Full HTML
Transverse testicular ectopia with persistent mullerian duct syndrome: A case series
Rupesh Keshri1, Digamber Chaubey2, Chandrakant Maurya1, Vivek Kumar1, Sourabh Chandrabhushan Sharma1, Sandip Kumar Rahul1
Author Affiliation
1Deprtment of Paediatric Surgery, All India Institute of Medical Sceiences, Deoghar, Jharkhand, India
2All India Institute of Medical Sciences (AIIMS), Patna, Bihar, India
Abstract
Transverse testicular ectopia with persistent mullerian structures is seldom seen. Although treatment for this condition is well defined, it is very important to suspect persistent mullerian duct syndrome in cases where both testes are found on the same side. We discuss three unusual cases which presented with non- palpable undescended testis on one side and a hernia with two gonads and persistent mullerian structures on the other side.
DOI: 10.18231/j.yjom.2024.031
Keywords: Transverse testicular ectopia, Persistent mullerian duct syndrome, Undescended testis
Pages: 265-268
View: 6
Download: 6
DOI URL: http://doi.org/10.18231/j.yjom.2024.031
Publish Date: 15-12-2024
Full Text
Transverse Testicular ectopia (TTE) is an unusual condition of ectopic testis where both testes are in the same inguinal canal. TTE was first described by Von Lenhossek et al. in 1886. 1 Persistent Mullerian Duct syndrome (PMDS) manifests in phenotypic males as the persistence of mullerian remnants like the uterus, fallopian tubes, cervix, upper third of the vagina, and the broad ligaments. 2 These occur in addition to unilateral or bilateral undescended testes. A subset of PMDS, in which the contralateral testis and fallopian tube are also found on the side of the ipsilateral inguinal hernia, may also occur. 3 This anatomy of PMDS associated with TTE represents only 10% of all PMDS cases. Although Jordan et al. first reported a case with both TTE and PMDS in 18954, fewer than 300 such cases have been reported in the literature to date. 5
Of the three types of TTE described in the literature, around 30% of cases are associated with PMDS. 6 Being rare with a unique anatomy, it is important that the operating surgeon is aware of this condition and its management. We present the clinical features and management of three such cases managed in our department in the last five years.
Case 1.
A 16-year-old boy presented to the outpatient’s clinic with a history of swelling in the left inguinal region and an empty scrotum on the right side. No other symptoms were present. On examination, he had attained puberty and had a muscular appearance, he had facial hair; no gonad was palpable on the right side and the right scrotum was hypoplastic. There was an expansile, non-tender, reducible swelling on the left side with ipsilateral testis palpable in the inguinal region. The rest of the examination was normal. Routine blood and urine investigation reports were normal. Sonography revealed no gonad on the right side and left testis in the left inguinal canal with a hernia. However, a large mass was evident near the deep ring.
During elective surgery for hernia on the left side through the left inguinal incision, the hernial sac was seen to contain two testes (one healthy and one atrophic) along with the uterus and fallopian tubes. No ovary was present. An intraoperative diagnosis of PMDS with TTE was made. The patient’s parents were informed about the findings and the uterus with its appendages was removed. Excised tissues were sent for histopathological examination (HPE). Mobilized right testis was brought down on the right side and orchidopexy was done on both sides. The patient’s parents were informed about the findings and the uterus with its appendages was removed. Excised tissues were sent for histopathological examination (HPE). Mobilized right testis was brought down on the right side and orchidopexy was done on both sides. The patient had an uneventful post-operative period. HPE report confirmed the Uterus with its appendages and testis in the surgical specimen. No features of malignancy were present.
Case 2.
A six-year-old boy presented with glandular hypospadias and right non-palpable undescended testis for which laparoscopy was done after routine investigations. Intraoperatively, the right testis was found near the opposite (left) deep ring with atretic uterus and fallopian tubes. The left testis was descended and there was no hernia on the left side in this case. The atretic uterus was divided and the testis was mobilized and finally fixed in the right hemiscrotum. In this case, complete excision of the atretic mullerian remnants was not done and only division with mobilization of the undescended testis to enable orchiopexy sufficed.
Case 3.
A 14-year-old boy presented with left non-palpable undescended testis and right inguinal hernia. During right inguinal exploration, he had an anatomy like the first case but on the opposite side. Uterus with fallopian tubes was present and both the testis were found on the right side. Following hysterectomy and mobilization of both testes, bilateral trans-septal orchiopexy was performed (Figure 1). (Figure 2 a & 2b) summarizes the anatomy of the case and the surgical procedure for its correction. (Table 1) summarizes the clinical findings of the three cases.
.png)
Figure 1: A & B. Transverse Testicular Ectopia with Persistent Mullerian Duct syndrome
.png)
Figure 2: A: Anatomical diagram of case 2 B : Pre & post- operative Diagram of case 3
Table 1: Summary of the three cases of transverse testicular ectopia and persistentmullerian duct syndrome
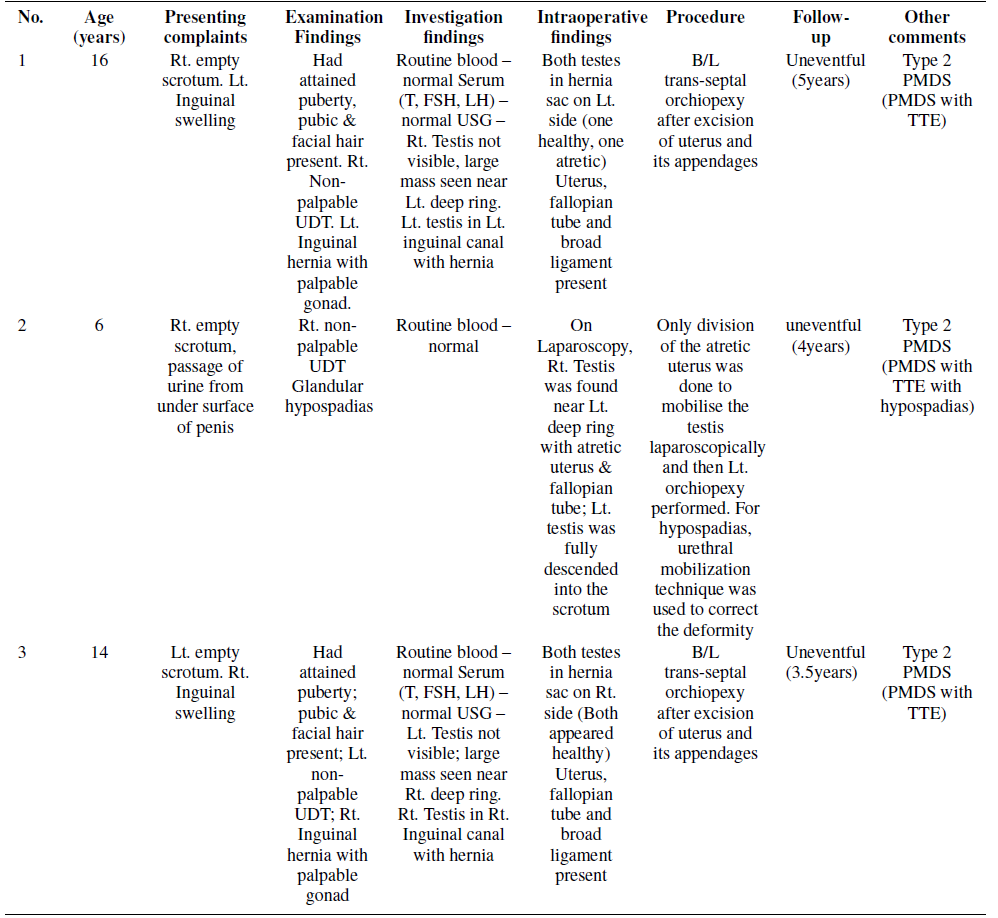
Rt.- Right; Lt. – Left; T – Testosterone; FSH – Follicle stimulating hormone; LH – Luteinizing hormone; USG – Ultrasound; UDT – Undescended testis; B/L – Bilateral; PMDS – Persistent mullerian duct syndrome; TTE – Transverse testicular ectopia
Follow-up was uneventful in all three cases.
Utriculus Prostaticus is the only mullerian remnant in a normal male. If other mullerian derivatives are conspicuous in a phenotypic male, PMDS is suspected. Not only a mutation in the gene for Mullerian inhibiting substance (MIS) but also a defect in its receptor can cause PMDS. 7,8 This results in a variable degree of persistence of mullerian remnants. MIS belongs to the transforming growth factor (TGF-β) family and its secretion is free Utriculus Prostaticus is the only mullerian remnant in a normal male. If other mullerian derivatives are conspicuous in a phenotypic male, PMDS is suspected. Not only a mutation in the gene for Mullerian inhibiting substance (MIS) but also a defect in its receptor can cause PMDS. 7,8 This results in a variable degree of persistence of mullerian remnants. MIS belongs to the transforming growth factor (TGF-β) family and its secretion is free of Pituitary control. 8 It is the Sertoli cells which secrete MIS that causes regression of Mullerian ducts between 8 -10 weeks of foetal life. As against this, Leydig cells secrete Testosterone which preserves the Wolffian ducts responsible for the normal development of epididymis, vas deferens, and seminal vesicles. In PMDS, the androgen- dependent structures like penis, scrotum, epididymis, Vas deferens, seminal vesicles, and prostate usually show normal development. Three anatomic variants of PMDS [Female type (bilateral cryptorchidism with testis embedded in lax broad ligaments in ovarian position with respect to the uterus), Male type (Hernia uteri inguinalis), and TTE (as in this case series)] have been described in literature. 3 Of these, PMDS with TTE is the least common variant.
The presentation of PMDS patients is usually as a male with unilateral or bilateral cryptorchidism and inguinal hernia with normal male external genitalia. Patients may present at variable ages like the usual cases of cryptorchidism. This is clear in our series where all three children were late presenters. Cases of PMDS have 46XY karyotypes. In case both the testes have not become atrophic serum Testosterone levels are usually normal; as are the levels of Follicle-stimulating hormone (FSH) and Luteinizing hormone (LH).
The surgical management of mullerian remnants in cases of PMDS is debatable. The blood supply to the PMDS testis is usually through internal spermatic and deferential arteries, which are closely related to the testis. So, during the excision of these mullerian remnants, the vascular supply to the testis can be jeopardized and so one must be very careful while mobilizing such testis. The mobilized testis
is brought down to the scrotum and fixed there. Trans- septal orchiopexy (Ombredanne technique) is helpful in such cases if the vasal and vascular length is adequate for both testes. 9 In two cases of this series, where open exploration and mobilization were done, orchiopexy was done using this technique. If the length of the vas or vessels is not optimum or if there are additional anomalies like fused vas deferens, the opposite testis may not reach its corresponding scrotal sac. In such cases, both the testes may require fixation on the same shorter side. Dhua et al. reported a case of TTE with PMDS and a blind-ending Vas deferens. 10 Laparoscopic excision of mullerian remnants is easier due to direct visualization of PMDS. Mobilized testes in such cases can be fixed into the scrotum using a shorter course laparoscopically as done in one of our cases.
The undescended testis in such cases has been described to be ‘-at risk’ for malignancy and should be kept in follow- up. 11,12 Barki et al. reported a case of mixed germ cell tumor, seminoma in such a case in a 48-year-old man. 12 By contrast, Shinmura et al reported clear cell adenocarcinoma of the mullerian duct in a case of PMDS. 13 In their seminal work on PMDS cases in which a historical review of PMDS cases was done along with their own cases, Farikullah et al. identified eleven cases of malignancy of mullerian remnants and therefore emphasized the excision of all mullerian remnants along with orchiopexy in such cases. 14 So, it is not only the undescended testes but also the mullerian remnants which are at risk of malignancy in such cases.
Fertility impairment has been reported in PMDS cases with TTE in large series; 15 but references to fertility and paternity can also be found in the literature. 15,16 Due to the rarity of the condition, long-term follow-up of these cases is necessary to have conclusive evidence regarding their fertility and malignancy risks.
Conclusion
TTE with PMDS represents a unique subset associated with challenges in management and long-term fertility and malignancy issues. Awareness about the unique anatomy of these cases and suspicion of their co-existence when confronting TTE guides appropriate management and successful outcomes.
Patient Consent and Ethical Approval
Consent was taken from the parents of the patients and approval was taken from the ethics committee to use retrospective data of the patients.
Conflict of Interest
None.
Source of Support
None.
References
- Lenhossek V. Ectopia testis transversa. Anat Anz. 1886;1:376.
- Agrawal AS, Kataria R. Persistent Müllerian Duct Syndrome (PMDS): a Rare Anomaly the General Surgeon Must Know About. Indian J Surg. 2015;77(3):217–38.
- Hutson JM, Chow CW, Ng WT. Persistent mullerian duct syndrome with transverse testicular ectopia. Pediatr Surg Int. 1987;2:191–5.
- Berkmen F. Persistent müllerian duct syndrome with or without testicular ectopia and testicular tumours. Br J Urol. 1997;79(1):122–6.
- Chua I, Samnakay N. Persistent Müllerian Duct Syndrome: Understanding the Challenges. Case Rep Urol. 2022;2022:2643833.
- Gauderer MW, Grisoni ER, Stellato TA, Ponsky JL, Izant RJ. Jr Transverse testicular ectopia. J Pediatr Surg. 1982;17(1):1–2.
- Hoshiya M, Christian BP, Cromie WJ. Persistent müllerian duct syndrome caused by both a 27-bp deletion and a novel splice mutation in the MIS type II receptor gene. Birth Defects Res A Clin Mol Teratol. 2003;67(10):868–74.
- Josso N, Belville C, Clemente ND, Picard JY. AMH and AMH receptor defects in persistent mullerian duct syndrome. Hum Reprod Update. 2005;11(4):351–6.
- Divarcı E, Ulman I, Avanoglu A. Transverse testicular ectopia treated by transseptal contralateral transposition: case report. Eur J Pediatr Surg. 2011;21(3):191–3.
- Dhua AK, Varshney A, Bhatnagar V. Transverse testicular ectopia with a blind ending vas deferens. Indian J Urol. 2016;32(4):317–9.
- Modi J, Modi D, Bachani L. Acute urinary retention caused by seminoma in a case of persistent Mullerian duct syndrome. Indian J Pathol Microbiol. 2015;58(1):83–8.
- Barki D, Manayath N, Vatsa BS, Venkatanarasimhan NS, Vishnuvardhana GV, Achar S, et al. Testicular masquerade’: a case report of testicular malignancy with persistent Müllerian duct syndrome and transverse testicular ectopia. Ann R Coll Surg Engl. 2024;106(5):466–70.
- Shinmura Y, Yokoi T, Tsutsui Y. A case of clear cell adenocarcinoma of the müllerian duct in persistent müllerian duct syndrome: the first reported case. Am J Surg Pathol. 2002;26(9):1231–5.
- Farikullah J, Ehtisham S, Nappo S, Patel L, Hennayake S. Persistent Müllerian duct syndrome: lessons learned from managing a series of eight patients over a 10-year period and review of literature regarding malignant risk from the Müllerian remnants. BJU Int. 2012;110(11):1084–9.
- Picard JY, Cate RL, Racine C, Josso N. The persistent Müllerian duct syndrome: an update based upon a personal experience of 157 cases. Sexual Dev. 2017;11(3):109–34.
- Farag TI. Familial persistent Müllerian duct syndrome in Kuwait and neighboring populations. American Journal of Medical Genetics. 1993;47:432–436.
