Full HTML
Gingival hypertrophy seen in perspective of typology and treatment trends, at patients treated with fixed orthodontic appliances
Ilma Robo1, Manola Kelmendi1, Saimir Heta2
Author Affiliation
1Dept. of Therapy, University of Medicine, Faculty of Dental Medicine, Tiranë, Albania
2Dept. of Pediatric Surgery, University Hospital Hospital, Tiranë, Albania
Abstract
Background: Gingival hypertrophy, the primary etiological factor, is the presence of bacterial plaque in the gingival sulcus, but if a fixed orthodontic appliance is placed in the affected teeth, the difficulty in achieving oral hygiene for these teeth increases, and it can even lead to "neglect" on the part of the patient. The clinical situation increases even more the possibility of gingival hypertrophy appearing.
Materials and Methods: The combination of the keywords gingival hypertophy, fixed orthodontic appliance, treatment, vertical index, horizontal index and bacterial plaque in Pubmed, applying them in combination between them, brought out about 31 articles for further analysis. From the selected articles, a total of 31 articles, after reading the abstracts of the full content of the article, 7 of them were outside the topic or scope of our study. 23 articles were used for further data processing.
Results: The tendency to find the incidence or prevalence of gingival hypertrophies in cases with orthodontic appliances is almost equal in the values of 29% and 24%. The lowest ratio is in the cases of case-report studies, which reaches the level of 5%. The reduction of gingival hypertrophy is indicated by the application of 40% chlorhexidine in gel form on the vestibular surface of already affected teeth, in the area of the maxillary molars on the vestibular surface.
Conclusion: Most of the articles try to find the cause of gingival hypertrophy to clinically compare patients without orthodontic appliances versus patients with orthodontic appliances, selecting patient samples with similarities in individual data conditions such as age for example. But seeing this trend, adolescent patients are selected more often, knowing also the close relationship that hormonal changes have with the appearance of gingival hypertrophies. This element can also lead to incorrect facts and figures.
Clinical Significance: The patient's periodontal status and his age are two other factors that attract the attention of studies at almost the same level of interest, leaving other factors such as the duration of orthodontic treatment and the socio-economic status of the patient at a lower level. Oral hygiene has an impact on the appearance of gingival hypertrophy in teeth with orthodontic appliances, this is expressed more in the area of the mandibular incisors than in the mandibular molars.
DOI: 10.18231/j.yjom.2024.012
Keywords: Orthodontic appliances, Fixed, Dental Plaque Index, Periodontal Indices, Gingival hypertrophy
Pages: 148-155
View: 2
Download: 6
DOI URL: http://doi.org/10.18231/j.yjom.2024.012
Publish Date: 11-09-2024
Full Text
The demand for orthodontic treatments is already presented in different age groups, it is understood with the necessary specific adaptations depending on the type of dentition and the condition in the oral cavity. 1–4 Fixed appliances are specifically indicated for permanent teeth without age limit and respecting this age group not only for pathologies such as gingival hypertrophy, but also for trauma from occlusion or even for implant treatment, the cooperation of the orthodontist with the periodontologist must be at a high level of professional understanding. The enlargement of the gingiva causes the movement of the gingival margin covering the tooth structure of the clinical crown, which automatically leads to the appearance of periodontal pathology under the classification of pseudopockets or intraosseous pockets when inflammation of the periodontal structures accompanied by incorrect tooth movement are combined together. 2,5–8 The literature supports the fact that gingival enlargement is the initial stimulus from the irritation of the materials used, mainly nickel allergy, but also from food fermentation products. 4,8–12
Orthodontic treatment has as primary the main role in the proper repositioning of the teeth, but followed by pink gingival margo. The gingival margin should fill the interdental spaces and be placed over the enamel-cementum junction. Fixed orthodontic treatments can cause soft tissues not only gingival hypertrophy, gingival intussusceptions but also gingival recessions, as if tooth inclinations are accompanied by immersion of the enamel-cement junction or its appearance in a visible supragingival position. 1,4,8,11 Data and clinical cases of gingival hypertrophy have been published in the literature even in cases of good oral hygiene, emphasizing the content of gingival fluid that indicates the presence of destructive enzymes of gingival collagen. Other authors focused on the occurrence of allergic reactions that may come from the nickel of which fixed orthodontic appliances are composed. The content of such material increased the indication to use nickelfree appliances in allergic patients. 11–14 Different authors have described hypertrophy as a linear invasion of the interproximal tissue with a mesial and distal direction and an intragingival depth of 1 mm. Gingival hypertrophy can range from a small surface crease to large defects that penetrate the alveolar bone. 1,7,14–17
Some studies have suggested that tilting of mandibular incisors is performed without jeopardizing periodontal health in patients treated with fixed orthodontic appliances if they have good oral hygiene. 1,3,6,8,11,14 Other studies showed that tilt movement with orthodontic appliances can be associated with a decrease in the width of keratinized tissue. These conclusions reached by these studies are consistent with other studies conducted some time ago, according to which labial tooth movement can reduce the height of the free gingiva that relieves gingival recession and can be associated with a decrease in buccolingual tissue thickness, while the lingual movement, unlike the buccal one, has the opposite effect. 17–23 Another element that is closely related to the treatment protocol with a fixed orthodontic appliance is the form of the periodontal biotype. In order to avoid problems with periodontal health, before starting orthodontic treatment, the health and thickness of the fixed gingiva should be assessed. 24,25
Orthodontic appliances apply biological forces, small and long-term forces, on the tooth-bearing studs and mainly on the bone and the periodontal ligament. These forces, being at the limits of biological forces, cause bone resorption or promote the creation of new bone on the surfaces where the pulling force is exerted and resorption on the dental surfaces where the compressive force is exerted. 26–29
The presence of periodontal pockets complicates the clinical picture. In cases where the periodontal pockets are below the level of the bone, then below the level of the alveolar ridge, depending on the anatomical shape, 1, 2 or 3 pages of the orthodontic apparatus indicates the application of force to the surface of the pocket, which means that areas of compression of the bone, or areas of its expansion will appear. 27–31 This is a clinical picture that is not included in our study. The clinical picture that affects is the fact of the presence of deep pockets caused by gingival hypertrophy, that is, in cases of gingival hypertrophy present before orthodontic intervention, or appearing after orthodontic intervention. Some studies have suggested that after periodontal surgical treatment, orthodontic treatment can have an effect on the morphology of bone defects, affect the healing of connective tissue and decrease the depth of pockets when they are present. 27–31 Some authors, after application of orthodontic forces, achieved clinical and radiological improvements. In the histological study, in the presence of good oral hygiene, new cementum formation and new collagen connection of the periodontal ligament can be obtained from orthodontic treatment.[27.29]
Guidance and eligibility criteria
The systematic review in question used the Prisma transparent reporting guidelines, which are designed to ensure a rigorous and transparent approach to conducting systematic reviews and meta-analyses. This study is of the review type with the primary purpose of finding data about the clinical evaluation of gingival hypertrophy, caused in patients treated with fixed orthodontic appliances in the oral cavity.
Information sources and search strategy
This information is collected from the selected articles in PubMed by combining the keywords applied for the search. The following query was used to screen the literature via Pubmed Advanced Search: (gingival enlargement OR orthodontic treatment OR fixed) AND (gingival overgrowth and index and orthodontic treatment). The selection of the Pubmed page as a source from which data will be collected from the articles to be selected, is a criterion that is predetermined by the authors, based on the evaluation that the authors themselves have for the safe and concrete information provided by this page of the published source. Articles in the field of medicine and also dentistry, since we are talking about such a topic in this article.
Selection and Data collection process
For the selection of the articles that will be included in the study, after being familiar with how it should be done, three reviewers (I.R., M.K. and R.K.) worked independently, who also independently applied the combination of keywords based on the way of their application. The collected data were further analyzed together to determine the final number of articles included in this article review.
Data items
12 articles were collected from the first phase of the search, while 19 articles were collected from the second combination of words. From the selected articles, a total of 31 articles, after reading the abstracts of the full content of the article, 7 of them were outside the topic or scope of our study. 23 articles were used for further data processing. After reading and processing the data collected from the published articles, they were analyzed and sorted and presented in the relevant tables expressing the purpose of this study.
Study selection If the situation is analyzed with an analytical eye for gingival hypertrophy caused by fixed orthodontic appliances, from 3949 articles, coming out of the combination with the keyword gingival enlargement and orthodontic treatment and fixed orthodontic appliance, reduced this number to almost 30 times less to the value of 126 articles. The second combination of the keywords gingival overgrowth and index and orthodontic treatment, was related to the orientation of the collection of articles related to the appearance of gingival hypertrophy caused by fixed orthodontic appliances, brought another group of 19 articles. found were also filtered for 10 years and reached the value of 23 articles for further analysis in this study, eliminating about 7 articles for further analysis. The inclusion criteria were all articles that specifically talk only about gingival hypertrophy in cases of patients with fixed orthodontic appliances, but hypertrophy defined only by the presence of bacterial plaque. Exclusion criteria concerned articles on allergy to fixed orthodontic appliance component materials and mouth breathing. At this stage, 23 articles were selected as part of the basic articles included in the study (Figure 1).
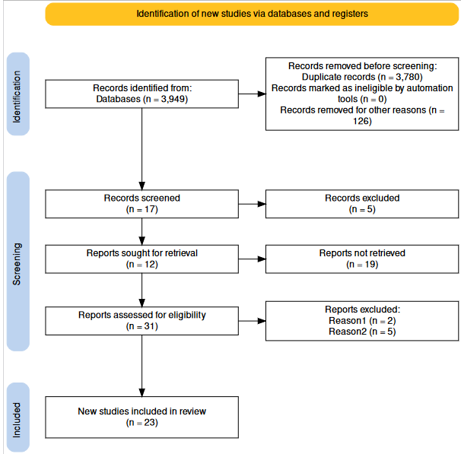
Figure 1: Flow diagram of the study protocol
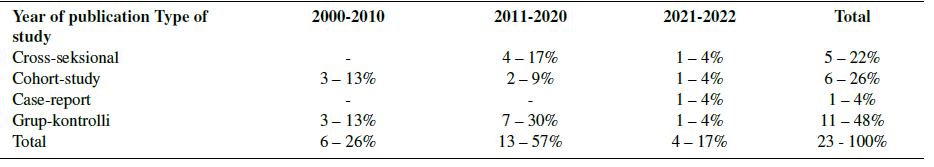
Based on the data collected from the electronic search in PubMed, the selected articles based on the characteristics evaluated by them, are grouped and presented in the following tables. Table 1 shows the distribution of articles based on their type, such as cross-sectional, cohort-study, case-report or randomized control trial. The type of article also shows the way and purpose for which the study was carried out, to find incidence to find prevalence or simply to show a clinical case and how this clinical case progressed after the intervention that was performed on the patient. This type of division also shows the tendency of studies on gingival hypertrophies caused by fixed orthodontic appliances.
Table 1: Distribution of articles based on the type of study performed presented in these selected articles, regarding gingival hypertrophy caused by fixed orthodontic appliances.
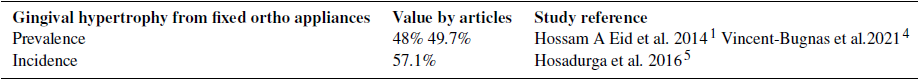
The studies of the selected articles were classified on the basis of the risk factor for the appearance of gingival hypertrophies. The data were presented in Table 2, while the Incidence and prevalence values of gingival hypertrophy caused by fixed orthodontic appliances were described in table 3.
Table 2: This table presents data on the risk factors of gingival hypertrophy, presented in the selected articles of the study, depending on the way of analysis expressed by the type of study applied
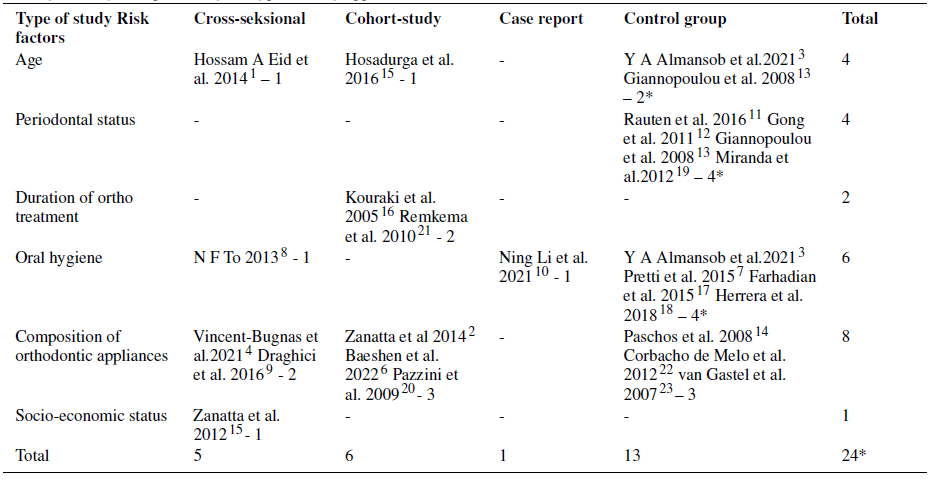
Table 3. Incidence and prevalence values of gingival hypertrophy caused by fixed orthodontic appliances.
The possible treatment of gingival hypertrophy is the application of different types of toothpastes, which significantly reduce plaque accumulation and gingival inflammation. Table 4 divides the studies according to angulation versus gingival hypertrophy caused by fixed orthodontic appliances. There are studies that aim at the diagnostic method of gingival hypertrophy, or the control of gingival hypertrophy at the microscopic level and the changes that the latter brings, or from the point of view of the treatment that can be performed.
Table 4: The collected articles were divided depending on the point of view and the interest that the pathology of gingival hypertrophy presents
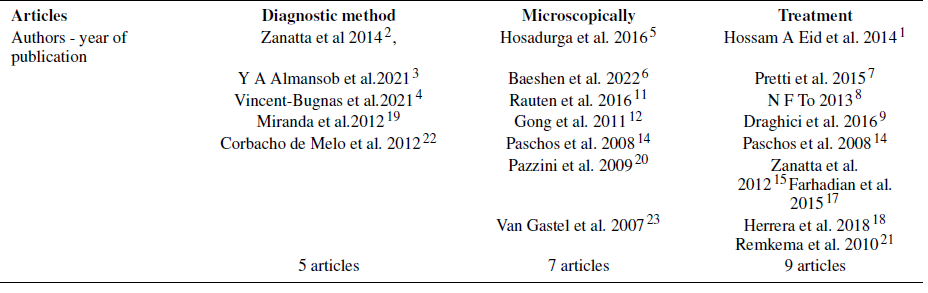
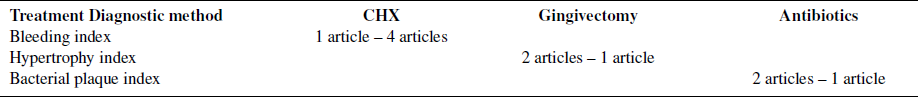
In table 5, the most specific data about the elements of table 4 are collected in relation to the authors’ agreement, for gingival hypertrophy caused by fixed orthodontic appliances. Table 6 lists the articles that microscopically assess gingival hypertrophy specifically according to the marker they identify in the article. Table 7, summarizes the articles depending on the treatment method of gingival hypertrophy caused by fixed orthodontic appliances. The combination of the data of table 5 and table 6 are expressed in figures in table 8.
Table 5: Diagnostic method of gingival hypertrophy caused by fixed orthodontic appliances, divided as positive result or negative result
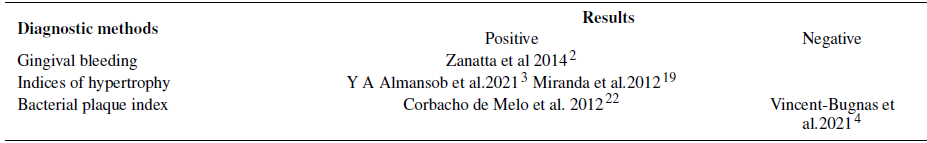
Table 6: Microscopic evaluation about changes that differ in gingival hypertrophy, presented specifically according to the article depending on which element or marker the study was carried out.
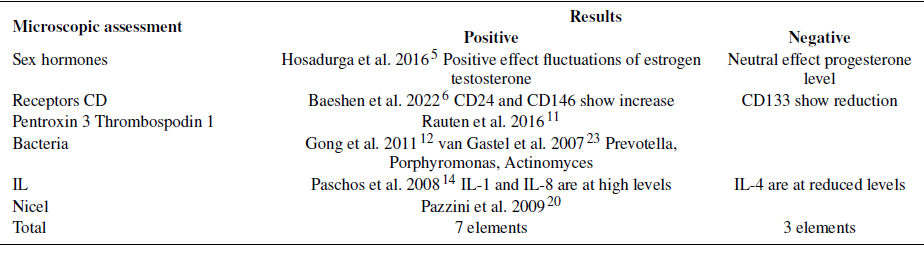
Table 7: This table summarizes the data on how to treat gingival hypertrophies caused by fixed orthodontic appliances.
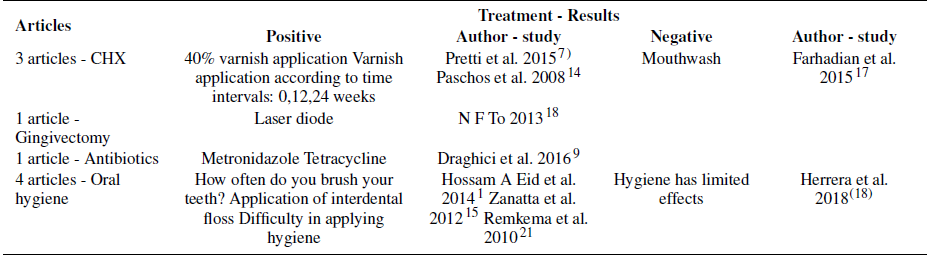
Table 8: Data on diagnostic methodology and treatment of gingival hypertrophies caused by fixed orthodontic appliances
Based on the data in table 1, the aim of the articles is to find the incidence and prevalence of gingival hypertrophy in cases of application of fixed orthodontic appliances. In order to find the causative factor, it seems that the tendency of the articles is higher, about 43% of articles oriented around studies with a control group. So, it is attempted to find the cause of gingival hypertrophy to clinically compare patients without orthodontic appliances versus patients with orthodontic appliances, selecting patient samples with similarities in individual data conditions such as age for example. Since we are dealing with the latter, adolescent patients are chosen more often, knowing also the close relationship that hormonal changes have with the appearance of gingival hypertrophies. The tendency to find the incidence or prevalence of gingival hypertrophies in cases with orthodontic appliances is almost in equal proportions, with values of 29% and 24%. The most reduced ratio is in cases of case-report studies at the level of 5%.
From the data in table 2, it is noted that among the most indicated factors as risk factors for the appearance of gingival hypertrophy after the placement of fixed orthodontic appliances is the metal component material, elastic, composite of the fixed orthodontic appliance applied to patients. The second factor in the sequence is the patient’s oral hygiene, assessed by the bacterial plaque index, which expresses the patient’s individual care for individual oral health. This shows the tendency of how gingival hypertrophy caused by the orthodontic apparatus is viewed, giving direction to the way of its treatment. The patient’s periodontal status and his age are two other factors that attract the attention of studies at almost the same level of interest, leaving other factors such as the duration of orthodontic treatment and the socio-economic status of the patient at a lower level. Oral hygiene has an impact on the appearance of gingival hypertrophy in teeth with orthodontic appliances, this is expressed more in the area of the mandibular incisors than in the mandibular molars.
Data supported by 2 studies. (2,3) If analyzed for oral hygiene based on a study (1) it is said that if brushing teeth 3 times a day, gingival hypertrophy will not appear, compared to brushing 2 times a day. days where the individuals who apply it present with gingival hypertrophy of the second degree, G2. But this data is rejected in another study, where it is stated that among the predisposing factors causing gingival hypertrophy in clinical cases with fixed orthodontic appliances in the oral cavity, in order to evaluate the regression of this pathology, it is directly related to metal brackets, the composition of and the duration of the treatment, or the time these nickel brackets have been in contact with the gingival tissues. (4) It is not the amount of bacterial plaque, but its quality that directly affects the appearance of gingival hypertrophy. But in cases where populations of the same age are compared, mainly adolescents with almost the same bacterial plaque index, it is noted that the main effect on the appearance of gingival hypertrophy is the fluctuating levels of sex hormones, appearing in the individual names of estradiol and testosterone and excluding here progesterone. (5) At the microscopic level, CD24 and CD146 cells are confirmed to be found in gingival hypertrophies caused by fixed orthodontic appliances (6), while the reduction of CD133 cells is observed. In cases of fixed orthodontic appliances, this source of study confirmed the genetic side of the process of the appearance of gingival hypertrophy. The reduction of gingival hypertrophy is indicated by the application of 40% chlorhexidine in gel form on the vestibular surface of already affected teeth, in the area of the maxillary molars on the vestibular surface. (7)
The treatment of these hypertrophies is indicated by the application of diode gingivectomy laser. (8) The application of antibiotics indicated for the treatment of periodontal diseases (9) is another way of treatment. Gingivectomy is the other solution from the periodontal side for the emerging problem(10) which is associated with an increase in Pentraxin 3 and Thrombospodin 1 biomarkers that reduce inflammation and increase angiogenesis.(11) gingival hypertrophy caused by specific bacteria such as prevotella, actinomyces, Porphiromonas is more based on the literature. (12) IL-1 and IL-8 are high in gingival hypertrophies caused by fixed orthodontic appliances, while IL-4 is at reduced levels. (13) Application of chlorhexidine causes a significant reduction of IL-1beta in the sulcus of teeth with gingival hypertrophy caused by fixed orthodontic appliances. (14) but there is a study that also emphasizes the fact that everything recovers and goes away by itself with regression of gingival hypertrophy, after just removing the orthodontic appliance, thus contradicting the fact that chlorhexidine or mouth rinses do not significantly affect the reduction or eventual disappearance of gingival hypertrophy. (17)
The patient’s periodontal status and his age are two other factors that attract the attention of studies at almost the same level of interest, leaving other factors such as the duration of orthodontic treatment and the socio-economic status of the patient at a lower level. Oral hygiene has an impact on the appearance of gingival hypertrophy in teeth with orthodontic appliances, this is expressed more in the area of the mandibular incisors than in the mandibular molars. It is not the amount of bacterial plaque, but its quality that directly affects the appearance of gingival hypertrophy.
List of Abbreviations
IV – vertical Index,
IH – Horisontal Index,
PBI – Index of Bacterial Pllaque,
CHX - Chlorhexidine
Ethics Declarations
Ethics approval and consent to participate As the authors of the article, we state that there is no violation of the code of ethics during the realization of this article. This study does not require an ethical approval since individual patient data is not included in any form. Availability of data and materials: The datasets analyzed during the current study are available from the corresponding author.
Authors’ contributions
IR and RK collected the scientific data and wrote the manuscript. SH and MK revised and edited the manuscript. Literature research was conducted by SH. IR and VO collected the scientific data. All authors read and approved the final manuscript.
Source of Funding
None.
Conflict of InterestNone.
Acknowledgements
Acknowledgments belong to our family. Henri and Hera are our motivation in the field of scientific research.
References
1. Eid HA, Assiri HA, Kandyala R, Togoo RA, Turakhia VS. Gingival enlargement in different age groups during fixed Orthodontic treatment. J Int Oral Health. 2014;6:3959129.
2. Zanatta FB, Ardenghi TM, Antoniazzi RP, Pinto TM, Rösing CK. Association between gingivitis and anterior gingival enlargement in subjects undergoing fixed orthodontic treatment. Dental Press J Orthod. 2014;19(3):59–66.
3. Almansob YA, Alhammadi MS, Luo XJ, Alhajj MN, Zhou L, Almansoub HA, et al. Comprehensive evaluation of factors that induce gingival enlargement during orthodontic treatment: A cross-sectional comparative study. Niger J Clin Pract. 2021;24(11):1649–55.
4. Vincent-Bugnas S, Borsa L, Gruss A, Lupi L. Prioritization of predisposing factors of gingival hyperplasia during orthodontic treatment: the role of amount of biofilm. BMC Oral Health. 2021;21(1):7903590.
5. Hosadurga R, Althaf MN, Hegde S, Rajesh KS, Kumar A. Influence of sex hormone levels on gingival enlargement in adolescent patients undergoing fixed orthodontic therapy: A pilot study. Contemp Clin Dent. 2016;7(4):506–11.
6. Baeshen HA, Alsulaimani FF, Awadh W, Ageeli MA, Abullais SS, Alqahtani NA, et al. Comparative assessment of the cell-surface antigens and gene expression profiles of the gingival tissue biomarkers in subjects with fixed functional and removable functional orthodontic appliances. Saudi J Biol Sci. 2021;29(3):1989–95.
7. Pretti H, Barbosa GL, Lages EM, García AG, Magalhães CS, Moreira AN, et al. Effect of chlorhexidine varnish on gingival growth in orthodontic patients: a randomized prospective split-mouth study. Dental Press J Orthod. 2015;20(5):66–71.
8. To TN, Rabie AB, Wong RW, Mcgrath CP. The adjunct effectiveness of diode laser gingivectomy in maintaining periodontal health during orthodontic treatment. Angle Orthod. 2012;83(1):43–7.
9. Draghici EC, Cr ˘ ai¸toiu ¸S, Mercu¸t V, Scrieciu M, Popescu SM, ˘ Diaconu OA, et al. Local cause of gingival overgrowth. Clinical and histological study. Rom J Morphol Embryol. 2016;57(2):472–35.
10. Li N, Wang W, Sun Y, Wang H, Wang T. Seven-year followup of a patient with hereditary gingival fibromatosis treated with a multidisciplinary approach: case report. . BMC Oral Health. 2021;21(1):473.
11. Rauten AM, Silosi I, Stratul SI, Foia L, Camen A, Toma V, et al. Expression of Pentraxin 3 and Thrombospondin 1 in Gingival Crevicular Fluid during Wound Healing after Gingivectomy in Postorthodontic Patients. J Immunol Res. 2016;1:1–7.
12. Monea M, Moldovan C. Rare Root Morphology of a Maxillary Central Incisor Associated With Gingival Hyperplasia: An Endodontic Case Report. . Medicine (Baltimore). 2016;95(18):e3617.
13. Zanatta FB, Ardenghi TM, Antoniazzi RP, Pinto TM, Rösing K. Association between gingivitis and anterior gingival enlargement in subjects undergoing fixed orthodontic treatment. Dental Press J Orthod. 2014;19(3):59–66.
14. Gong Y, Lu J, Ding X. Clinical, microbiologic, and immunologic factors of orthodontic treatment-induced gingival enlargement. Am J Orthod Dentofac Orthop. 2011;140(1):58–64.
15. Giannopoulou C, Mombelli A, Tsinidou K, Vasdekis V, Kamma J. Detection of gingival crevicular fluid cytokines in children and adolescents with and without fixed orthodontic appliances. Acta Odontol Scand. 2008;66(3):169–73.
16. Paschos E, Limbach M, Teichmann M, Huth KC, Folwaczny M, Hickel R, et al. Orthodontic attachments and chlorhexidine-containing varnish effects on gingival health. Angle Orthod. 2008;78(5):908–24.
17. Zanatta FB, Ardenghi TM, Antoniazzi RP, Pinto TM, Rösing CK. Association between gingival bleeding and gingival enlargement and oral health-related quality of life (OHRQoL) of subjects under fixed orthodontic treatment: a cross-sectional study. . BMC Oral Health. 2012;12:3534331.
18. Kouraki E, Bissada NF, Palomo JM, Ficara AJ. Gingival enlargement and resolution during and after orthodontic treatment. . N Y State Dent J. 2005;71(4):34–7.
19. Farhadian N, Bidgoli M, Jafari F, Mahmoudzadeh M, Yaghobi M, Miresmaeili A, et al. Comparison of Electric Toothbrush, Persica and Chlorhexidine Mouthwashes on Reduction of Gingival Enlargement in Orthodontic Patients: A Randomised Clinical Trial. . Oral Health Prev Dent. 2015;13(4):301–7.
20. Vincent-Bugnas S, Borsa L, Gruss A, Lupi L. Prioritization of predisposing factors of gingival hyperplasia during orthodontic treatment: the role of amount of biofilm. BMC Oral Health. 2021;21(1):1–8.
21. Herrera D, Escudero N, Pérez L, Otheo M, Cañete-Sánchez E, Pérez T, et al. Clinical and microbiological effects of the use of a cetylpyridinium chloride dentifrice and mouth rinse in orthodontic patients: a 3-month randomized clinical trial. Eur J Orthod. 2018;40(5):465–74.
22. Miranda J, Brunet L, Roset P, Farré M, Mendieta C. Reliability of two measurement indices for gingival enlargement. J Periodontal Res. 2012;47(6):776–82.
23. Pazzini CA, Júnior GO, Marques LS, Pereira CV, Pereira LJ. Prevalence of nickel allergy and longitudinal evaluation of periodontal abnormalities in orthodontic allergic patients. Angle Orthod. 2009;79(5):922–9.
24. Hosadurga R, Althaf MN, Hegde S, Rajesh KS, Kumar A. Influence of sex hormone levels on gingival enlargement in adolescent patients undergoing fixed orthodontic therapy: A pilot study. Contemp Clin Dent. 2016;7(4):506–11.
25. Mcgrath CP, Rabie AB, Wong RW. The adjunct effectiveness of diode laser gingivectomy in maintaining periodontal health during orthodontic treatment. Angle Orthod. 2012;83(1):43–7.
26. Sheehy EC, Roberts GJ, Beighton D, Brien O. Oral health in children undergoing liver transplantation. Int J Paediatr Dent. 2000;10(2):109– 28.
27. Renkema AA, Dusseldorp JK, Middel B, Ren Y. Zwelling van de gingiva bij orthodontische behandeling met volledig vaste apparatuur [Enlargement of the gingiva during treatment with fixed orthodontic appliances. Ned Tijdschr Tandheelkd. 2010;117(10):507–12.
28. Rde OG, Ciampioni AL. Prevalence of periodontal disease in the primary dentition of children with cerebral palsy. J Dent Child. 2004;71(1):27–32.
29. De Melo MC, Cardoso MG, Faber J, Sobral A. Risk factors for periodontal changes in adult patients with banded second molars during orthodontic treatment. Angle Orthod. 2011;82(2):224–8.
30. Van Gastel J, Quirynen M, Teughels W, Coucke W, Carels C. Influence of bracket design on microbial and periodontal parameters in vivo. J Clin Periodontol. 2007;34(5):423–54.
31. Kloehn JS, Pfeifer JS. The effect of orthodontic treatment on the periodontium. Angle Orthod. 1974;44(2):452–8.
