Full HTML
Learning and Teaching in Internal Medicine Teams in Hamad General Hospital, Qatar: A Resident Journey in ACGME-I Accredited Program Outside the United States
Mohanad Faisal1
Author Affiliation
1 Fellowship, General internal medicine department/ Hamad General, Doha, Qatar.
Abstract
NO ABSTRACT
DOI: 10.63475/yjm.v4i1.0072
Pages: 1-4
View: 82
Download: 76
DOI URL: https://doi.org/10.63475/yjm.v4i1.0072
Publish Date: 21-05-2025
Full Text
The Internal Medicine Residency Program at Hamad Medical Corporation (HMC) is accredited by the Accreditation Council for Graduate Medical Education–International (ACGME-I). Upon completion, residents are awarded both the Arab Board and Qatari Board certifications. This four-year program involves rotations across general internal medicine and its subspecialties in both inpatient and outpatient settings. This article aims to analyze the teaching theories and methods observed during internal medicine residency training. An essential benefit of learning theories is the ability to articulate educational plans and objectives more precisely. Furthermore, integrating theory into practice strengthens improvement programs and facilitates their evaluation. [1] The following sections describe and analyze the educational process as experienced throughout the residency program from resident perspective.
Upon entering the program, residents undergo two to four weeks of shadowing and orientation, during which they familiarize themselves with the hospital system and are assessed on their attitude, professionalism, and eagerness to learn. Subsequently, residents are assigned to progressively responsible roles within general medical teams, initially under peer and senior supervision. Learning occurs formally and informally, through observation and supervised participation, fostering a community of practice among colleagues. This social model of learning allows residents to progress from "legitimate peripheral participation" to full integration into the community, as described by Lave and Wenger. [2]
Throughout training, Bandura’s social learning theory [3] is applied: initially through attention to the behaviors of seniors, followed by retention of observed practices, reproduction of these behaviors in similar contexts, and reinforcement through feedback. [4] To manage the high cognitive load associated with clinical practice, residents are initially assigned simpler tasks, which progressively increase in complexity. [5] Learning theories such as behaviorism, cognitivism, constructivism, humanism, and connectivism interweave during residency. Behaviorism is observed when external stimuli shape resident behavior, while cognitivism highlights internal thought processes. Constructivism underscores the learning derived from experience and reflection, humanism emphasizes autonomy and personal growth, and connectivism focuses on collaborative learning environments. [6]
Reflective Practices
Reflective practice is crucial for the development of mature physicians, acknowledging that "diseases do not read textbooks." From the outset, residents are encouraged to apply their knowledge and clinical judgment with appropriate faculty supervision. Kolb’s experiential learning cycle is evident throughout the training journey. In the first year, residents accumulate "concrete experiences" across a range of clinical scenarios. As they advance, they begin to reflect on these experiences, integrating them with theoretical knowledge acquired through readings and educational sessions. This reflection leads to "abstract conceptualization," wherein residents formulate new understandings, ultimately culminating in "active experimentation" — the application of insights into clinical practice (7). By the fourth year, residents are expected to act independently under indirect supervision, making critical decisions such as admissions and discharges, and leading ward rounds, thereby solidifying their clinical reasoning skills in preparation for independent consultancy. However, variations in the application of reflective practice are observed among trainees. Some remain confined to repetitive clinical tasks without significant reflection. Addressing this requires structured initiatives to promote reflective practices among both residents and faculty, including dedicated reflective activities, to maximize learning from experience (8).
Role of Consultants
During ward rounds, consultants function as team leaders, guiding safe, evidence-based patient care while simultaneously facilitating resident education. HMC’s multicultural environment, with consultants from diverse scientific and cultural backgrounds, enriches trainees' clinical exposure. Teaching strategies adapted from Cantillon (9) are employed: consultants encourage active participation, stimulate prior knowledge, engage residents with case-based questions, and conduct bedside examinations.
Residents are tasked with presenting cases comprehensively and receiving continuous real-time feedback, promoting deeper clinical understanding. Despite challenges such as heavy workloads and time constraints, efforts are made to preserve the educational value of ward rounds through awareness programs and the adoption of teaching models like the "One-Minute Preceptor" and "Flipped Classroom" (10).
Consultants also play an essential role in small-group educational activities, including pre-call presentations, PICOs (Patient/Problem, Intervention, Comparison, Outcome), and bedside teaching sessions. Although bedside teaching is vital for honing diagnostic skills, its prevalence is declining due to clinical pressures and technological reliance (11). To counter this trend, initiatives such as MINI-CEX evaluations, registrar-led teaching sessions, and exam preparation activities have been introduced.
Feedback and Evaluation
Feedback is a cornerstone of resident development, though a standardized evidence-based feedback model remains elusive (12). At HMC, residents and educators set specific goals at the start of each training block, with structured mid-block and end-of-block evaluations supplemented by formative online assessments (13). These evaluations serve to motivate residents, highlighting areas for clinical and professional growth. It help to assess and monitor the six ACGME-I competencies which are Patient Care, Medical Knowledge, Practice Based Learning and Improvement, Systems Based Practice, Professionalism and Interpersonal Skills Communication.
Challenges such as time constraints and varying degrees of motivation among residents and consultants can impact the effectiveness of feedback tools. Nevertheless, fostering a culture of effective feedback, including the use of web-based tools, remains a program priority (14).
A 360-degree evaluation system is also implemented, collecting feedback from a wide range of sources including the resident himself, peers, nurses, pharmacists and faculty consultants. This comprehensive approach assesses communication, professionalism, and teamwork skills (15). Its usually conducted once or twice yearly and monitored by the program.
Additionally, the MINI-CEX tool, requiring at least six evaluations annually, enhances learning within clinical rotations when utilized effectively (16). Other feedback mechanisms include Chart-Stimulated Recall (CSR) sessions, where faculty and residents engage in detailed reviews of patient cases to assess clinical reasoning and documentation. It’s usually done face to face meeting between faculty and the resident with thorough review of the documents. This will enhance the reflective practices. CSR assess clinical competence using a clinician's documented patient encounter as the starting point for assessment of clinical reasoning and clinical documentation. Patient records for CSR are usually selected by faculty providing assessment but may also be selected by the learner. CSR involve asking the trainee to externalize his or her thought processes—to elicit diagnostic reasoning, decision-making, and related decisions such as use of resources or communicating with patients, families, or other members of the health care team. (17) Summative feedback is conducted twice yearly to judge if the residents will move to next academic year.
Educational Activities
Residents engage in a broad spectrum of educational activities, including daily case-based discussions, weekly lectures on research and quality improvement, emergency management, diagnostic interpretation, grand rounds, morbidity and mortality meetings, journal clubs, and policy updates. These sessions enhance medical knowledge and foster teaching and presentation skills, as many activities are resident-led.
Board preparation is also emphasized, with dedicated didactic sessions focusing on MCQs spanning internal medicine subspecialties. Clinical exam preparation is supported through intensified bedside teaching by consultants and structured sessions led by senior registrars. Additionally, annual mock examinations simulate the Arab Board clinical assessment format, providing residents with valuable practical experience.
Procedure Teaching
Skill acquisition in essential procedures such as urinary catheterization, lumbar puncture, and abdominal paracentesis follows the "observe one, perform one, teach one" model. Initially, residents observe procedures conducted by experienced practitioners, followed by supervised practice, and eventually, independent performance after demonstrating competence. Upon proficiency, residents are issued competency cards authorizing unsupervised or indirectly supervised practice.
To further enhance procedural safety and proficiency, simulation-based training has been integrated into the curriculum, aligning with best practices recommended by Vozenilek et al. (18). This approach ensures that residents acquire necessary procedural skills within a controlled, patient-safe environment.
Quality and Research
HMC’s Internal Medicine Residency Program strongly promotes resident engagement in quality improvement and research initiatives. Twice-monthly lectures in addition to quality workshops form part of the program’s structured support. Active participation in quality and research projects not only addresses healthcare gaps but also fosters patient safety, system efficiency, and professional development (19).
By graduation, each resident must complete at least one quality project and one research activity. Notably, the number of resident-led publications has demonstrated continuous growth, from 90 publications in 2019–2020, to 175 in 2020–2021, and reaching 195 publications during the 2021–2022 academic year.
Teaching and Patient Care
The medical teams at Hamad General Hospital exemplify a "community of practice," collaborating toward the shared objective of delivering optimal, evidence-based, patient-centered care. Clinical rounds routinely incorporate detailed discussions supported by current evidence, emphasizing teamwork, collaboration, quality improvement, and best practices.
Numerous studies have linked the practice of evidence-based medicine with improved clinical outcomes, reduced mortality, and shorter hospital stays (20), affirming the dual focus on teaching and patient care embedded within the program. Managing the patient in an environment of teaching has been linked to a shorter hospital stay and decreased mortality. (21)
Courses and Workshops
The residency program offers a broad array of supplementary courses and workshops aimed at enhancing resident competencies. Core offerings include research methodology courses, quality improvement workshops, professionalism courses, and communication skills workshops. Additionally, residents may attend specialty-specific workshops across internal medicine disciplines, allowing for tailored skill development according to individual interests.
Examinations
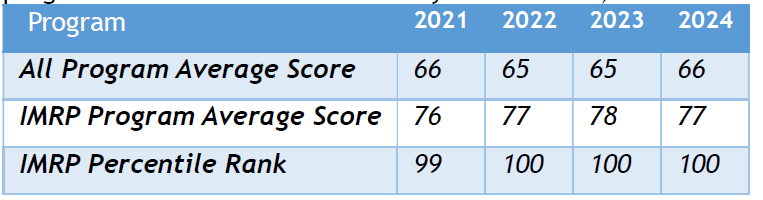
Graduates of the Internal Medicine Residency Program at HMC qualify for both the Arab Board and Qatari Board certifications. Moreover, as an ACGME-I accredited program, rigorous evaluation mechanisms are in place to ensure educational excellence. One key assessment tool is the annual In-Training Examination (ITE), administered by the American College of Physicians. This web-based, self-assessment exam mirrors the American Board of Internal Medicine certification examination, providing an international benchmark for resident progress. HMC residents have consistently performed exceptionally well, achieving percentile ranks among the top 1% of all ACGME-I programs globally in 2021. (22)
Table 1: Hamad Medical Corporation Internal Medicine Residency Program (IMRP) performance compared to all ACGME-I accredited programs (based on data from 615 programs with five or more second-year residents).
CONCLUSION
The Internal Medicine Residency Program at Hamad Medical Corporation provides a comprehensive educational environment enriched by a diverse array of teaching methodologies, multicultural consultant experiences, and robust educational activities. Emphasizing reflective practice, evidence-based patient care, research engagement, and continuous feedback, the program effectively prepares residents for independent practice and lifelong learning, ensuring the delivery of safe, effective, and innovative healthcare.
ACKNOWLEDGEMENT
Special thanks are extended to Dr. Dabia Al Mohannadi (Program Director of IMRP) and Dr. Hisham El Hiday (Chief Fellow of IMRP) for their valuable assistance in reviewing this article. Gratitude is also extended to Seeya Yousif and Adla Alshehabi (Secretaries in the IMRP Office) for providing essential data regarding research output and examination performance.
SOURCE OF FUNDING
None.
CONFLICT OF INTEREST
None.
References
- Davidoff F, Dixon-Woods M, Leviton L, Michie S. Demystifying theory and its use in improvement. BMJ quality & safety. 2015 Mar 1;24(3):228-38.
- Cruess RL, Cruess SR, Steinert Y. Medicine as a community of practice: implications for medical education. Academic Medicine. 2018 Feb 1;93(2):185-91.
- Bandura A, Walters RH. Social learning theory. Englewood Cliffs, NJ: Prentice hall; 1977 Mar.
- Horsburgh J, Ippolito K. A skill to be worked at: using social learning theory to explore the process of learning from role models in clinical settings. BMC medical education. 2018 Dec;18:1-8.
- Young JQ, Van Merrienboer J, Durning S, Ten Cate O. Cognitive load theory: implications for medical education: AMEE Guide No. 86. Medical teacher. 2014 May 1;36(5):371-84.
- Shaughnessy AF, Erlich DR. The science of education: using learning theory to solve teaching problems in medical education. Education for Primary Care. 2022 Jul 4;33(4):194-8.
- Kolb DA. Experience as the source of learning and development. Upper Sadle River: Prentice Hall. 1984.
- Sternlieb Jeffrey L. A guide to introducing and integrating reflective practices in medical education. The International Journal of Psychiatry in Medicine. 2015 Jan;49(1):95-105.
- Cantillon P, Wood DF, Yardley S, editors. ABC of Learning and Teaching in Medicine. John Wiley & Sons; 2017 Sep 25.
- Andrew C. What is the educational value of ward rounds? A learner and teacher perspective. Clinical Medicine. 2011 Dec 1;11(6):558-62.
- Peters M, Ten Cate O. Bedside teaching in medical education: a literature review. Perspectives on medical education. 2014 Apr;3:76-88.
- Bing-You R, Hayes V, Varaklis K, Trowbridge R, Kemp H, McKelvy D. Feedback for learners in medical education: what is known? A scoping review. Academic Medicine. 2017 Sep 1;92(9):1346-54.
- Weurlander M, Söderberg M, Scheja M, Hult H, Wernerson A. Exploring formative assessment as a tool for learning: students’ experiences of different methods of formative assessment. Assessment & Evaluation in Higher Education. 2012 Sep 1;37(6):747-60.
- Bindal T, Wall D, Goodyear HM. Trainee doctors’ views on workplace-based assessments: are they just a tick box exercise?. Medical teacher. 2011 Nov 1;33(11):919-27.
- -Tariq, M., Boulet, J., Motiwala, A., Sajjad, N., & Ali, S. K. (2014). A 360-degree evaluation of the communication and interpersonal skills of medicine resident physicians in Pakistan. Education for Health, 27(3), 269-276.
- HAUER KE. Enhancing feedback to students using the mini-CEX (Clinical Evaluation Exercise). Academic Medicine. 2000 May 1;75(5):524.
- Philibert I. Using chart review and chart-stimulated recall for resident assessment. Journal of graduate medical education. 2018 Feb 1;10(1):95-6.
- Vozenilek J, Huff JS, Reznek M, Gordon JA. See one, do one, teach one: advanced technology in medical education. Academic emergency medicine. 2004 Nov;11(11):1149-54.
- Backhouse A, Ogunlayi F. Quality improvement into practice. Bmj. 2020 Mar 31;368.
- Connor L, Dean J, McNett M, Tydings DM, Shrout A, Gorsuch PF, Hole A, Moore L, Brown R, Melnyk BM, Gallagher‐Ford L. Evidence‐based practice improves patient outcomes and healthcare system return on investment: Findings from a scoping review. Worldviews on Evidence‐Based Nursing. 2023 Feb;20(1):6-15.
- Rosenthal GE, Harper DL, Quinn LM, Cooper GS. Severity-adjusted mortality and length of stay in teaching and nonteaching hospitals: results of a regional study. Jama. 1997 Aug 13;278(6):485-90.
- HMC Internal Medicine Residency Program achieves exceptional score of 99 percentile (2021) Hamad Medical Corporation. Available at: http://www.hamad.qa/en/news/2021/november/pages/hmc-internal-medicine-residency-program-achieves-exceptional-score-of-99-percentile.aspx.
