden General Hospital was still operational and working. At present, and after 7 years of the war, only 51% of all health facilities in the country are fully functional, and there were only one large public hospital and one small center providing maternity services in the governorate of Aden, with only a few private hospitals, leaving pregnant women and newborns with limited access to a wider range of maternal
and child health services. In its 2019 report, the United Nations International Children’s Emergency Fund had found that only three out of 10 births taking place in regular health facilities, resulting in one woman and six newborns dying every 2 h due to complications during pregnancy or childbirth [20]. Ascertaining the cause of perinatal death helps in determining the avoidable and preventable factors in a given society and facilitates the work of health authorities to come up with the appropriate solutions to minimize the perinatal mortality rate. In the present study, we found that the main causes of perinatal mortality were prematurity 48 (29%), mechanical 36 (21.7%), and uncertain 32 (19.3%). Similarly, prematurity has been reported as the leading cause of perinatal mortality in many countries including Sudan, Pakistan, Brazil, Iran, Turkey, and Nepal [8,12,17,21-23]. This finding highlights the importance of offering antenatal care and skilled health attendance to ensure the safety of both mothers and babies. In addition, providing adequate neonatal intensive care units with surfactant therapy and ventilator support would further lessen the number of cases of preterm perinatal mortalities.
Moreover, this study demonstrated that mechanical causes (Breech and fetal distress) ranked second in the list of causes of perinatal mortality, which was also a major finding by some authors from Sudan, Pakistan, India, and Iran [8,12,19,21]. All mechanical causes can be avoided and perinatal deaths reduced with good obstetric care and appropriate prenatal planning for delivery as well as appropriate intrapartum monitoring. Interestingly, perinatal deaths of uncertain causes ranked 3rd in our list accounting for 19.3% of all death cases. In many reports from Pakistan, Saudi Arabia, Brazil, India, Iran, Turkey, and Nepal [12,16-19,21-25], approximately one-third of fetal deaths remain unexplained. The most important step in identifying the causes of perinatal mortality includes placental examination, together with molecular cytogenetic evaluation and fetal autopsy, which requires adequate health facilities and positive attitude toward fetal autopsy. In Yemen, since, the fetal autopsy is not performed routinely for perinatal deaths, the cause of death in a significant number of cases will remain unexplained. This study has several limitations that need to be considered when interpreting these data. First, this study was hospital-based and it did not reflect the community situation. Second, it is based on clinic-epidemiological classification, which is attributed to the inability to perform fetal biopsy in this country. Third, the data were old reflecting the period before the civil war. However, due to the paucity of studies in this field, this study can be used as a reference for any future work.
CONCLUSION
The perinatal mortality rate of our center was 44/1000 deliveries. The major cause of perinatal mortality was prematurity, followed by mechanical causes, and the most of the cases occurred outside the health facilities (extra-hospital). Improving prenatal care, promoting hospital accessibility, promoting hospital equipment, timely referral from referring centers, and good neonatal care are recommended for better outcomes. Autopsy of the dead baby in unexplained or uncertain perinatal deaths would help determine the cause to enable future interventions.
AUTHORS’ CONTRIBUTION
Khan NY collected and analyzed the data, reviewed the literature, and wrote the final manuscript. Bawazeer S proposed the idea, reviewed the literature, aided in the data analysis, and the revision of the final manuscript. All authors read the manuscript and agree to its publication.
References
1. Liu L, Oza S, Hogan D, et al. Global, regional, and national causes of child mortality in 2000-13, with projections to inform post-2015 priorities: An updated systematic analysis. Lancet (London, England) 2015;385:430-40.
2. Vogel JP, Souza JP, Mori R, et al. Maternal complications and perinatal mortality: Findings of the World Health Organization Multicountry Survey on Maternal and Newborn Health. BJOG 2014;121 Suppl 1:76-88
3. de Bernis L, Kinney MV, Stones W, et al. Stillbirths: Ending preventable deaths by 2030. Lancet (London, England) 2016;387:703-16.
4. Peller S. Mortality, past and future. Popul Stud 1948;1:405-56.
5. UNICEF. The Situation of Children and Women in Republic of Yemen. Sana’a: UNICEF; 1992. p. 75-86.
6. Nijkamp JW, Sebire NJ, Bouman K, Korteweg FJ, Erwich JJ, Gordijn SJ. Perinatal death investigations: What is current practice? Semin Fetal Neonatal Med 2017;22:167-75.
7. Neonatal and Perinatal Mortality, Country, Regional and Global Estimates. Available from: https://apps.who.int/iris/bitstream/ handle/10665/43444/9241563206_eng.pdf?sequence=1&isAllowed=y. [Last accessed on 2022 Jan 01].
8. Dafallah SE, Elhadi H. Perinatal mortality rate in a teaching hospital in Sudan. Review of 15 years. Saudi Med J 2004;25:242-3.
9. Erdem G. Perinatal mortality in Turkey. Paediatr Perinat Epidemiol 2003;17:17-21.
10. Berg CJ. Prenatal care in developing counties: The World Health Organization technical working group on antenatal care. J Am Med Womens Assoc 1995;50:182-6.
11. Zanconato G, Msolomba R, Guarenti L, et al. Antenatal care in developing countries: The need for a tailored model. Semin Fetal Neonatal Med 2006;11:15-20.
12. Korejo R, Bhutta S, Noorani KJ, et al. An audit and trends of perinatal mortality at the Jinnah Postgraduate Medical Centre, Karachi. J Pak Med Assoc 2007;57:168-71.
13. MacDorman MF, Munson ML, Kirmeyer S. Fetal and perinatal mortality, United States, 2004. Natl Vital Stat Rep 2007;56:1-19.
14. Macintosh MC, Fleming KM, Bailey JA, et al. Perinatal mortality and congenital anomalies in babies of women with Type 1 or Type 2 diabetes in England, Wales, and Northern Ireland: Population based study. BMJ 2006;333:177.
15. Queensland Mothers and Babies 2014 and 2015. Available from: https:// clinicalexcellence.qld.gov.au/sites/default/files/docs/qmpqc-report-2017. pdf [Last accessed on 2022 Jan 01].
16. Sobaih BH, Al-Shebly MM. Perinatal statistics of a 15-year period in the Central Region of Saudi Arabia. Sudan J Paediatr 2013;13:23-30.
17. Al-Ani ZR, Al-Hiali SJ, Al-Mashhadani WS. Perinatal mortality rate in Al-Ramadi maternity and children’s hospital, Western Iraq. Saudi Med J 2009;30:1296-300.
18. Bezerra IM, Ramos JL, Pianissola MC, et al. Perinatal mortality analysis in Espírito Santo, Brazil, 2008 to 2017. Int J Environ Res Public Health 2021;18:11671.
19. Mavalankar DV, Trivedi CR, Gray RH. Levels and risk factors for perinatal mortality in Ahmedabad, India. Bull World Health Organ 1991;69:435-42.
20. Yemen: Maternal and Newborn Health “on the Brink of Total Collapse”. UNICEF Alerts. Available from: https://news.un.org/en/ story/2019/06/1040531 [Last accessed on 2022 Jan 01].
21. Hadavi MA, Alidalaki S, Aminzadeh F. Effective factors on perinatal mortality in Rafsanjan Hospitals (2004-2006). J Rafsanjan Univ Med 2009;8:117-26.
22. Ecevit A, Oguz SS, Tarcan A, et al. The changing pattern of perinatal mortality and causes of death in central Anatolian region of Turkey. J Matern Fetal Neonatal Med 2012;25:1738-41.
23. Dali SM, Tuladhar TH, Pradhan P, et al. Perinatal death audit. J Nepal Med Assoc 2003;42:383-6.
24. Bellad MB, Srividhya K, Kangle R, et al. Factors associated with perinatal mortality: A descriptive observational study. J South Asian Federation Obstet Gynecol 2010;2:49-51.
25. Shrestha S, Sharma A, Upadhyay S, et al. Perinatal mortality audit. Nepal Med Coll J 2010;12:257-9.
