Full HTML
A cute pancreatitis following laparoscopic sleeve gastrectomy: A case report and literature review
Abdulhaleem Elhiday1
Author Affiliation
1Senior Consultant, Department of Medicine, Hamad General Hospital, Doha, Qatar
Abstract
Recent reports showed an association between bariatric surgery and the development of acute pancreatitis. This report presents a case of acute pancreatitis following a laparoscopic sleeve gastrectomy (LSG) in a 24-year-old Indian female patient, who presented to the Emergency Department at Hamad General Hospital, Qatar, with severe epigastric pain and persistent vomiting 13 days after LSG. She was diagnosed with acute pancreatitis based on a high level of lipase greater than three times the upper limit of normal, and a computed tomography scan of the abdomen, which was consistent with acute pancreatitis. The patient was treated conservatively with a significant improvement in her symptoms and laboratory tests throughout her admission and consequently was discharged.
DOI: 10.32677/yjm.v1i1.3274
Keywords: : Acute pancreatitis, Computed tomography, Lipase, Sleeve gastrectomy
Pages: 43-45
View: 3
Download: 10
DOI URL: https://doi.org/10.32677/yjm.v1i1.3274
Publish Date: 27-03-2025
Full Text
Laparoscopic sleeve gastrectomy (LSG) is, at present, one of the most common surgical treatments for morbid obesity worldwide that effectively achieve significant weight loss with the improvement of obesity-related comorbidities [1]. Staple line leak, bleeding, peritonitis, abscess, and stricture constitute the major complications that have been reported after sleeve gastrectomy [2]. However, pancreatitis directly following bariatric surgery is a very uncommon complication. A literature review revealed very few cases of acute pancreatitis postbariatric surgery [3-6]. Here, we present a rare case of acute pancreatitis following LSG in the early post-operative period to increase the awareness of bariatric surgeons of the complications of this surgery.
CASE REPORT
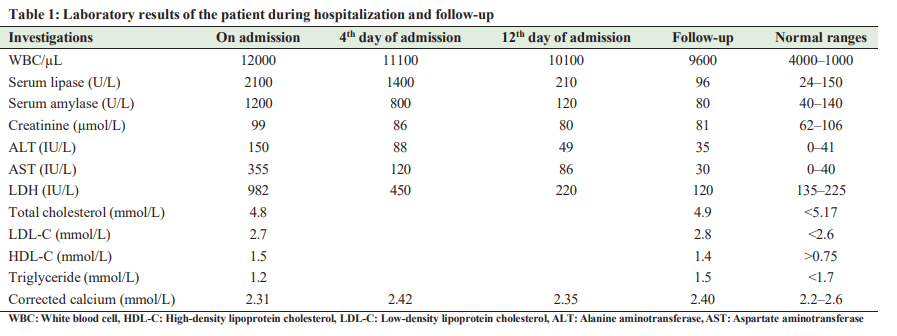
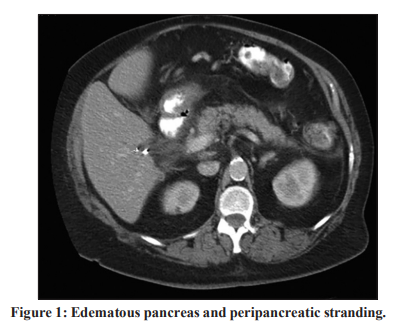
A 24-year-old Indian female patient presented to the Emergency Department at Hamad General Hospital, Qatar, with epigastric pain and persistent vomiting for the past 10 days. She denied loose stools, fever, constipation, melena, and dysuria. Her previous history was remarkable for morbid obesity (Body mass index = 41), for which she had undergone uncomplicated LSG 23 days ago in Jordan. Post-operative recovery was uneventful and she was discharged 5 days after surgery. However, on the 13th postoperative day, the patient developed epigastric pain and persistent vomiting, which brought the patient to the hospital. On physical examination, the patient looked sick, but she was conscious and well oriented. Blood pressure was 140/89 mm Hg, pulse 98/min, temperature 37.1°C, and respiratory rate was 16/min. Abdominal examination showed tenderness with the presence of a guarded abdomen. The rest of her examination was unremarkable.On admission, white blood cell counts were 12,000/mm, serum creatinine 99 mol/L, lactate dehydrogenase 982 IU/L, aspartate aminotransferase 355 IU/L, alanine aminotransferase 150 IU/l, serum amylase 1200 U/L, and serum lipase 2100 U/L. Her lipid profile showed total cholesterol of 4.8 mmol/L, triglyceride 1.2 mmol/L, high-densitylipoproteincholesterol1.5 mmol/L, and low-density lipoprotein cholesterol 2.7 mmol/L, and her corrected calcium was 2.31 mmol/l. Antinuclear antibody was negative, and immunoglobulin G level was within normal limits. Abdomen ultrasonography revealed no gallstones and no biliary tree dilatation. Abdominal computed tomography with contrast revealed edematous pancreas and peripancreatic stranding consistent with acute pancreatitis (Fig. 1), but there was no fluid collection or necrosis. The patient received conservative management with analgesics, antiemetics, intravenous fluid, and fasting. Moreover, the patient’s symptoms improved with significant clinical and laboratory improvement during her admission, and she was discharged after 12 days. During ambulatory follow-up, the patient presented with complete resolution of the symptoms and biochemical results (Table 1).
DISCUSSION
Gallstones and alcohol abuse are among the most common causes of acute pancreatitis, accounting for 80% of cases. Rare causes include drugs and toxins, metabolic disorders (hypertriglyceridemia, hypercalcemia, and others), connective tissue disorders, infections, and others [7]. Interestingly, recent case reports have been published of patients who developed acute pancreatitis after bariatric surgery with no identifiable causative risk factors. However, an important challenge in postbariatric surgery acute pancreatitis is establishing causality, because it is unclear whether this relation is causal or incidental. Therefore, this relationship will remain a subject of debate, as the cause-andeffect relationship has not yet been directly investigated. In this patient, it is hypothesized that acute pancreatitis is related to bariatric surgery, based on eliminating the main causes of acute pancreatitis, such as alcohol abuse and gallstones. In addition, normal triglyceride and immunoglobulin G levels ruled out hypertriglyceridemia and autoimmune pancreatitis as the cause of this clinical problem. Viral causes were not investigated as there was no history of viral prodromal symptoms before admission. he global incidence of acute pancreatitis postbariatric surgery, especially in the early period, is not well known as this event is rare. However, one study showed that the prevalence of this event was 1.04% [3]. To the best of our knowledge, this is the first case of acute pancreatitis in the early post-operative period following LSG reported in Qatar. The impact of bariatric surgery on the prevalence rate of acute pancreatitis is not clear. However, a recent study showed an increased rate of acute pancreatitis after versus before surgery in vertical sleeve gastrectomy (VSG) and Roux-en-Y gastric bypass (RYGB) groups compared to the control group. Moreover, compared with RYGB, VSG was associated with a markedly greater increase in the risk of post-operative acute pancreatitis [4]. Acute pancreatitis following LSG mostly resolves without complications in 80% of cases; however, in cases of severe pancreatitis (20%), complications can be life-threatening and lead to death in 3% of cases. The mechanism of increased acute pancreatitis after LSG surgery is not clear. However, Sarwal et al. [5] suggested that postbariatric acute pancreatitis is most likely caused by severe adhesion of peripancreatic tissue intraoperatively, compromised pancreatic microcirculation following gastrectomy, or edema and spasm of the major papilla. Hassan et al. found the following variables as potential risk factors for acute pancreatitis after VSG and RYGB: younger age, gallstones in the absence of cholecystectomy, prior cholecystectomy, female gender, and prolonged hospital stay (≥3 days) [4].
CONCLUSION
In conclusion, surgeons should maintain a high index of suspicion for acute pancreatitis as a short-term complication of LSG, given the increasing number of bariatric surgeries. Hence, acute pancreatitis should be considered in our list of differential diagnoses when seeing a patient presenting with epigastric pain after bariatric surgery to the Emergency Department. Could bariatric surgery be considered a new etiological risk factor for pancreatitis in the future?
AUTHOR CONTRIBUTION
The author was the treating physician, and he wrote the whole manuscript.
References
1.Pradarelli JC, Varban OA, Ghaferi AA, et al. Hospital variation in perioperative complications for laparoscopic sleeve gastrectomy in Michigan. Surgery 2016;159:1113-20.
2. Sarkhosh K, Birch DW, Sharma A, et al. Complications associated with laparoscopic sleeve gastrectomy for morbid obesity: A surgeon’s guide. Can J Surg 2013;56:347-52.
3. Kumaravel A, Zelisko A, Schauer P, et al. Acute pancreatitis in patients after bariatric surgery: Incidence, outcomes, and risk factors. Obes Surg 2014;24:2025-30.
4. Hussan H, Ugbarugba E, Porter K, et al. The type of bariatric surgery impacts the risk of acute pancreatitis: A nationwide study. Clin Transl Gastroenterol 2018;9:179.
5. Sarwal A, Khullar R, Sharma A, et al. Acute pancreatitis as an unusual early post-operative complication following laparoscopic sleeve gastrectomy. J Minim Access Surg 2018;14:164-7.
6. Baran KC, de Brauw M. Pancreatitis following bariatric surgery. BMC Surg 2019;19:77.
7. Khan FY, Sulaiman TO, Nair AP, et al. Coronavirus disease-19-associated acute pancreatitis: Report of three cases and review of case reports. Open Access Maced J Med Sci 2021;9:63-9.
