Full HTML
Intracerebral hemorrhage developing in a patient with posterior reversible encephalopathy syndrome; a case report
Hatice Güldal1, Aziz Alper Ayaslı2, Alp Kaan Furkan Kıcıroğlu1, Salih Karakoyun3, Mustafa Boğan3
Author Affiliation
1Resident, Department of Emergency, School of Medicine, Düzce University
2Specialist, Department of Neurology, Düzce Atatürk State Hospital, Duzce, Turkey
3Consultant, Department of Emergency, School of Medicine, Düzce University
Abstract
We describe a case of hemorrhagic posterior reversible encephalopathy syndrome (PRES) in a 19-year-old woman, who had undergone a cesarean section for epilepsy and lupus-related chronic renal failure 2 months ago, and presented to the emergency department with complaints of blurred vision. The neurological and ophthalmological examinations were normal. Despite the initial imaging being normal, subsequent magnetic resonance images showed hyperintensity in bilateral occipital lobes and cerebellum (indicative of PRES) and watershed ischemia in addition to intracerebral hemorrhage. Brain surgery was performed, external ventricular drainage was placed and she was monitored postoperatively with routine care in the intensive care unit where she remained intubated for a month, after which she died of the consequences of her condition.
DOI: 10.32677/yjm.v3i1.4326
Keywords: Emergency department, Intracerebral hemorrhage, Posterior reversible encephalopathy syndrome
Pages: 60-62
View: 7
Download: 10
DOI URL: https://doi.org/10.32677/yjm.v3i1.4326
Publish Date: 11-05-2024
Full Text
Introduction
Posterior Reversible Encephalopathy Syndrome (PRES) is a reversible clinical condition characterized by non-specific neurological symptoms such as headache, altered consciousness, seizures, and visual disturbances [1,2,3]. It is usually associated with or triggered by hypertension, eclampsia, renal failure, immunosuppression, and autoimmune diseases, including systemic lupus erythematosus (SLE), as well as cytotoxic drugs [2,3,4]. Although there are different views on its pathophysiology, it is known to be caused by endothelial dysfunction, which results in the disruption of the blood-brain barrier under the influence of endogenous factors (eg, sepsis) and exogenous factors (cytotoxic and immunosuppressive agents) as well as hypertension-related hyperperfusion and impairment of cerebral autoregulation [1,3,4].
With the increasing availability of neuroimaging techniques, such as MRI, an increase in PRES cases has been observed in recent years [2]. The differential diagnosis of PRES requires consideration of several neurological diseases such as viral and autoimmune encephalitis, demyelinating disease, toxic leukoencephalopathy, malignancies such as gliomatosis cerebri, central nervous system vasculitis, central/extrapontine myelinolysis, and acute stroke, especially cerebral venous thrombosis [4].
PRES is a clinicoradiological diagnosis supported by clinical features, risk factors, and findings on magnetic resonance imaging (MRI) of the brain [1,4]. Diagnosis is facilitated by the presence of posterior subcortical edema on MRI, and restricted diffusion can be seen on diffusion-weighted imaging (DWI) [1,4]. Although bleeding is considered atypical in PRES, it can still occur [4,5]. The present case report describes a 19-year-old female patient who presented to the emergency department with visual symptoms, was suspected of having PRES based on MRI findings, and developed a intracerebral cerebral hemorrhage during follow-up.
Case Report
A 19-year-old woman, who had undergone a cesarean section for epilepsy and lupus-related chronic renal failure two months ago, presented to the emergency department with complaints of blurred vision. In addition to visual symptoms, she reported nausea, vomiting, and diarrhea for the past three days, with at least 6-7 episodes of watery stools daily. She initially had blurred vision, followed by a brief period of complete vision loss, but when she presented to the emergency room she complained only of blurred vision. According to her self-report, she had blurred vision beyond approximately one meter. Two months prior to this presentation, when she was seven months pregnant, she developed nephrotic syndrome and underwent a cesarean section. She subsequently underwent dialysis and was diagnosed with lupus nephritis based on a kidney biopsy. During follow-up, she experienced epileptic seizures resulting in status epilepticus and was intubated and monitored in the intensive care unit. After follow-up, she was extubated and discharged 14 days later. Since then, she has been undergoing dialysis three times a week. Her medications include Valproic acid 500 mg q24hr PO, Folic acid 5 mg q24hr PO, Methylprednisolone 32 mg q24hr PO, Methyldopa 250 mg q8hr PO, Carvedilol 6.25 mg q12hr PO, Lansoprazole 30 mg q24hr PO. Two days before the current presentation, she was prescribed Ciprofloxacin 250 mg q12hr PO and Metronidazole 500 mg q12hr PO due to nausea, vomiting, and diarrhea, but her symptoms did not improve.
Upon examination, she was conscious, cooperative, and oriented. Her temperature was 36.3°C and her initial blood pressure was measured at 177/128 mmHg. Other vital signs were normal. Examination of the eyes revealed intact ocular structures, including eyelids, conjunctiva, cornea, and sclera. Eye movements were coordinated and there was no diplopia. Bilateral light reflexes were triggered. Other cranial examinations and other systems examinations were unremarkable, except that bilateral pretibial edema was noted.
The electrocardiogram showed normal sinus rhythm with a rate of 100 beats per minute. The patient's medical history revealed epilepsy, hypertension, lupus nephritis, and chronic kidney failure requiring continuous dialysis. Initial considerations include electrolyte imbalances, central nervous system pathologies (hemorrhagic or ischemic stroke), ocular pathologies (retinal detachment, cataract, vitreous hemorrhage, retinal artery or venous occlusion, and hypertensive retinopathy) that require further investigations. Hemoglobin was 11.27 g/dL, creatinine was 4.31 mg/dL, and C-reactive protein was 0.86 in biochemical tests. No other abnormal laboratory findings were observed. Contrast-free cranial computed tomography (CT) and diffusion-weighted imaging (DWI) did not show any significant pathology during the emergency department visit. However, during follow-ups, the patient experienced generalized tonic-clonic seizures 2-3 times in the emergency department.
Based on the existing symptoms, PRES was suspected. The patient was admitted to the hospital for monitoring and blood pressure control. In the 15th hour of follow-up, when her consciousness worsened, CT and MRI were performed. The CT scan revealed a 44x47 mm intraparenchymal hemorrhage with vasoconstrictive edema at the juxtacortical junction, extending from the left lateral ventricles to the deep white matter and basal ganglia (Figure 1). MRI showed hyperintensity in bilateral occipital lobes and cerebellum (indicative of PRES) and watershed ischemia in addition to the hemorrhagic area (Figures 2 & 3).
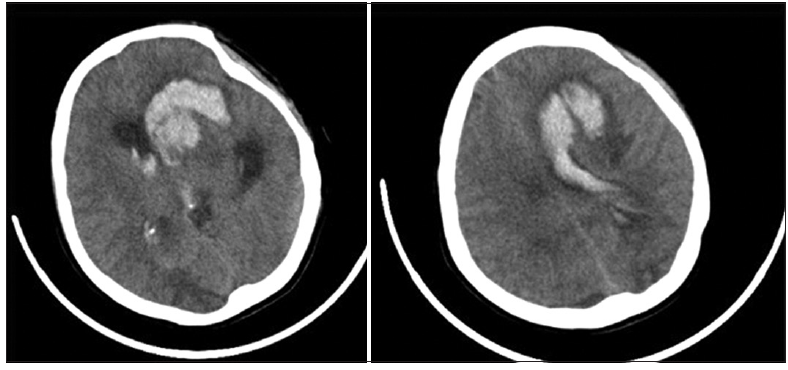
Figure 1: Computed tomography image showing extensive hemorrhage
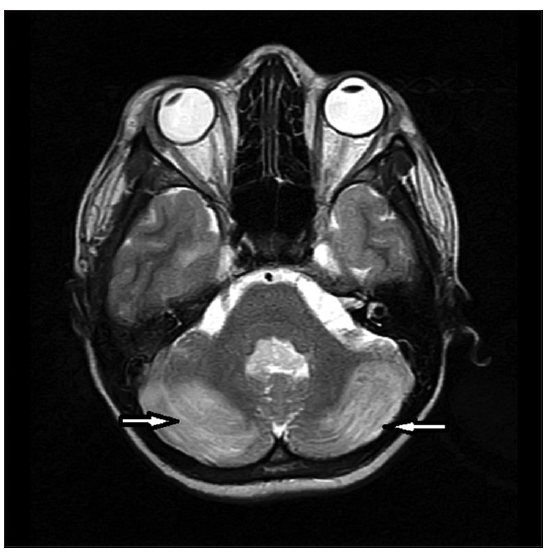
Figure 2: Hyperintensity in the cerebellum (white arrows)
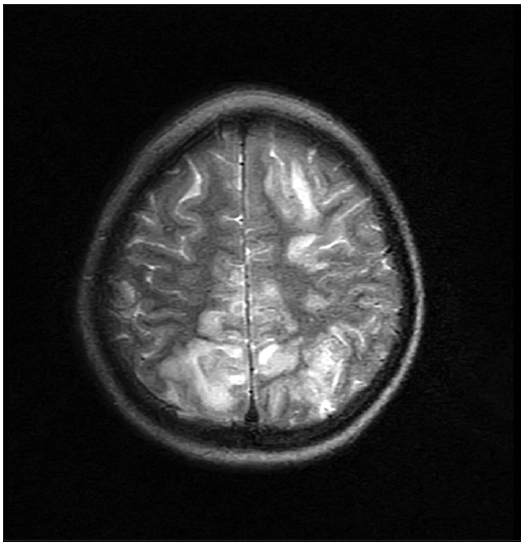
Figure 3: Magnetic resonance imaging showing watershed ischemia
Brain surgery was performed, external ventricular drainage was placed and she was monitored postoperatively with routine care in the intensive care unit where she remained intubated for a month, after which she died of the consequences of her condition.
Discussion
Posterior Reversible Encephalopathy Syndrome (PRES) is a reversible clinical-radiological condition characterized by non-specific neurological symptoms. PRES can occur at any age, from infants to the elderly, but it most commonly affects young or middle-aged adults, with an average age of 45 [4]. It is frequently reported in patients receiving immunosuppressive drugs after solid organ, bone marrow, or stem cell transplantation [6-8]. Impaired kidney function has been reported in 55% of patients with PRES [6,9,10]. However, it is unclear whether accompanying arterial hypertension or kidney dysfunction itself is the primary causative factor [6]. Although the underlying pathophysiological changes of PRES are not fully understood, endothelial dysfunction is considered a significant factor. Acute neurological symptoms of PRES should also be considered in patients with renal failure, blood pressure fluctuations, taking cytotoxic drugs, autoimmune diseases, or eclampsia [11,12]. The patient discussed in this report was a 19-year-old female who has some of these risk factors, such as a history of autoimmune disease and hypertension.
The diagnosis of PRES is typically made through magnetic resonance imaging (MRI) of the brain. Imaging characteristically shows focal areas of symmetric hyperintensities in T2-weighted studies, most commonly in the parietal and occipital lobes, followed by the frontal lobes and cerebellum [13]. The distinctive feature of PRES lesions in diffusion-weighted imaging (DWI) is the vasogenic edema pattern [14]. Diffusion-weighted MRI reliably distinguishes vasogenic edema in PRES from cytotoxic edema in the setting of cerebral ischemia [14]. CT is less sensitive than magnetic resonance imaging (MRI) in detecting initial findings. In one study, up to 22% of cases had a normal initial CT [14]. Edema is often widespread in CT but predominant in parietal and occipital regions, followed by frontal lobes, the lower temporal-occipital junction, and the cerebellum [15]. The treatment of PRES is generally a conservative approach. Blood pressure should be controlled, and close monitoring is essential. Treatment planning for the underlying etiology, correction of metabolic disorders, planning delivery in the case of preeclampsia, discontinuation of medication in drug-induced cases, etc., should be considered [16]. Antiepileptic treatment should be arranged, with preference given to benzodiazepines (lorazepam or diazepam), and initiation should not be delayed [16]. If seizures persist, phenytoin, fosphenytoin, or barbiturates are recommended [17].
Complete resolution occurs within 2 to 8 days in 75 to 90% of PRES cases, whereas rare case reports show progression without complete recovery [18]. In one study, 44% of patients continued to experience significant functional loss 90 days after PRES diagnosis. Delays in diagnosis and treatment can lead to death or irreversible neurological symptoms [19]. If PRES is not treated promptly, infarction or bleeding may occur [14]. In one study, PRES was associated with various types of bleeding in 15.1% of cases, including minor bleeding, subarachnoid hemorrhage, and hematoma [13]. Brainstem involvement and intracranial hemorrhage have a poor prognosis [14]. Although initial imaging was normal, follow-up imaging in this case showed an unexpectedly large area of hemorrhage..
Conclusion
This case presentation addresses the clinical course of PRES, which initially manifested with non-specific neurological symptoms, and focuses on a rare complication. The patient, with a history of lupus nephritis, chronic kidney failure, epilepsy, and hypertension, falls into the risk group for PRES. Magnetic resonance imaging (MRI) is crucial for diagnosis, and treatment typically involves a conservative approach. However, in this case, suspicion arose despite normal imaging. The rare hemorrhagic complication of PRES can be prevented with early diagnosis and treatment, but in this instance, due to the extensive hemorrhagic area and the development of hydrocephalus, the patient did not survive.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient for publication of this case report and all accompanying images.
AUTHORS’ CONTRIBUTIONS
All authors contributed to the completion of this work. The final manuscript was read and approved by all authors
References
- Patel SP, Jarbath M, Saravis L, et al. Pheochromocytoma manifesting as cortical blindness secondary to PRES with associated TMA: a case report and literature review. BMC Endocr Disord. 2022;22(1):205.
- Chaudhuri J, Basu S, Roy MK, et al. Posterior Reversible Leucoencephalopathy Syndrome: Case Series, Comments, and Diagnostic Dilemma. Curr Neurol Neurosci Rep. 2023;23(8):433-449.
- Baisya R, Kumar Devarasetti P, Narayanan R, et al. Posterior reversible encephalopathy syndrome in juvenile lupus- a case series and literature review. Lupus. 2022;31(5):606-612.
- Triplett JD, Kutlubaev MA, Kermode AG, et al. Posterior reversible encephalopathy syndrome (PRES): diagnosis and management. Pract Neurol. 2022;22(3):183-189.
- Aranas RM, Prabhakaran S, Lee VH. Posterior reversible encephalopathy syndrome associated with hemorrhage. Neurocrit Care. 2009;10(3):306-312.
- Fischer M, Schmutzhard E. Posterior reversible encephalopathy syndrome. J Neurol. 2017;264(8):1608-1616.
- Bartynski WS, Tan HP, Boardman JF, et al. Posterior reversible encephalopathy syndrome after solid organ transplantation. AJNR Am Soc Neuroradiology. 2008; 29 (5):924–930.
- Masetti R, Cordelli DM, Zama D, et al. PRES in children undergoing hematopoietic stem cell or solid organ transplantation. Pediatrics. 2015; 135 (5):890–901.
- Fugate JE, Rabinstein AA. Posterior reversible encephalopathy syndrome: clinical and radiological manifestations, pathophysiology, and outstanding questions. Lancet Neurology. 2015; 14 (9):914–925.
- Bartynski WS. Posterior reversible encephalopathy syndrome, part 1: fundamental imaging and clinical features. American Journal of Neuroradiology, 2008; 29 (6):1036–1042.
- Fugate JE, Rabinstein AA. Posterior reversible encephalopathy syndrome: clinical and radiological manifestations, pathophysiology, and outstanding questions. Lancet Neurol. 2015;14(9):914-925.
- Sulaiman TO, Yasin AK, Ismail A. A case of cyclophosphamide-induced posterior reversible encephalopathy syndrome: Is it dose-related side effect? Yemen J Med. 2022;1(2):103-107.
- Gewirtz AN, Gao V, Parauda SC, et al. Posterior Reversible Encephalopathy Syndrome. Curr Pain Headache Rep. 2021;25(3):19.
- Shankar J, Banfield J. Posterior Reversible Encephalopathy Syndrome: A Review. Can Assoc Radiol J. 2017;68(2):147-153.
- Bartynski, W. S.Posterior reversible encephalopathy syndrome, part 1: fundamental imaging and clinical features. American Journal of Neuroradiology, 2008: 29(6), 1036-1042.
- Servillo G, Bifulco F, De Robertis E, et al. Posterior reversible encephalopathy syndrome in intensive care medicine. Intensive Care Med 2007;33(2):230-6.
- Marchetti A, Magar R, Fischer J, et al. A pharmacoeconomic evaluation of intravenous fosphenytoin (Cerebyx) versus intravenous phenytoin (Dilantin) in hospital emergency departments. Clin Ther1996;18(5):953-66.
- ÇETİN, G. Y. Posterior Reversibl Ensefalopati Sendromu: Sistemik Lupus Eritematozuslu hastalarda görülen nadir ve acil klinik bir antite. Kahramanmaraş Sütçü İmam Üniversitesi Tıp Fakültesi Dergisi, 2023; 15(2): 116-119.
- Legriel S, Schraub O, Azoulay E, et al. Determinants of recovery from severe posterior reversible encephalopathy syndrome. PLoS One 2012;7(9):e44534. doi: 10.1371/journal.pone.0044534.
