Full HTML
Outcome of COVID-19 Positive Patients with type 2 Diabetes and Polypharmacy: an Examination of a Tertiary Hospital Cohort
Mohammed Danjuma1, Bhagya Sree2, Unwam jumbo3, Lina Al Tarawneh4, Rowan Mesilhy4, Aly Roa4, Hend AlObaidi4, Amal H ElMasaad4, Gamal AlFitori3, Islam Elzouki3 Lina Naseralallah2,5
Author Affiliation
1 Consultant, Department of Medicine, Weill Cornell College of medicine, Internal medicine residency training program, Qatar university college of Medicine, Doha Qatar,
2 Pharmacist, clinical pharmacy division, Hamad Medical Corporation, Doha Qatar
3 Consultant, Internal medicine residency training program, Department of Medicine, hamad medical corporation, Doha Qatar,
4 Consultant, Department of Medicine, Qatar university college of medicine
5 Pharmacist, School of pharmacy, university of Birmingham, Birmingham, united kingdom
Abstract
Background: COVID-19-positive patients are at increased risk of adverse clinical outcomes, with type 2 diabetes cohorts at substantially higher risk compared to the general population. The additional role of diabetic and non-diabetic polypharmacy in these patients' clinical course has remained unexamined. In this study we have comprehensively examined the role of polypharmacy in the determination of mortality outcomes in patients with COVID-19 clinical syndrome.
Methods: We retrospectively examined case notes and electronic records of N = 497 patients with type 2 diabetes and COVID-19 infection. We ascertained the number of medications each patient was taking and used this to categorize the study cohort into diabetic [n = 246] (5 or more diabetic medications), and non-diabetic polypharmacy [n = 251] (5 or more non-diabetic medications). The primary outcome was the need for intensive care admission between the two groups.
Results: In patients with “non-diabetic polypharmacy” (>5 medications), advancing age, and higher HBA1c levels, were associated with increased risk of Intensive care admission (OR 1.06 [CI 1.03-1.07], P = <0001), (OR 1.01 [CI 1.01- 1.20], P 0.017), respectively. Patients taking 5 or more non-diabetic medications had an increased likelihood of admission into the intensive care unit compared to those on lower medication thresholds (OR = 1.7; CI = 1.1 to 1.3; p-value = <0.0006).
Conclusion: In an inpatient cohort of type 2 diabetic patients with COVID-19, non-diabetic polypharmacy was associated with a multiplicative risk of intensive care admissions. This will necessitate the need for periodic medication reviews
DOI: 10.63475/yjm.v4i1.0051
Keywords: COVID-19, polypharmacy, Diabetes Mellitus, adverse drug reactions
Pages: 117-122
View: 9
Download: 13
DOI URL: https://doi.org/10.63475/yjm.v4i1.0051
Publish Date: 22-05-2025
Full Text
Despite the uptake of COVID-19 vaccination programs around the world as part of the comprehensive attempt at addressing its rising morbidity and mortality, the evolution of new variants of the virus has continued to be a source of ongoing concerns.
In this study, we have explored the pattern and the clinical phenotype of diabetic and non-diabetic polypharmacy in patients with T2DM and COVID-19, as well as its impact on the risks of potentially adverse clinical outcomes such as intensive care unit (ITU) admissions.
Study design and setting
This retrospective study examined case notes and electronic records of a randomly selected cohort of patients (n=2014) with type 2 Diabetes Mellitus and a confirmed diagnosis of COVID-19 presenting to the Hamad General Hospital, Doha, Qatar between March 2020 and December 2020. This is a tertiary healthcare facility with a capacity of 600 beds, catering to patients referred from other primary and secondary healthcare centers in the state of Qatar. The number of medications each patient was cumulatively prescribed was abstracted from an online prescription platform (Cerner®). Disordered glycemic control often accompanies COVID-19 infection, consequently, we did not censure the timing of medications included in the patient's total medication list, as some of these patients had either insulin or other diabetic drugs added to their medication list upon diagnosis of COVID-19 to optimize their glycemic control. Other variables abstracted include age (then categorized into 18-25, 26-35, 36-45, 46-55, 56-65, 66-75 years), gender, self-declared ethnicity, eGFR, alanine aminotransferase (ALT), aspartate aminotransferase (AST), serum interleukin 6 (IL-6), serum ferritin, serum D-dimer, length of hospital stay, and intensive care unit (ITU) admission. The primary outcome was admission to the ITU. We chose ITU admission as a surrogate marker of COVID-19 severity as it has previously been reported as a reliable index of COVID-19 interventions (including various pharmaco- and immunotherapies)
Study population
Type 2 diabetic patients with COVID-19 infection confirmed by nasopharyngeal swab polymerase chain reaction (PCR). We included all diabetic patients regardless of the duration of diagnosis.
Inclusion and exclusion criteria
The inclusion criteria were
- New or preexisting diagnoses of type 2 diabetes
- COVID-19 infection.
- On index medication for at least 4 months
The exclusion criteria include the Unavailability of data
Sample size
Given the prevalence of COVID-19 in Qatar of 16.2%, we estimate that a sample size of 2014 is likely to give us about 80% power to detect the differential effect of diabetic polypharmacy on COVID-19 clinical outcomes.
Case ascertainment and definitions.
In this study,
- “Diabetic” polypharmacy was defined as the intake of 5 or more diabetic medications (including insulin). A different cohort of type 2 diabetic patients taking 5 or more non-diabetic medications (and fewer than 5 diabetic medications) was classified as having “non-diabetic” polypharmacy.
- A positive COVID-19 case refers to patients with positive PCR from a nasopharyngeal swab.
Statistical analyses
Continuous variables were compared and summarized as means (±SD) or medians (interquartile range [IQR]) using ANOVA and Kruskal-Wallis, depending on the distribution as appropriate. Differences in the distribution of categorical variables were determined by Chi-squared tests. Correlation coefficients were derived to ascertain the correlation between study variables. Bivariate analyses were utilized to determine the relationship between study variables and risk of intensive care admissions. Multivariate regression models were generated to determine factors associated with the risk of ITU admission in type 2 diabetic patients who are COVID-19 positive. These include specific outcome comparisons between “major” and “minor” polypharmacy, as well as “diabetic” and “non-diabetic” polypharmacy. All analyses were carried out with Stata Statistical Software (Stata Corp. 2019. Release 16. College Station, TX: Stata Corp LLC)
Ethical approval
The protocol and various documentation for this study, including consent to access the records of participants in the study, were reviewed and approved by the independent review board of the medical research center (MRC-01-21-167).
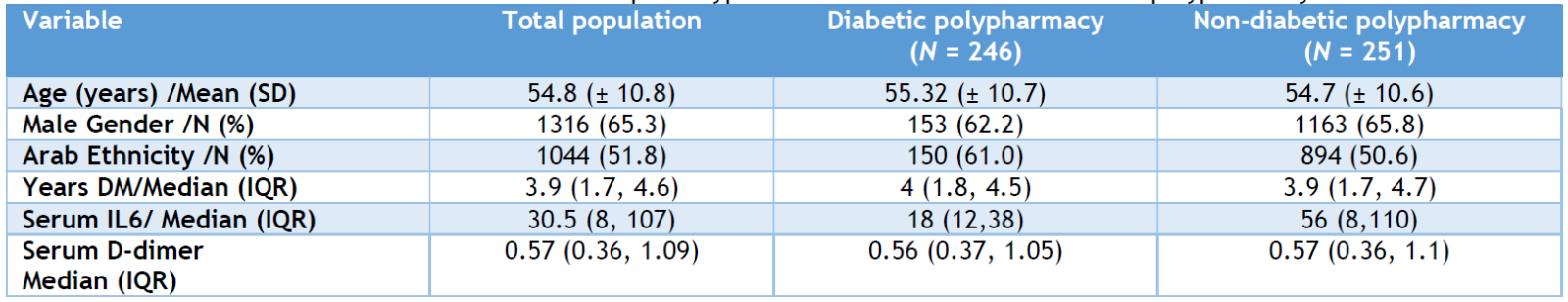
The baseline characteristics of the study population are shown in Table 1. Amongst an inpatient cohort of N = 2014 T2DM patients with COVID-19, the proportion of the study population with “diabetic” and “non-diabetic” polypharmacy was (N = 246, and N = 251, respectively). The mean age of the study cohort was 54.8 [SD ±10] years, with a male population of 65.3%. The median number of comorbidities was 4 (interquartile range 2-8). About 94.5% of the study population was on an insulin-based regimen. The distribution of drug classes amongst patients with “diabetic” and “non-diabetic polypharmacy” is shown in Tables 4 and 5.
Table 1: Baseline characteristics of different clinical phenotypes of “diabetic” and “non-diabetic polypharmacy
Diabetic vs. Non-Diabetic Polypharmacy
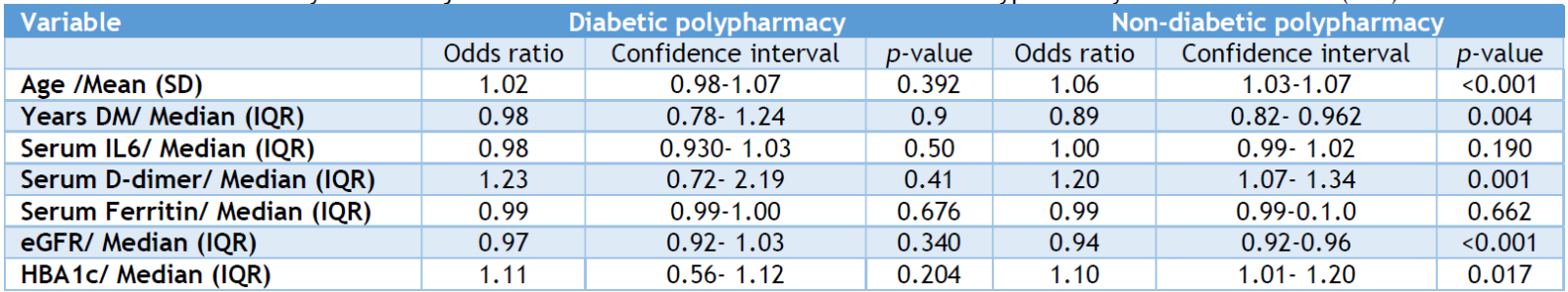
The adjusted ORs (AORs) and their 95% CIs derived from multivariable logistic regression models are given in Table 2. The presence of non-diabetic polypharmacy (5 or more non-diabetic medications) was associated with increased risk of Intensive care admission (Odds ratio = 1.7 [Confidence interval (CI) 1.1 to 1.3]; p = 0.0006). In patients with non-diabetic polypharmacy, advancing age, higher HBA1c levels, and every additional year since diagnosis of diabetes were associated with increased risk of Intensive care admission (OR 1.06 [CI 1.03-1.07], P = <0001), (OR 1.01 [CI 1.01- 1.20]), (OR 0.9 [0.82- 0.962]) respectively. We found out of the three markers of endothelial injury evaluated (viz. serum Ferritin, IL-6, and D-dimer), only rising serum D-dimer levels were associated with a doubling of the risk of Intensive care monitoring in patients with nondiabetic polypharmacy but with an uncertain point estimate (OR 1.07 [CI 1.07- 1.34]. Of note, none of the tested covariates were predictive of ITU admissions in patients with diabetic polypharmacy (5 or more diabetic medications, including insulin).
Table 2: Multivariate analyses and adjusted odds ratios for the effect of Diabetic Polypharmacy on intensive care (ITU) admissions
The cumulative effect of age on the risk of intensive therapy unit (ITU) admissions
We additionally explored the differential effect of age categories on the risk of ITU admissions in the setting of COVID-19 in patients with non-diabetic polypharmacy and evidence of “endotheliopathy” as evidenced by raised D-dimer. Patients with raised D-dimer levels within the age categories (56-65 and 66-75 years) were associated with increased risk of ITU admissions (OR = 1.11 [CI 1.00-1.23], p = 0.041), (OR = 1.47 [CI 1.02-2.13], p = 0.041) respectively. See Table 3
Table 3: Cummulative effect of age category on ITU admissions in type 2 Diabetic patients with COVID-19 and established markers of endothelial dysfunction (raised D-dimer levels)
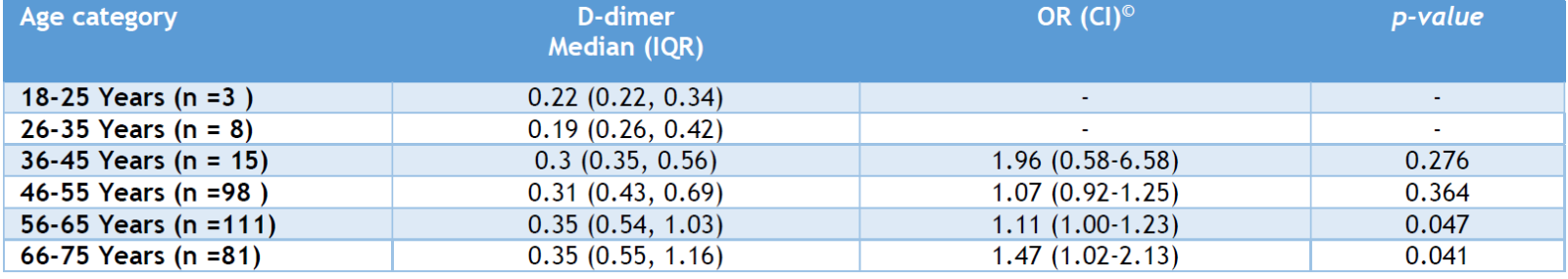
Table 4. Drug classes among patients with non-diabetic polypharmacy phenotypes
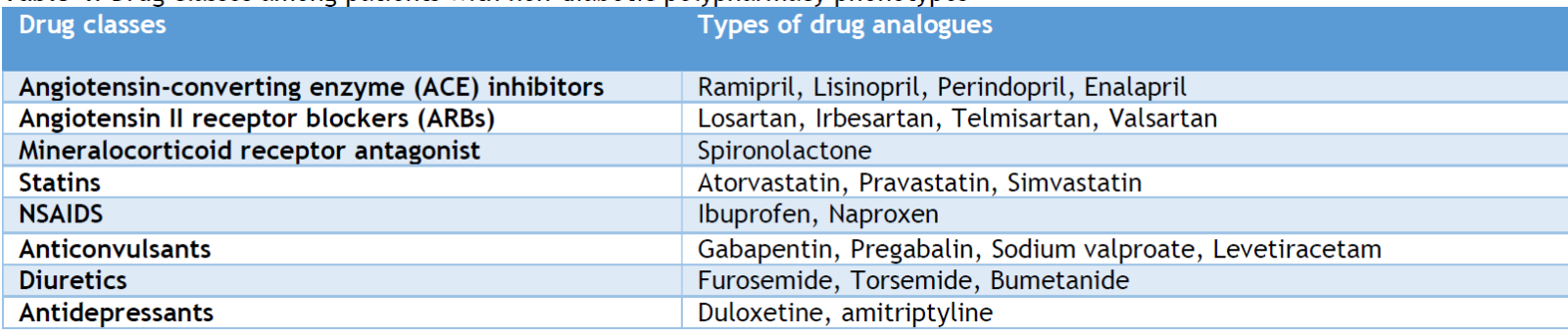
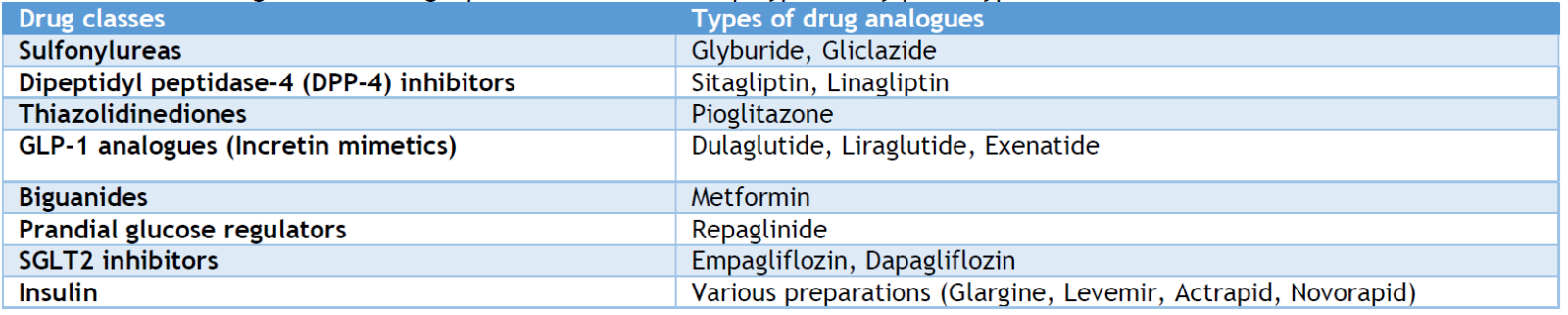
Table 5. Diabetic drug classes amongst patients with Diabetic polypharmacy phenotypes
To our knowledge, this study’s examination of different polypharmacy phenotypes and their impact on COVID-19 ITU-related admissions represents the first comprehensive exploration of the association between this rising therapeutic morbidity and adverse outcomes in these cohorts of patients. We found a 2-fold increase in the risk of ITU admissions amongst patients taking more than 5 non-diabetic medications compared to those on lower medication thresholds or taking 5 or more diabetic drugs. This will call for increased vigilance and the institution of mitigation strategies to address this additional risk factor in these patient cohorts who are already at increased risk of ITU admissions. Our findings are consistent with recent reports that have investigated polypharmacy and multimorbidity in COVID-19 patients
Our finding of differences in outcomes between patients with non-diabetic polypharmacy compared to those with diabetic polypharmacy is interesting. The lack of demonstrable adverse outcomes with the latter (by way of ITU admissions) will reinforce the earlier findings from previous reports on the role of optimal glycemic control in mitigating COVID-19 adverse clinical outcomes.
Our finding of increased risk of ITU admissions for each additional year since the diagnosis of T2DM for both diabetic and non-diabetic polypharmacy may denote the duration of T2DM as a surrogate marker of associated T2DM complications (including micro and macrovascular diseases). These complications have been well established to be a factor of the length of T2DM, amongst other factors. The presence of these overt and sub-clinical complications, therefore, perhaps plays an additional yet-to-be-determined role in promoting endothelial dysfunction, a key driver of deterioration and the need for supportive intensive monitoring in patients with COVID-19 infection.
We observed that a sizable proportion of our study population was on insulin (94.5%). The impact of tight glycemic control on favorable COVID-19 outcomes has been exhaustively explored elsewhere.
Strengths and limitations
The novelty of our report lies in being the first attempt at investigating the relationship between various phenotypes of polypharmacy in T2DM with COVID-19 clinical syndrome and adverse outcomes. Our findings both reinforced earlier observations in this area, but also reported several potential hypothesis-generating observations that will assist in the design of future studies in this area.
Our use of a retrospective data scheme meant that we had to deal with missing values as well as other issues encountered with retrospective study designs. But notwithstanding that, the consistency of our final point estimates across key report observations meant that this limitation is unlikely to affect any potential inference from our report.
In a population of type 2 diabetic patients with COVID-19 infection, non-diabetic polypharmacy in the setting of advancing age and rising HBA1c levels was associated with multiplicative risks of adverse clinical outcomes such as intensive care admission. This will necessitate the need for periodic medication reviews in these cohorts of patients to mitigate these potential risks and improve clinical outcomes.
AUTHORS' CONTRIBUTION
Each author has made a substantial contribution to the present work in one or more areas, including conception, study design, conduct, data collection, analysis, and interpretation. All authors have given final approval of the version to be published, agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work
SOURCE OF FUNDING
None
CONFLICT OF INTEREST
None
References
- Rubin EJ, Baden LR, Abdool Karim SS, Morrissey S. Audio Interview: The Omicron Variant of SARS-CoV-2. New England Journal of Medicine. 2021; 385(23):e96.
- Cele S, Jackson L, Khoury DS, Khan K, Moyo-Gwete T, Tegally H, et al. Omicron extensively but incompletely escapes Pfizer BNT162b2 neutralization. Nature. 2022; 602(7898):654-656
- McQueenie R, Foster HME, Jani BD, Katikireddi SV, Sattar N, Pell JP, et al. Multimorbidity, polypharmacy, and COVID-19 infection within the UK Biobank cohort. PLoS One. 2020; 15(8):e0238091.
- Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, et al. Dexamethasone in Hospitalized Patients with C
- Pfizer’s Novel COVID-19 Oral Antiviral Treatment Candidate Reduced Risk of Hospitalization or Death by 89% in Interim Analysis of Phase 2/3 EPIC-HR Study: available at: https://www.pfizer.com/news/press-release/press-release-detail/pfizers-novel-covid-19-oral-antiviral-treatment-candidate [Accessed on 23/12/2022]
- Cully M. A tale of two antiviral targets — and the COVID-19 drugs that bind them. Nat Rev Drug Discov. 2022; 21(1):3-5.
- European Medicines Agency. EMA endorses use of dexamethasone in COVID-19 patients on oxygen or mechanical ventilation. Available at: https://www.ema.europa.eu/en/news/ema-endorses-use-dexamethasone-covid-19-patients-oxygen-or-mechanical-ventilation#:~:text=Based%20on%20the%20review%20of,(drip)%20into%20a%20vein. . [Accessed on 21/12/2022]
- Danjuma MI, Sinha U, Fatima H, Mohamed MFH, Nathoe H. QTc evaluation in COVID-19 patients treated with chloroquine/hydroxychloroquine: A letter to the editor. Eur J Clin Invest. 2020; 50(11):e13407.
- Porter B, Arthur A, Savva GM. How do potentially inappropriate medications and polypharmacy affect mortality in frail and non-frail cognitively impaired older adults? A cohort study. BMJ Open. 2019; 9(5):e026171.
- Dhalwani NN, Fahami R, Sathanapally H, Seidu S, Davies MJ, Khunti K. Association between polypharmacy and falls in older adults: A longitudinal study from England. BMJ Open. 2017; 7(10):e016358.
- Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017; 17(1):230.
- Grant RW, Devita NG, Singer DE, Meigs JB. Polypharmacy and medication adherence in patients with type 2 diabetes. Diabetes care. 2003; 26(5):1408–12.
- da Silva MRR, Diniz LM, dos Santos JBR, Reis EA, da Mata AR, de Araújo VE, et al. Drug utilization and factors associated with polypharmacy in individuals with diabetes mellitus in Minas Gerais, Brazil. Ciencia e Saude Coletiva. 2018; 23(8): 2565-2574
- Kow CS, Hasan SS. Mortality risk with preadmission metformin use in patients with COVID-19 and diabetes: A meta-analysis. Journal of medical virology. J Med Virol. 2021; 93(2):695-697.
- Crouse A, Grimes T, Li P, Might M, Ovalle F, Shalev A. Metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes. Front Endocrinol. 2021;11: 600439..
- Jain V, Yuan JM. Predictive symptoms and comorbidities for severe COVID-19 and intensive care unit admission: a systematic review and meta-analysis. Int J Public Health. 2020;65(5): 533-546.
- Sirois C, Boiteau V, Chiu Y, Gilca R, Simard M. Exploring the associations between polypharmacy and COVID-19-related hospitalisations and deaths: a population-based cohort study among older adults in Quebec, Canada. BMJ open. 2022; 12(3):e060295.
- Do JY, Kim SW, Park JW, Cho KH, Kang SH. Is there an association between metformin use and clinical outcomes in diabetes patients with COVID-19? Diabetes Metab. 2021;47(4):101208
- Bramante CT, Ingraham NE, Murray TA, Marmor S, Hovertsen S, Gronski J, et al. Metformin and risk of mortality in patients hospitalised with COVID-19: a retrospective cohort analysis. Lancet Healthy Longev. 2021;2(1): e34-e41.
- Saand AR, Flores M, Kewan T, Alqaisi S, Alwakeel M, Griffiths L, et al. Does inpatient hyperglycemia predict a worse outcome in COVID-19 intensive care unit patients? J Diabetes. 2021;13(3): 253-260
- Esam Z. A proposed mechanism for the possible therapeutic potential of Metformin in COVID-19. Diabetes Res Clin Pract. 2020; 167:108282.
- Parray A, Mir FA, Doudin A, Iskandarani A, Danjuma MM, Kuni RAT, et al. SnoRNAs and miRNAs Networks Underlying COVID-19 Disease Severity. Vaccines (Basel). 2021; 9(10):105623.
- Gupta JK, Ravindrarajah R, Tilston G, Ollier W, Ashcroft DM, Heald AH. The association of polypharmacy with COVID-19 outcomes independent of comorbidities in people with type 2 diabetes: implications for the unforeseen consequences of polypharmacy. Cardiovasc Endocrinol Metab. 2024 May 23;13(2):e0304.
- Formiga F, Vidal X, Agustí A, Chivite D, Rosón B, Barbé J, et al. Potentially Inappropriate Prescription in Older Patients in Spain (PIPOPS) Investigators' Project. Inappropriate prescribing in elderly people with diabetes admitted to hospital. Diabet Med. 2016; 33(5):655-62
- Cheng X, Liu Y-M, Li H, Zhang X, Lei F, Qin J-J, et al. Metformin Is Associated with Higher Incidence of Acidosis, but Not Mortality, in Individuals with COVID-19 and Pre-existing Type 2 Diabetes. Cell metabolism. 2020; 32(4):537-547.e3
- Reiterer M, Rajan M, Gómez-Banoy N, Lau JD, Gomez-Escobar LG, Ma L, Gilani A, et al. Hyperglycemia in acute COVID-19 is characterized by insulin resistance and adipose tissue infectivity by SARS-CoV-2. Cell Metab. 2021; 33(11):2174-2188.e5
- Yang Y, Cai Z, Zhang J. Hyperglycemia at admission is a strong predictor of mortality and severe/critical complications in COVID-19 patients: a meta-analysis. Biosci Rep. 2021; 41(2):BSR20203584
- Bode B, Garrett V, Messler J, McFarland R, Crowe J, Booth R, Klonoff DC. Glycemic Characteristics and Clinical Outcomes of COVID-19 Patients Hospitalized in the United States. J Diabetes Sci Technol. 2020; 14(4):813-821.
- Tharmarajah E, Buazon A, Patel V, Hannah JR, Adas M, Allen VB, et al. IL-6 inhibition in the treatment of COVID-19: A meta-analysis and meta-regression. J Infect. 2021; 82(5):178-185.
- Eljilany I, Elzouki AN. D-dimer, fibrinogen, and il-6 in covid-19 patients with suspected venous thromboembolism: A narrative review. Vol. 16, Vascular Health and Risk Management. 2020; 16:455-462
- Potere N, Batticciotto A, Vecchié A, Porreca E, Cappelli A, Abbate A, et al. The role of IL-6 and IL-6 blockade in COVID-19. Expert Review of Clinical Immunology. 2021; 17(6): 601-618
- Chen L, Sun W, Liu Y, Zhang L, Lv Y, Wang Q, et al. Association of Early-Phase In-Hospital Glycemic Fluctuation With Mortality in Adult Patients With Coronavirus Disease 2019. Diabetes Care. 2021;44(4): 865-873
