Full HTML
Assessing the Relationship Between the Dietary Pattern, Oral Hygiene and Self-Reported Gingival Bleeding in Pregnant Women in Ondo, Southwest Nigeria
Ikponmwosa Augustine Edomwonyi1, Jacob Babatunde Afolabi2, Ayobami Temitayo Abayomi3, Olayinka Timothy Edun4, Precious Oreoluwa Akingbule5
Author Affiliation
1 Consultant, Department of Preventive Dentistry, University of Medical Sciences Teaching Hospital, Ondo, Ondo state, Nigeria
2 Consultant, Department of Child Dental Health, University of Medical Sciences Teaching Hospital, Ondo, Ondo state, Nigeria
3 Dentist, University of Medical Sciences Teaching Hospital, Ondo, Ondo State, Nigeria
4 Dentist, University of Medical Sciences Teaching Hospital, Ondo, Ondo State, Nigeria
5. Dentist, University of Medical Sciences Teaching Hospital, Ondo, Ondo State, Nigeria
Abstract
Background: Pregnancy-related hormonal changes increase the risk of gingival inflammation and bleeding. Poor oral hygiene and dietary habits, such as frequent intake of sugary foods, may worsen this risk. Understanding the relationship between diet, oral hygiene, and gingival health in pregnant women is essential for improving prenatal care. This study aimed to assess dietary patterns, oral hygiene practices, and self-reported gingival bleeding among pregnant women attending the Mother and Child Hospital, Ondo, Nigeria.
Methods: A descriptive cross-sectional study was conducted over four months among 216 pregnant women at the Mother & Child Clinic, University of Medical Sciences Teaching Hospital, Ondo, Southwest Nigeria. A structured, self-administered questionnaire collected data on sociodemographic characteristics, oral hygiene habits, perceived oral health conditions, and dietary patterns. Clinical oral examinations were conducted using the Oral Hygiene Index. Data were analyzed using SPSS version 25, with p < 0.05 considered significant.
Results: Most participants (79.2%) were in their second or third trimester. Although 83.3% used toothbrushes and 52.3% brushed twice daily, 39.8% had poor oral hygiene, and 33.3% reported gingival bleeding. Despite 76.4% awareness of dental services, 53.2% had never visited a dentist. Most participants frequently consumed fruits (88.9%), vegetables (84.8%), and animal proteins (84.7%), while 43.0% consumed sugary drinks regularly. No significant association was found between dietary habits and gingival bleeding.
Conclusion: The study revealed a clear awareness–behavior gap: good knowledge of oral health did not translate into optimal hygiene practices or dental visits. Poor oral hygiene remained common, and gingival bleeding was prevalent. Although most participants had healthy diets, sugary drink intake was still high. Diet alone was not protective against gingival bleeding. Promoting effective oral hygiene and integrating dental care into prenatal programs is recommended.
DOI: 10.63475/yjm.v4i1.0035
Keywords: Gingival Bleeding, Oral Hygiene, Pregnancy, Dietary Habits, Maternal Health.
Pages: 153-159
View: 3
Download: 6
DOI URL: https://doi.org/10.63475/yjm.v4i1.0035
Publish Date: 23-05-2025
Full Text
Periodontal diseases, including gingivitis and periodontitis, are among the most common inflammatory conditions affecting the supporting structures of the teeth. Gingivitis, a reversible inflammation of the gingiva, manifests as swollen and bleeding gums, while periodontitis involves deeper destruction of periodontal tissues, potentially resulting in tooth loss. [1] Globally, periodontal diseases affect between 20% and 62% of adults, with severe periodontitis alone impacting approximately 23.6% of the population, making it the second most prevalent oral health condition worldwide. [2]
The primary aetiology of periodontal disease is poor oral hygiene, particularly the accumulation of dental plaque. [3] However, the course of periodontal disease can be modified by the important roles played by several other lifestyle factors, such as diet, smoking, stress, and physical activity. [3,4]
Pregnancy is associated with significant physiological and hormonal changes that increase susceptibility to oral diseases, especially gingivitis and periodontitis. [5,6] The prevalence of pregnancy-associated gingivitis is reported to range from 35% to 100% globally, [5] driven largely by elevated estrogen and progesterone levels that enhance vascular permeability, reduce immune responses, and exacerbate inflammatory reactions to dental plaque. [6] Additionally, shifts in the oral microbiome—particularly the proliferation of pathogenic bacteria like Porphyromonas gingivalis and Prevotella intermedia—contribute to the progression of periodontal disease during pregnancy. [7]
Beyond oral discomfort, periodontal disease during pregnancy has been linked to serious complications such as preeclampsia, gestational diabetes, fetal loss, low birth weight, and preterm delivery. [8,9] These outcomes are thought to be mediated by systemic inflammatory responses and the translocation of oral pathogens into the placental or amniotic environment. [8]
Despite the clinical significance, the burden of periodontal disease remains under-recognized and poorly managed in many low- and middle-income countries, including Nigeria. [3,10-12] Studies done in Nigeria reported low levels of Oral Hygiene awareness among pregnant women. For instance, fewer than 20% of pregnant women in a Nigerian study reported visiting a dentist during pregnancy, and only 35% brushed their teeth regularly. [11] Contributing factors include low prioritization of oral health, misconceptions about dental care during pregnancy, cost barriers, and lack of oral health referrals during antenatal care. [12]
Diet is another important modifiable lifestyle factor in pregnancy that affects periodontal health. Increased cravings and consumption of sugary foods and drinks have been associated with a higher risk of gingival bleeding—an early sign of periodontal disease—while diets rich in fruits, vegetables, and antioxidants appear protective. [4,13] Studies conducted to assess the relationship between lifestyle factors and oral health have often targeted specific populations such as pregnant women. [3,4,7,10] One key finding from such studies is that unhealthy dietary habits and inadequate oral hygiene practices, such as infrequent tooth brushing, are associated with increased gingival bleeding during pregnancy, a common indicator of periodontal disease. [4]
While these risk factors have been studied individually, few investigations, particularly in Nigeria, have explored the combined influence of dietary patterns and oral hygiene practices on gingival bleeding among pregnant women. Given the potential implications for both maternal and fetal health, a more integrated approach to assessing these associations is warranted. This study aimed to assess the relationship between dietary patterns, oral hygiene practices, and self-reported gingival bleeding among pregnant women attending the Mother and Child Hospital, Ondo, Southwest Nigeria.
Study setting and population
This study was conducted between July and October 2024 among pregnant women attending the antenatal clinic of Mother & Child Centre, University of Medical Sciences Teaching Hospital, Ondo, South West, Nigeria.
Study design
A cross-sectional descriptive study was conducted to assess the prevalence of gingival diseases among pregnant women attending the Mother & Child Clinic, Ondo, South West Nigeria.
Sample size and participant recruitment
A sample size of 216 participants was determined using Kish’s formula [14] with an adjustment for potential incomplete data or attrition. A convenience sampling technique was employed to recruit participants from the antenatal clinic of the hospital. Before participation, all individuals provided informed consent.
A sample size of 216 participants was determined using Leslie Kish’s formula.
.png)
n = Sample size
Z = Confidence level is 95%, which corresponds to 1.96
P = Expected prevalence = 0.85
The documented prevalence of pregnancy gingivitis from a previous study was 85%. [15]
q = (1-p)
q = 1− P = 1 - 0.85 = 0.15
d = the degree of accuracy desired, maximal error allowed set at 0.05
n = (1.96)2*0.85*(0.15)
(0.05)2
n = 196
Catering for an attrition rate of 10%, the above, the final sample size is:
n = 196 + 20 = 216.
Pregnant women aged 18 years and above attending the ante-natal clinic of the Mother and Child Clinic, University of Medical Sciences Teaching Hospital, over a 4‑month period constituted the study population.
Selection criteria
Inclusion criteria
Pregnant women aged 18 years and above who could comprehend and respond to the questionnaire.
Exclusion criteria
Pregnant women with neurological or cognitive disorders that impair their ability to respond to the questionnaire.
Data collection instruments and procedures
A standardized, self-administered questionnaire, adapted from a previous study [3] and administered in English language was used to collect data. The questionnaire included the following sections:
- Sociodemographic Factors: Age, education, occupation, and trimester of pregnancy.
- Perceived Oral Health Conditions: Gingival status, dental pain, periodontal disease, and dental caries.
- Oral Health Habits: Frequency of tooth brushing, use of dental floss, other oral hygiene aids, and fluoride toothpaste.
- Knowledge and Utilization of Dental Services: Awareness of dental services and frequency of dental visits.
- Nutritional Data using the pretested Food Frequency Table. [16]
- Clinical Examination: Assessment of oral hygiene status using the Simplified Oral Hygiene Index. [17]
Assessment of participants’ nutritional intake
Participants’ dietary habits were evaluated using a pretested Food Frequency Questionnaire (FFQ). [16] Respondents were asked to indicate how often they consumed items from various food groups listed in the FFQ. These food groups included fruits, vegetables, bread and cereals, milk and dairy products, meat, fish and poultry, and soft drinks.
The frequency of intake was categorized based on the following response options: daily, 4–6 times per week, less than 4 times per week, and never. Foods consumed either daily or 4–6 times per week were classified as frequently consumed, while those consumed less than 4 times per week or occasionally were classified as infrequently consumed.
Simplified Oral Hygiene Index (OHI-S) [17]
The Simplified Oral Hygiene Index (OHI-S), developed by Greene and Vermillion in 1964, is a clinical tool used to evaluate oral hygiene status by assessing the presence of debris and calculus on selected tooth surfaces. The index comprises two components: The Debris Index-Simplified (DI-S) and the Calculus Index-Simplified (CI-S), with the final score being the sum of their means. Interpretation of OHI-S scores is as follows: 0.0 – 1.2: Good oral hygiene, 1.3 – 3.0: Fair oral hygiene, and 3.1 – 6.0: Poor oral hygiene.
A pre-test was conducted with 30 patients from the antenatal clinic of a primary health care centre in the state who shared similar characteristics with the target population. Participants evaluated the clarity and comprehensibility of the questionnaire, and feedback was used to refine the instrument. Reliability was confirmed using Cronbach’s alpha, which yielded a value of 0.75, indicating good internal consistency.
Data analysis
Data entry was performed using Microsoft Excel (2016 version) and subsequently exported to SPSS Statistics for Windows Version 25.0 (IBM Corp., Armonk, NY, USA) for comprehensive analysis. [18] Descriptive statistics were used to summarize the data, presenting results as frequencies, percentages, tables, and pie charts. Inferential statistics were performed using the chi-square test and Fisher’s exact test where appropriate, with a 95% confidence interval. Statistical significance was set at p < 0.05.
Ethical considerations
Ethical clearance for the study was obtained from the University of Medical Sciences Health Research Ethics Committee, Ondo, Nigeria (NHREC/TR/UNIMED-HREC-Ondo St/22/06/21). The study’s objectives, potential benefits, and any associated risks were clearly explained to all participants before enrollment. Informed consent was obtained from each participant before data collection. Participants were assured of confidentiality, and no personally identifiable information was collected or disclosed.
Sociodemographic characteristics
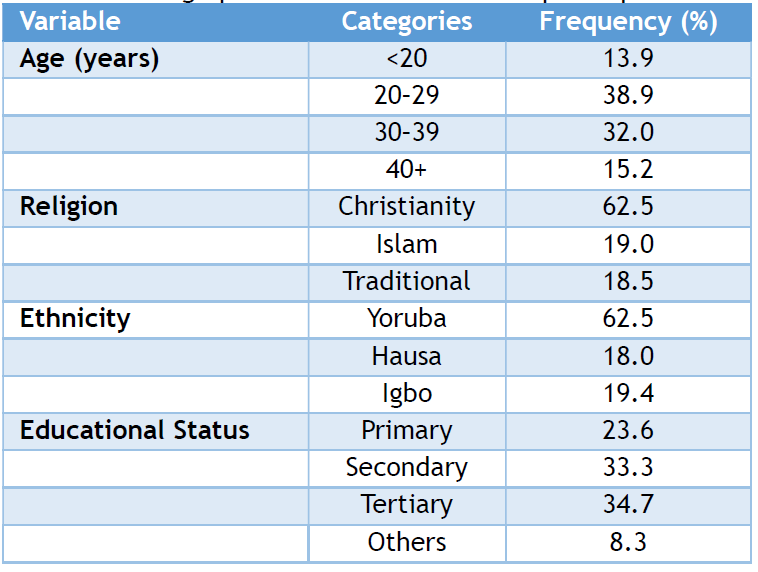
The study included 216 Nigerian pregnant women across all trimesters, with the majority in the second (39.8%) and third (39.4%) trimesters, while 13.9% were in the first trimester (Figure 1). Most of the participants (38.9%) were between 20–29 years, followed by 32.0% in the 30–39 age group. Only 13.9% were under 20 years. The majority identified as Christians (62.5%) and were of Yoruba ethnicity (62.5%). Over two-thirds of the participants had at least secondary education, with 33.3% having secondary and 34.7% tertiary level education (Table 1).
Table 1: Demographic characteristics of the participants
Oral hygiene practices
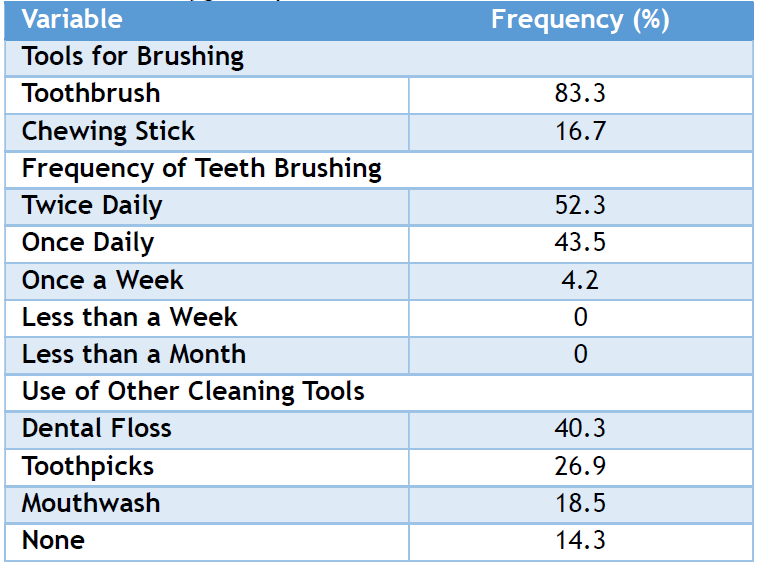
As shown in (Table 2), the majority of participants (83.3%) used a toothbrush for cleaning their teeth, while 16.7% used chewing sticks. More than half (52.3%) brushed their teeth twice daily, while 43.5% brushed once daily. Only 4.2% brushed once a week, and none brushed less frequently than that. Regarding the use of other cleaning aids, 40.3% used dental floss, 26.9% used toothpicks, and 18.5% used mouthwash. Notably, 14.3% did not use any other oral hygiene tools beyond basic brushing (Table 2).
Table 2: Oral hygiene practices
Self-reported dental problems
Regarding self-reported oral health, more than half of the women (51.4%) perceived their teeth as healthy and requiring no dental visit. However, 6.9% reported experiencing pain from a toothache, and 33.3% reported bleeding and swollen gums during pregnancy. Among those with gum disease, 48.6% did not consult a dentist (Table 3).
Table 3: Self-reported dental problems among the participants
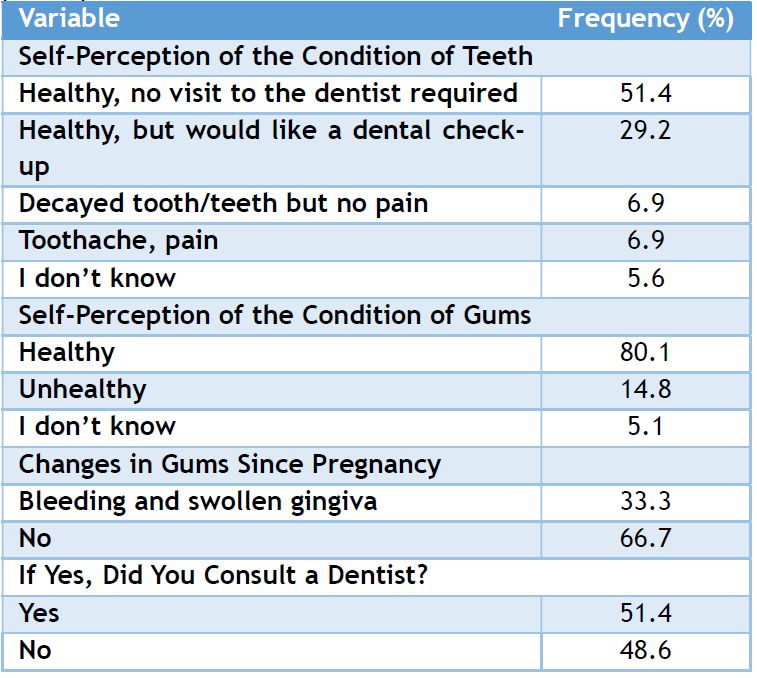
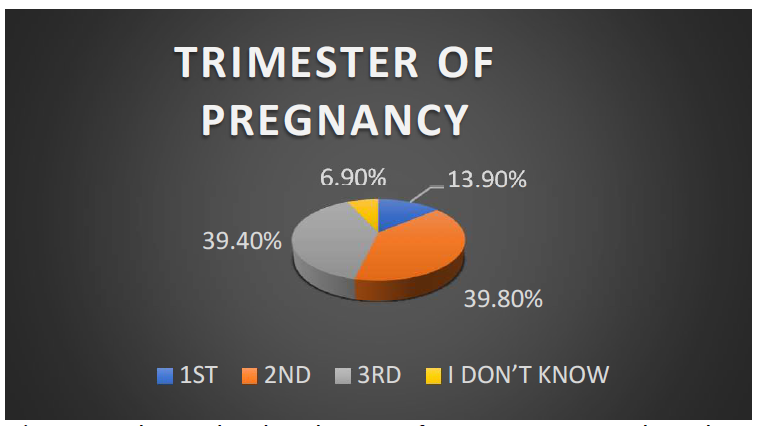
Figure 1: shows the distribution of pregnant women based on their trimester. The majority of participants (79.2%) were in their second or third trimester.
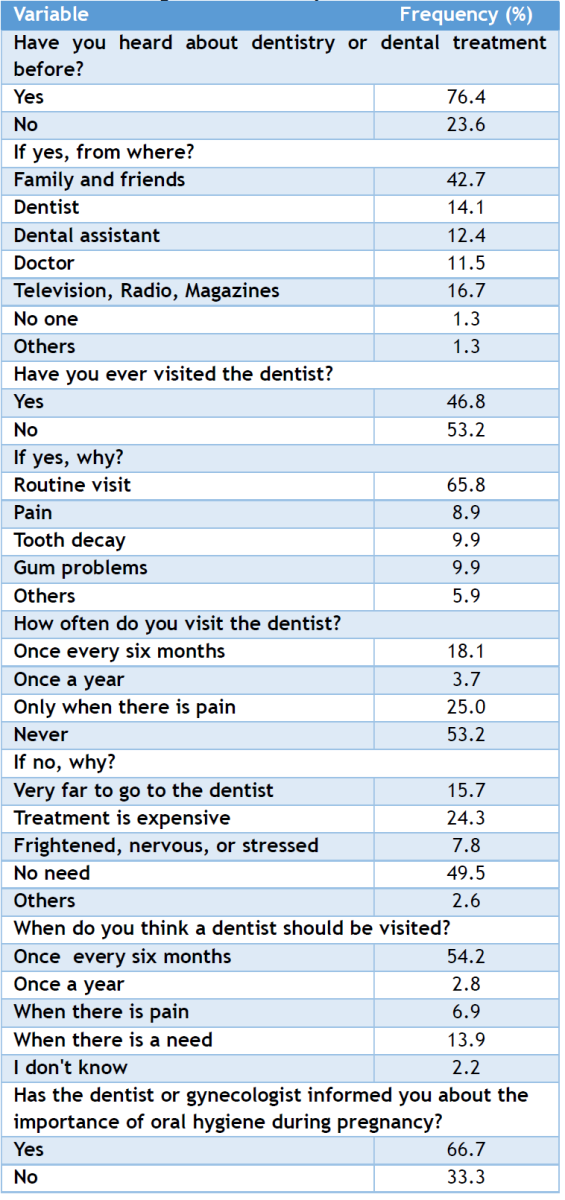
Knowledge and utilization of dental services
Awareness of dentistry or dental treatment was relatively high (76.4%), though only 14.1% received this information from dentists. Less than half (46.8%) had ever visited a dentist, and of these, 65.8% did so for routine checkups. Notably, Most participants (53.2%) had never visited a dentist, with the most common reasons being no perceived need (49.5%), high treatment costs (24.3%), and long distance to dental facilities (15.7%). When asked about the appropriate time to visit a dentist, 54.2% believed it should be once every six months. Additionally, 66.7% of respondents reported being informed by a dentist or gynecologist about the importance of oral hygiene during pregnancy, while 33.3% had not received such information. (Table 4).
Table 4: Knowledge about dentistry
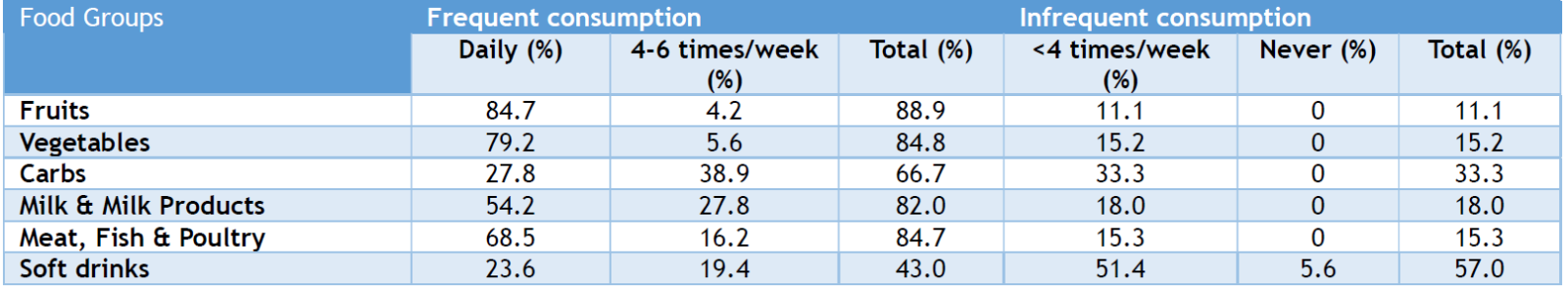
Nutritional practices
Most pregnant women reported frequent consumption of healthy food groups, with fruits (88.9%), vegetables (84.8%), and animal-source proteins (meat, fish, and poultry – 84.7%) being the most commonly consumed. Milk and milk products were also frequently consumed by 82.0% of participants. However, only 66.7% frequently consumed carbohydrate-rich foods. Notably, 43.0% of the women reported frequent consumption of soft drinks, indicating a considerable intake of sugary beverages, while 5.6% never consumed them. (Table 5).
Table 5: Nutritional information
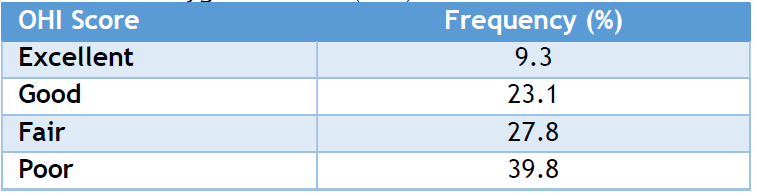
Oral hygiene status
The oral hygiene status among participants varied widely. Only 9.3% had excellent oral hygiene, and 23.1% were categorized as having good oral hygiene. However, a significant portion had fair (27.8%) or poor (39.8%) oral hygiene. Altogether, 67.6% of participants had suboptimal oral hygiene (fair or poor), indicating a need for improved oral health education and services among pregnant women (Table 6).
Table 6: Oral hygiene status (OHI)
This study included 216 pregnant women attending the Mother and Child Hospital, Ondo, South West Nigeria. Most participants were in their second and third trimesters, similar to findings among pregnant women in Saudi Arabia and the USA. [19, 20] This may be attributed to the common practice of registering for antenatal care during these trimesters.
A striking and somewhat unexpected finding was the disconnect between good oral hygiene awareness and actual oral hygiene status. Although 83.3% of respondents used toothbrushes and 52.3% brushed twice daily, which is consistent with findings from studies in Lagos [3] and Benin City, [21] oral hygiene assessment showed that 67.6% had suboptimal hygiene. This finding aligns with studies in Australia [22] and Saudi Arabia, [4] and suggests that brushing frequency alone may not ensure good oral health, especially without proper brushing techniques and adjunct cleaning methods like flossing. Similarly, despite 76.4% of participants being aware of dental services, over half (53.2%) had never visited a dentist. This awareness-utilization gap was also reported in Nigeria [3] and the United States. [20] The reported rate of regular dental visits during pregnancy (18.1%) aligns with findings from Benin City, Nigeria (19.8%), [21] Saudi Arabia (18.1%); [4] but at variance with rates reported in Australia (30%),[22] Kuwait (52%)[23], UAE (58.3%) [24] and Italy (59.9%). [25] Many pregnant women learned about dentistry and dental treatments from family and friends rather than professionals. Cost, perceived lack of need, and distance were key barriers. These findings reflect structural limitations in access to oral health care and underscore a need for system-level interventions.
The prevalence of self-reported gingival bleeding (33.3%) is noteworthy. It is higher than previously reported rates in the UAE (23.5%) [24] and certain regions of Nigeria, including Benin (18.8%) [21] and Lagos (27.2%), [3] but lower than the prevalence reported among Chinese women in Singapore (over 60%) [26] and pregnant women in Saudi Arabia (65%). [4]
The absence of a significant association between dietary habits and gingival bleeding is consistent with earlier Nigerian [3] and Pakistani [27] studies. This reinforces the understanding that while diet contributes to general oral health, it cannot substitute for proper hygiene practices in preventing periodontal conditions like gingivitis. Notably, a previous study [28] has reported that diets in many developing countries typically contain low amounts or a complete absence of protein from animal sources. However, this study revealed a higher proportion of frequent animal protein consumption, with 84.7% of participants consuming such foods regularly. This figure exceeds earlier findings in Borno (67.3%) [29] and Lagos (73.4%), [3] suggesting an improvement in nutritional quality among pregnant women in Ondo. This higher intake of animal protein may reflect increased nutritional awareness or better access to protein-rich foods, both of which have implications for overall maternal and fetal health.
Most participants reported good dietary practices, including high daily intake of fruits (84.7%) and vegetables (79.2%), which contrasts with reports from Saudi Arabia [4] where low fruit and vegetable intake was associated with higher periodontal risk. Conversely, 43.0% of the women in this study reported frequent consumption of sugary drinks, a much higher prevalence compared to the 25.7% reported in Lagos. [3] This finding is concerning given the well-established role of sugar in increasing the risk of dental caries and potentially worsening periodontal conditions.[30]
It further underscores the need for dietary counseling during antenatal visits to reduce sugar intake and promote oral health. Overall, this study highlights a critical gap between knowledge and behavior—an important public health insight. It suggests that interventions in pregnancy should go beyond education and address the behavioral and systemic factors that impede effective oral care.
Limitation
A key limitation of this study, conducted in Ondo, Southwest Nigeria, is the reliance on self-reported data, which may be affected by recall bias and social desirability bias—common challenges in questionnaire-based research.
The study reveals that despite good awareness of oral hygiene and healthy dietary practices among pregnant women in Ondo, Nigeria, there remains a high prevalence of poor oral hygiene and self-reported gingival bleeding. A novel contribution of this study is the identification of a significant awareness-behavior gap, where knowledge of oral health does not necessarily translate into optimal hygiene practices or routine dental visits.
The absence of a statistically significant link between diet and gingival bleeding further confirms that dietary practices alone cannot compensate for poor oral hygiene in preventing periodontal disease during pregnancy. This finding emphasizes the need for a multifaceted approach that includes education, behavior change, and access to care.
To improve oral health among pregnant women, oral hygiene education should be strengthened during antenatal visits, with emphasis on proper brushing techniques and the use of additional hygiene tools. Routine dental check-ups should be integrated into antenatal care to facilitate early detection and treatment of gum issues.
Nutrition counseling should also highlight the importance of balanced diets rich in animal-source proteins while discouraging frequent consumption of sugary drinks. Collaboration between dentists, gynecologists, and nutritionists is essential to deliver consistent health messages and promote better maternal oral health outcomes.
AUTHORS’ CONTRIBUTION
Each author has made a substantial contribution to the present work in one or more areas, including conception, study design, conduct, data collection, analysis, and interpretation. All authors have given final approval of the version to be published, agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
SOURCE OF FUNDING
None.
CONFLICT OF INTEREST
None.
References
- Chow AW. Infections of the oral cavity, neck, and head. In: Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia: WB Saunders; 2015. p. 789-805.
- Trindade D, Carvalho R, Machado V, Chambrone L, Mendes JJ, Botelho J. Prevalence of periodontitis in dentate people between 2011 and 2020: a systematic review and meta‐analysis of epidemiological studies. J Clin Periodontol. 2023 May;50(5):604-26.
- Onigbinde OO, Olajugba GO, Oyapero A. Dietary pattern, oral hygiene and self-reported gingival bleeding in pregnant women in Lagos State. Adv Hum Biol. 2021 Jan 1;11(1):73-8.
- Gaffar BO, El Tantawi MA, AlAgl AS, Al-Ansari A. Food intake, oral hygiene and gingival bleeding in pregnancy: does lifestyle make a difference? A cross-sectional exploratory study. Int J Health Sci (Qassim). 2016;10:13–20.
- Moss KL, Beck JD, Offenbacher S. Clinical risk factors associated with incidence and progression of periodontal conditions in pregnant women. J Clin Periodontol. 2005 May;32(5):492-8.
- Hemalatha VT, Manigandan T, Sarumathi T, Aarthi Nisha V, Amudhan A. Dental considerations in pregnancy-a critical review on the oral care. J Clin Diagn Res. 2013 Mar 21;7(5):948.
- Sachelarie L, Iman AEH, Romina MV, Huniadi A, Hurjui LL. Impact of Hormones and Lifestyle on oral health during pregnancy: a prospective observational regression-based study. Medicina (Kaunas). 2024 Oct 30;60(11):1773. PMID: 39596958; PMCID: PMC11596282.
- Shanthi, V, Vanka, A, Bhambal A, Saxena, V, Saxena, S, Kumar, SS. Association of pregnant women periodontal status to preterm and low-birth weight babies: a systematic and evidence-based review. Dent Res J. 2012;9:368–80.
- Offenbacher S, Boggess KA, Murtha AP, Jared HL, Lieff S, McKaig RG, et al. Progressive periodontal disease and risk of very preterm delivery. Obstet Gynecol. 2006 Jan;107(1):29-36.
- Ugwa EA. Nutritional practices and taboos among pregnant women attending antenatal care at general hospital in Kano, Northwest Nigeria. Ann Med Health Sci Res. 2016;6(2):109-14.
- Okunaiya G, Fadupin G, Oladeji D. Knowledge, attitude and practice of maternal and child food-based dietary guidelines among pregnant women in urban slum of Lagos State. Clin Mother Child Health. 2016;13(2):240.
- Rocha JS, Arima L, Chibinski AC, Werneck RI, Moysés SJ, Baldani MH. Barriers and facilitators to dental care during pregnancy: a systematic review and meta-synthesis of qualitative studies. Cad Saude Publica. 2018 Sep 6;34:e00130817.
- Murphey C, Fowles E. Dental health, acidogenic meal, and snack patterns among low-income women during early pregnancy: a pilot study. J Midwifery Womens Health. 2010 Nov; 55(6):587-92.
- Kish L. Sampling organizations and groups of unequal sizes. Am Sociol Rev. 1965 Aug;30(4):564-72.
- Soroye MO, Ayanbadejo PO. Prevalence of gingivitis and perception of gingival colour among pregnant women attending the antenatal clinic of Lagos University Teaching Hospital, Idi-Araba. J Orofac Sci. 2016;8:53-9.
- Ogunkunle MO, Oludele AS. Food intake and meal pattern of adolescents in school in Ila Orangun, South-West Nigeria. S Afr J Clin Nutr. 2013;26:188–93.
- Greene JC, Vermillion JR. The simplified oral hygiene index. J Am Dent Assoc. 1964;68:713.
- IBM Corp. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp;2011.
- Kawkab MA, Al-Turck KM. Self-reported dental care and dietary habits of Saudi pregnant women in prenatal clinic in Riyadh. Pak Oral Dent J. 2005;25(1):75-80.
- Gaffield ML, Gilbert BJ, Malvitz DM, Romaguera R. Oral health during pregnancy: an analysis of information collected by the pregnancy risk assessment monitoring system. J Am Dent Assoc. 2001 Jul;132(7):1009-16.
- Azodo CC, Omuemu VO. Perceived oral health, oral self-care habits and dental attendance among pregnant women in Benin-City, Nigeria. Tanzan Dent J. 2012;17:459.
- Thomas, NJ, Middleton PF, Crowther CA. Oral and dental health care practices in pregnant women in Australia: a postnatal survey. BMC Pregnancy Childbirth. 2008;8:13.
- Honkala S, Al-Ansari J. Self-reported oral health, oral hygiene habits, and dental attendance of pregnant women in Kuwait. J Clin Periodontol. 2014;32:809-14.
- Hashim R. Self-reported oral health, oral hygiene habits and dental service utilization among pregnant women in United Arab Emirates. Int J Dent Hyg. 2012;10:142-6.
- Villa A, Abati S, Pileri P, Calabrese S, Capobianco G, Strohmenger L et al. Oral health and oral diseases in pregnancy: a multicentre survey of Italian postpartum women. Aust Dent J. 2013; 58:224-9.
- Balan P, He HG, Cao F, Wong ML, Chong YS, Lopez V, et al. Oral health in pregnant Chinese women in Singapore: a call to go beyond the traditional clinical care. Healthcare (Basel). 2018 Jul 9;6(3):77.
- Ghazal M, Zaidi SJ, Riaz S, Farooqi WA. Influence of socio-cultural variables on periodontal conditions in pregnant Women. Pak Oral Dent J. 2017 Jun;37(2):294-301.
- Willy K, Judith K, Peter C. Dietary diversity,nutrient intake and nutritional status among pregnant women in Laikipia County, Kenya. Int J Health Sci Res. 2016;6:378–85.
- 29.Kever RT, Martins SD, Lola N, Dathini H, Habu H, Fatima AA, et al. Knowledge and attitude of pregnant women towards dietary practices in Yerwa Clinic, Maiduguri Metropolitan Council; Borno State. J Res Nurs Midwifery. 2015 Jan;4(1):12-9.
- Tomar N, Gupta C, Kaushik M, Wadhawan A. Nutrigenomics: a perionutrition interrelationship. J Oral Res Rev. 2017;9:326.
