Full HTML
Pheochromocytoma in pregnancy: A case report and updated management review
Wajiha Gul1 , Khaled Ahmed Baagar2 , Hind Yousef Ahmed3 , Mohammed Bashir4
Author Affiliation
1Consultant, 2 Senior consultant, Department of Diabetes and Endocrine, Hamad Medical Corporation, Doha, Qatar
Abstract
Pheochromocytoma is a catecholamine-producing neuroendocrine tumor leading to hypertensive crises in untreated patients. Presentation in pregnancy can mimic gestational hypertension or pre-eclampsia. Physicians need to keep a high index of suspicion to have timely diagnosis and management of pheochromocytoma during pregnancy. We report a 27-year-old female who was diagnosed with pheochromocytoma at 18 weeks of gestation and she underwent laparoscopic adrenalectomy at 22 weeks of gestation with a good pregnancy outcome and with no recurrence over 8 years of follow-up.
DOI: 10.32677/yjm.v1i1.3334
Keywords: Pregnancy, Pheochromocytoma, Hypertension, Catecholamines.
Pages: 40-42
View: 5
Download: 13
DOI URL: https://doi.org/10.32677/yjm.v1i1.3334
Publish Date: 27-03-2025
Full Text
Pheochromocytoma in pregnancy: A case report and updated management review Wajiha Gul1 , Khaled Ahmed Baagar1 , Hind Yousef Ahmed1 , Mohammed Bashir2 1Consultant, 2 Senior consultant, Department of Diabetes and Endocrine, Hamad Medical Corporation, Doha, Qatar heochromocytoma is a rare catecholamine-producing neuroendocrine tumor of chromaffin cells, leading to hypertensive crises in untreated patients [1]. The prevalence of pheochromocytoma is variable, between 0.2 and 0.4% in hypertensive patients to 3–5% in patients with an incidental adrenal mass [2,3]. In pregnancy, the prevalence is between 1 in 15,000 and 1 in 54,000 pregnancies [4]. If left untreated, pheochromocytoma during pregnancy is associated with an increased risk of maternal and fetal morbidity and mortality [1,5]. Both reported that maternal and fetal mortalities are markedly improving from 48% to 1% and from 54% to 9% between 1971 and 2021; respectively, indicating improvement in diagnostic methods, medical treatment, obstetric care, and surgical and anesthesia expertise [6,7]. In this report, we present a case of pheochromocytoma detected and treated during pregnancy, with a brief literature review
CASE REPORT
A 27-year-old female, Gravida 4, Para 3, at 18 weeks of gestation, was admitted to obstetric care with a raised blood pressure of 210/100 mmHg. She had a 4-year history of hypertension. There was no family history of endocrine disorders or secondary hypertension. She did not have any workup for secondary causes of hypertension Her pre-pregnancy antihypertensive medications were nifedipine, hydrochlorothiazide, and hydralazine. During pregnancy, she was on methyldopa, nifedipine, and hydralazine, but her blood pressure readings were all elevated. She also reported intermittent symptoms of palpitations, sweating, and headaches. Physical examination was unremarkable except for an abdominal examination consistent with her gestational age. Because of her young age and elevated blood pressure, the workup for secondary causes of hypertension was carried out during her inpatient stay. Screening for vasculitis, lupus, primary aldosteronism, and overnight dexamethasone suppression test was negative. Laboratory tests revealed: Urea: 4.2 (2.5–6.7 mmol/L), creatinine: 55 (50–98 umol/L), sodium: 136 (135–145mmol/L), potassium 4 (3.6–5.1 mmol/L), and bicarbonate: 26 (22–29 mmol/L), 24-h urine vanillylmandelic acid 108.310 (0–33 umol/24 h), 24-h urine normetanephrine 25.052 (0–2.13 umol/24-h),24 h urine dopamine 3655 (0–3240 nmol/24 h), 24 h urine noradrenaline 10,719 (0–570 nmol/24 h), and 24-h urine adrenaline level was below the detection limit. MRI of the abdomen revealed a left adrenal mass 6 × 5.5 × 5 cm in diameter with features suggestive of pheochromocytoma. Because of her young age, RET (receptor tyrosine kinase) proto-oncogene mutation screening was done and it was negative. Her antihypertensive medications were adjusted to nifedipine 20 mg twice daily, methyldopa 500 mg 3 times daily, prazosin 1.5 mg twice daily, and a beta-blocker, labetalol, was added after 10 days. She underwent surgical resection of the adrenal mass at 22 weeks of gestation. Histopathology confirmed the diagnosis of pheochromocytoma. After the surgery, her anti-hypertension medications were tapered gradually. She delivered a healthy baby at 38 weeks through cesarean section (as she had previous three cesarean deliveries). Her blood pressure improved, and 8 years after her surgery, she is off antihypertensive medications and has no evidence of recurrence.
DISCUSSION
It has been assumed that catecholamine-secreting tumors occur rarely during pregnancy [4]. However, the condition has been described in an increasing number of reports in the past few years [8]. They could be sporadic or as a part of a familial syndrome such as MEN 2A (Multiple Endocrine Neoplasia), MEN 2B, or Von Hippel Lindau syndromes [1]. Bancos et al. reported a 66% genetic predisposition in a cohort of 144 pregnant females with pheochromocytoma [7]. Clinical presentation includes palpitations, headache, and diaphoresis, with or without hypertension [1]. Headache is present in around 90% of cases, while palpitations and diaphoresis are in around 5% of the cases [5]. Presentation during pregnancy closely resembles pregnancyinduced hypertension, essential hypertension, or pre-eclampsia [9]. Unfortunately, failure to diagnose pheochromocytoma has catastrophic implications on pregnancy outcomes [3,9]. Preeclampsia denotes new-onset hypertension after 20 weeks of gestation [9]. The presence of proteinuria, ankle edema, high serum uric acid, signs of hemolysis, increased liver enzymes, and low platelet count are in favor of pre-eclampsia [9]. Conversely, assessment for pheochromocytoma should be done in pregnant females with features of hereditary syndromes, orthostatic hypotension in a patient known to have hypertension, presentation of hypertension at <20 weeks of gestation, paroxysmal hypertension and headaches, and/or adrenergic attacks (episodic diaphoresis, palpitations, tremor, and pallor) [9]. More than 75% of the cases with pheochromocytoma are symptomatic during pregnancy, mostly later in pregnancy, as the tumor gets compressed by the gravid uterus resulting in catecholamine release [1,5]. Our patient was diagnosed early in the second trimester unlike most cases who were detected around the gestational age of 24 weeks [7]. Pregnancy does not affect biochemical testing of pheochromocytoma [9]. A 24 h urinary fractionated metanephrines and normetanephrines is the preferred test for screening and diagnosis of pheochromocytoma with 97% sensitivity and 69% specificity [10]. In addition, a combined measurement of both fractionated metanephrines and catecholamines in a 24 h urine sample has a sensitivity and specificity of 98% [10]. Plasma-free metanephrines have a sensitivity of almost 100% and a specificity of 85% [10]. Clinicians should be alert to the possibility of falsepositive values secondary to certain medications such as methyldopa, tricyclic antidepressants, labetalol, alcohol, and clonidine withdrawal; or certain medical conditions such as congestive heart failure, brain hemorrhage, and brain tumors [10]. On the other hand, false-negative results can be due to the use of immunoassays for diagnosis which are inaccurate and markedly underestimate plasma metanephrine and normetanephrine, compared with liquid chromatography with electrochemical or fluorometric detection (LC-ECD) and liquid chromatography with tandem mass spectrometry (LC-MS/MS). In addition, there is a possibility of false-negative results of plasma-free metanephrines withdrawn in a supine position, as reference intervals are often reported from blood samples taken from seated subjects [10]. Pregnancy impacts the choice of imaging modalities where MRI without contrast is the imaging modality of choice during pregnancy [9]. Furthermore, an ultrasound abdomen is helpful during the first trimester [1,5]. There is no consensus on the management of pheochromocytomas during pregnancy and available recommendations are from retrospective studies (Table 1) [7,9,10]. While laparoscopic surgical resection is the treatment of choice, medical treatment is critical to control the blood pressure and prepare the patients for surgery [9]. During the first trimester, medical treatment is preferred over surgery except in life-threatening situations due to the increased risk of miscarriage [1]. The first line of medical treatment is an alphablocker [1]. Prazosin and doxazocin are preferred during pregnancy due to their short half-life, while phenoxybenzamine has a longer half-life and binds irreversibly to alpha receptors [1]. Adequate hydration with intravenous fluids and a high salt diet is critical at all times, particularly during the perioperative period to reverse the catecholamine-induced blood volume contraction
Table 1: Management of pheochromocytoma diagnosed during pregnancy [7,9,10]
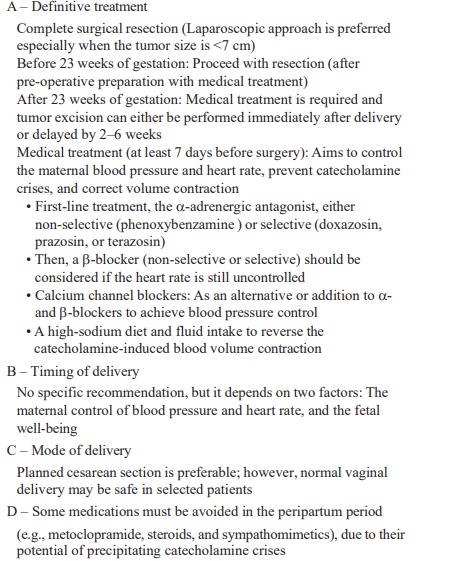
[10]. Within 7–14 days after starting alpha-blockers, betablockers (atenolol, propranolol) can be initiated to control the reflex tachycardia and reduce orthostatic hypotension [10]. Betablockers should be used in the lowest possible dose and for the minimum duration due to intrauterine growth retardation risk [1]. The second trimester is the appropriate time for surgical removal of the tumors [1]. During the third trimester, adrenalectomy is carried out preferably along with the delivery or immediately after it [1]. If surgical removal of the tumor is planned after delivery, the possibility of secretion of antihypertensive medications in breast milk should be considered [1,3,5]. Our patient underwent successful laparoscopic resection of pheochromocytoma in the second trimester after appropriate pre-operative preparation. Interestingly, it has been found no significant difference in pregnancy adverse outcomes between antepartum versus postpartum tumor excision [7,11]. Delivery should be carefully planned and the preferred mode of delivery is a cesarean section [9]. Vaginal delivery is not preferred in patients who did not undergo surgical removal of the tumor during pregnancy as uterine contractions can trigger catecholamine release leading to fatal complications in 31% of patients compared to 19% of patients who underwent cesarean delivery [12,13]. Although recent reports showed no difference in maternal or fetal mortality between vaginal delivery versus elective cesarean section, we should keep in mind that those two reports included patients who were mostly delivered by planned cesarean section, and the authors suggested that vaginal delivery may be safe in appropriately selected low-risk cases [7,11]. Our patient had a delivery through cesarean section because of her previous obstetric history (history of three cesarean deliveries). In the post-operative period, patients should have biochemical testing for metanephrines and normetanephrines in 2–4 weeks post-surgery to exclude persistent disease, then life-long annual screening for recurrent or metastatic disease [10]. In addition, genetic testing is essential as most patients in this age group have an autosomal dominant inheritance and are at an increased risk of other endocrine malignancies [10]. Fortunately, our patient had negative genetic testing.
CONCLUSION
Physicians need to keep a high index of suspicion to have a timely diagnosis and management of pheochromocytoma during pregnancy. Hypertension secondary to catecholamine release is potentially curable with surgical excision of the tumor. Appropriate management significantly improves both mortality and morbidity. Optimal outcomes need to have a multidisciplinary approach involving anesthetists, endocrine physicians, endocrine/ adrenal surgeons, and obstetricians.
AUTHORS’ CONTRIBUTION
Gul W contributed to writing the manuscript and reviewing the literature. Baagar KA contributed to developing the work idea composing and revising the manuscript. Ahmed HY contributed to composing and revising the manuscript. Bashir M contributed to composing and revising the manuscript. All authors read the manuscript and agree to its publication
References
1.Yulia A, Seetho IW, Ramineni A, et al. Pheochromocytoma in pregnancy: A review of the literature. Obstet Gynecol Cases Rev 2016;3:96.
2. Santos DR, Barbisan CC, Marcellini C, et al. Pheochromocytoma and pregnancy: A case report and review. J Bras Nefrol 2015;37:496-500.
3. Sarathi V, Lila AR, Bandgar TR, et al. Pheochromocytoma and pregnancy: A rare but dangerous combination. Endocr Pract 2010;16:300-9.
4. Ahlawat SK, Jain S, Kumari S, et al. Pheochromocytoma associated with pregnancy: Case report and review of the literature. Obstet Gynecol Surv 1999;54:728-37.
5. Oliva R, Angelos P, Kaplan E, et al. Pheochromocytoma in pregnancy: A case series and review. Hypertension 2010;55:600-6.
6. Schenker JG, Chowers I. Pheochromocytoma and pregnancy. Review of 89 cases. Obstet Gynecol Surv 1971;26:739-47.
7. Bancos I, Atkinson E, Eng C, et al. Maternal and fetal outcomes in phaeochromocytoma and pregnancy: A multicentre retrospective cohort study and systematic review of literature. Lancet Diabetes Endocrinol 2021;9:13-21.
8. Kurosawa S, Yamasaki H, Hasegawa W, et al. Intraoperative bleeding and drastic change in circulatory dynamics in a pregnant patient with metastatic pheochromocytoma: A case report. JA Clin Rep 2022;8:13.
9. Pacu I, Zygouropoulos N, Furau CG, et al. Pheochromocytoma as a rare hypertensive complication rarely associated with pregnancy: Diagnostic difficulties (Review). Exp Ther Med 2021;22:1345.
10. Lenders JW, Duh QY, Eisenhofer G, et al. Pheochromocytoma and paraganglioma: An endocrine society clinical practice guideline. J Clin Endocrinol Metab 2014;99:1915-42.
11. Langton K, Tufton N, Akker S, et al. Pregnancy and phaeochromocytoma/ paraganglioma: Clinical clues affecting diagnosis and outcome a systematic review. BJOG 2021;128:1264-72.
12. Junglee N, Harries SE, Davies N, et al. Pheochromocytoma in pregnancy: When is operative intervention indicated? J Womens Health (Larchmt) 2007;16:1362-5.
13. Kariya N, Nishi S, Hosono Y, et al. Cesarean section at 28 weeks’ gestation with resection of pheochromocytoma: Perioperative antihypertensive management. J Clin Anesth 2005;17:296-9.
