Full HTML
Rupture of sinus of Valsalva aneurysm in a young adult male: A case report
Özkan Kömürcü1, Cem Atik2, Metehan Özen3, Hatice Güldal4, Mustafa Boğan5
Author Affiliation
1Specialist, Primary Health Care Corporation, Umm Salal Health Center, Umm Salal Muhammed/Qatar
2Consultant, Department of Cardiovascular Surgery, Private Yeni Hayat Hospital, Osmaniye
3Consultant
4Resident, Department of Emergency, Medicine Faculty
5Consultant, Department of Emergency, School of Medicine, Düzce University, Düzce, Turkey
Abstract
Rupture of the sinus of Valsalva aneurysm (SVA) is a surgical emergency. It can be fatal if not treated properly and on time. In this report, we present a 39-year-old male patient with no known disease who was admitted to the emergency department with complaints of pressure-such as chest pain, chest tightness, and an inability to breathe easily after a heavy meal at night. Thoracic and abdominal computed tomography angiography was performed to better evaluate the vascular structures; the ascending aorta diameter was 71 mm (wider than normal). Hemorrhagic fluid was observed in the pericardial space and paracardiac recesses. The preliminary diagnosis was a rupture of the right SVA, and emergency surgery was performed. The posterior aorta was found to have ruptured at the level of the right sinus of Valsalva, and anastomosis was performed on the torn portion. The patient was extubated 8 h after surgery. On the 7th post-operative day, transthoracic echocardiography was within normal limits, and he was discharged from the hospital on the 8th day in good condition with stable vital signs.
DOI: 10.32677/yjm.v3i1.4410
Keywords: Acute coronary syndrome, Rupture, Sinus of Valsalva aneurysm
Pages: 57-59
View: 6
Download: 9
DOI URL: https://doi.org/10.32677/yjm.v3i1.4410
Publish Date: 11-05-2024
Full Text
INTRODUCTION
There are three sinuses of Valsalva surrounding the aortic valve. These are the right coronary sinus, the left coronary sinus, and the noncoronary sinus on the back of the aortic valve between these two sinuses [1]. A sinus Valsalva aneurysm (SVA) results from the weakening of the regions between the sinuses due to the lack of elastic fibers between the median layer of the aorta and the muscular layer [2]. SVA is defined as the enlargement of the coronary sinuses due to the absence of elastic tissue between the aorta and the annulus fibrosus [2,3]. The function of the sinuses is to prevent occlusion of the coronary artery ostia when the aortic valve is opened during systole [4].
SVA has two clinical forms namely congenital and acquired. Congenital SVA accounts for 0.1-3.5% of congenital heart disease cases [1,2,5]. The origin is most commonly in the right coronary sinus (70–90%), less frequently in the noncoronary sinus (10–20%) and rarely in the left sinus (<5%). An acquired sinus of Valsalva aneurysm can be seen with a variety of conditions such as infective endocarditis, tuberculosis, Behçet disease, and trauma [1].
Rupture of the SVA is a surgical emergency. It can be fatal if not treated properly and on time. Treatment options include open or endovascular surgery, percutaneous repair, or procedures such as external heart support [6]. In this case report, we present a 39-year-old male patient with no previous illness who was diagnosed with SVA rupture after sudden onset chest pain. We describe this case to emphasize the importance of early diagnosis to avoid life-threatening complications and poor outcome.
CASE REPORT
A 39-year-old patient with no known illness was admitted to the emergency department with complaints of pressure-like chest pain, chest tightness, and inability to breathe easily after a large night meal (he described it as fatty and salty ). The personal and family history was unremarkable. He was not taking any medication.
On initial examination, the patient appears to be in good general condition, conscious and oriented. Vital signs observed were as follows: temperature, 36.5°C; heart rate 85 beats per minute; blood pressure 110/70 mmHg; and respiratory rate of 22 breaths per minute. Cardiac examination revealed a continuous systolic murmur at the left sternal border, while pulses were evident in both upper extremities in equal volumes. No significant differences were observed in blood pressure measurements in the two arms.
A 12-lead electrocardiogram appeared normal at his initial visit and during his follow-up visit. Initial blood tests, including cardiac troponin, complete blood count (CBC), renal and liver function tests, and serum electrolytes, were within normal limits. However, due to the high likelihood of cardiac-related chest pain, a follow-up troponin level test was requested and a cardiology team was consulted.
A transthoracic echocardiography, showed ejection fraction of 60% with normal left ventricular systolic functions. There was aortic root enlargement and aortic insufficiency. No significant fluid was observed in the pericardial space. Thoracic and Abdominal Computed Tomography Angiography (CTA) was performed to better evaluate the vascular structures; the ascending aorta diameter was 71 mm (wider than normal), and hemorrhagic fluid was observed in the pericardial space and paracardiac recesses (Figures 1 and 2). The preliminary diagnosis was a rupture of the right SVA and the cardiovascular surgery team was consulted.
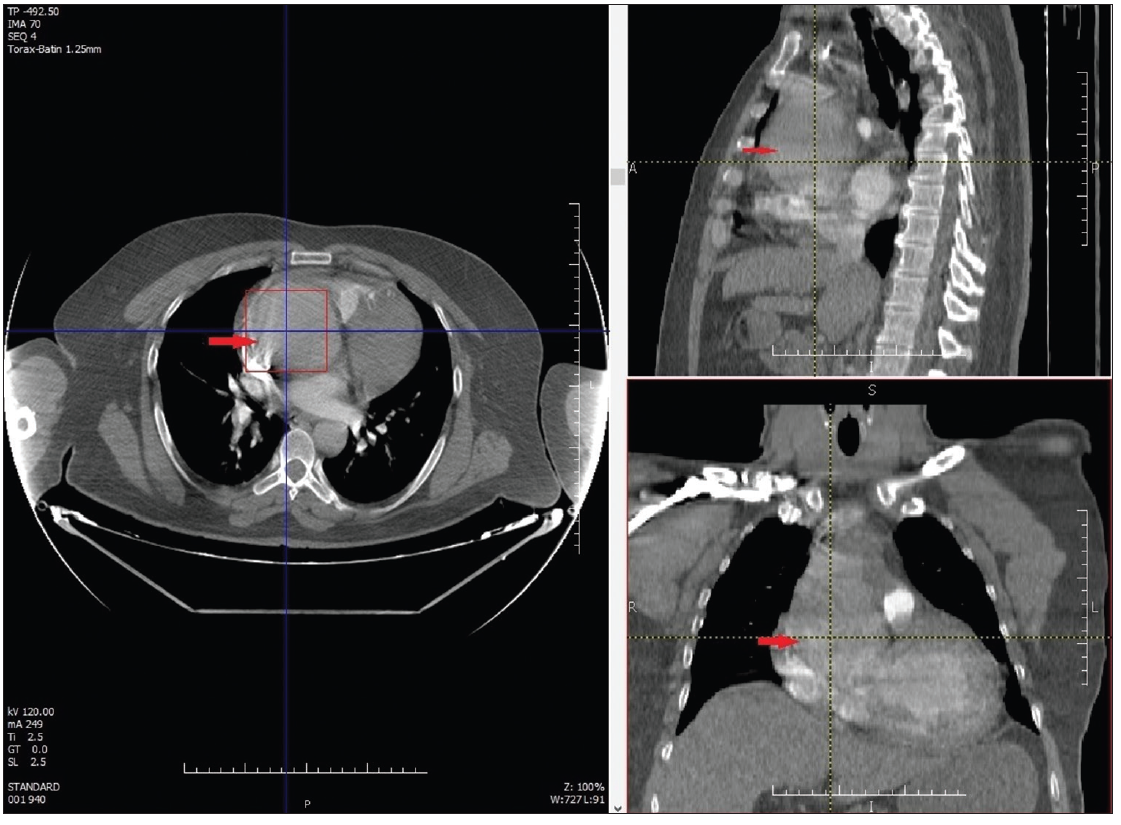
Figure 1: Sinus Valsalva aneurysm at the level of the right coronary artery (red arrows)
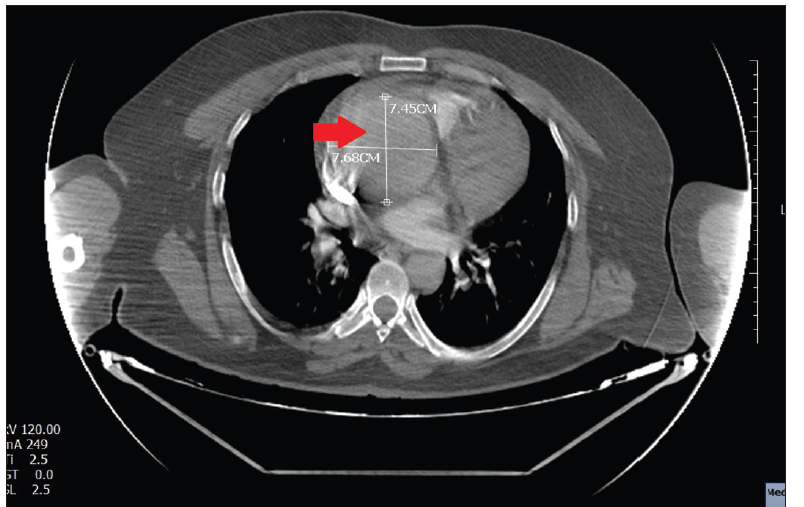
Figure 2: Enlarged aortic root (red arrow)
A preoperative transthoracic echocardiography was performed. A new pericardial effusion with a diameter of 1.5 cm was noted. The patient was taken into the operation theater, and about 1000cc of hemorrhagic fluid was drained from the pericardial area. The aorta was found to have posteriorly ruptured at the level of the right sinuse of Valsalva and anastomosis was performed on the torn portion. The patient was extubated 8 hours after surgery. On the 7th postoperative day, transthoracic echocardiography was within normal limits and the patient was discharged from the hospital on the 8th day in good condition and stable vital signs.
Discussion
The estimated prevalence of SVA is 0.09% in the population, with men being affected more frequently than women [1-3]. SVA can be either acquired or congenital. In congenital SVA, the pathology is often associated with Marfan syndrome, Ehlers-Danlos syndrome or other connective tissue diseases [1,2,5], whereas acquired aneurysms are caused by events and conditions that weaken the juncture between the media and the annulus fibrosus of the aorta by trauma, bacterial endocarditis, syphilis, tuberculosis, and atherosclerosis [1,2,5]. The right coronary sinus is the most common site of occurrence [1,2]. Our case also involves a man who presented with a rupture of the right SVA. Although the acquired causes in our patient have not been thoroughly investigated, SVA is most likely congenital since our patient was young and without known structural or acquired heart disease.
Although Unruptured SVAs are usually clinically asymptomatic, the use of advanced diagnostic techniques has made SVAs detected incidentally during echocardiography and cross-sectional imaging for other indications more common [7]. Unruptured SVAs can be accompanied by a variety of symptoms, including shortness of breath, palpitations, angina, irregular heartbeat, atrial fibrillation, and complete heart block [1,2,5,7]. Very large aneurysms can serve as a nidus for thrombus formation, leading to obstruction of major coronary arteries and ischemic heart disease [2]. Furthermore, signs of aortic insufficiency can be observed in up to half of unruptured SVA cases [5]. Our patient was asymptomatic until the SVA ruptured.
Rupture is the most common complication of SVA and occurs most frequently between the ages of 20 and 40 [2]. Patients typically experience symptoms such as chest pain, shortness of breath, palpitations, fatigue, and syncope. Symptoms may progress gradually from the onset or progress rapidly, leading to sudden death [2,5,8,9]. Our patient's age falls within the above range and he presented with chest pain, chest tightness, and difficulty breathing after a heavy meal.
The rapid and accurate diagnosis of rupture of SVA requires a high index of suspicion and proper use of cardiac imaging [1-4]. Clinicians should be aware of SVA rupture in young patients (particularly those with no or low cardiac risk factors) who present with signs and symptoms of myocardial ischemia, heart failure, or cardiac conduction defects.
Diagnosis of sinus of Valsalva aneurysm is facilitated by echocardiography, computed tomographic angiography (CTA), cardiac catheterization, aortic artery angiography (CAG), and magnetic resonance imaging [1,2,5]. In our case, the transthoracic echocardiogram revealed aortic root enlargement and aortic insufficiency, while CTA enabled the diagnosis of ruptured right SVA. Unruptured SVAs may require surgery if they lead to conditions such as arrhythmias, encroach on nearby structures causing myocardial ischemia, or pose a risk of rupture. However, optimal management of an asymptomatic, unruptured SVA is less clear. Treatment of a ruptured SVA typically entails surgery [1–5], but percutaneous closure techniques have also been adopted by some centers [6].
If SVA ruptures, the prognosis is very poor if left untreated. Sawyers et al. [10] documented a mean survival time of 3.9 years in patients with untreated SVA rupture. After the repair, the life expectancy of the patients is approximately the same as that of the healthy population. A satisfactory prognosis after surgical repair has been reported, with an event-free survival of approximately 90% at 15 years [11]. In the current case, surgical repair was successfully performed and the patient was discharged in good condition.
Conclusion
AVS and its complications may be a potential cause of acute chest pain in people without known structural or acquired heart disease. Although rare, this potentially fatal disease requires rapid recognition and intervention. Therefore, clinicians need to be more aware of the symptoms, differential diagnosis, and clinical conditions mimicked by VAS. It should be kept in mind that it is part of the differential diagnosis in patients with acute coronary syndrome.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient for publication of this case report and all accompanying images.
AUTHORS’ CONTRIBUTIONS
All authors contributed to the completion of this work. The final manuscript was read and approved by all authors
References
Hoey ET, Kanagasingam A, Sivananthan MU. Sinus of valsalva aneurysms: assessment with cardiovascular MRI. AJR Am J Roentgenol. 2010 Jun;194(6):W495-504.
Weinreich M, Yu PJ, Trost B. Sinus of Valsalva aneurysms: review of the literature and an update on management. Clin Cardiol. 2015;38:185–9.
Jiang K, Chen J, Zhu X, et al. Rupture of sinus of Valsalva aneurysm: a case report in a child. BMC Cardiovasc Disord 22, 158 (2022).
Bass D, Tivakaran VS. Sinus Of Valsalva Aneurysm. [Updated 2023 Feb 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448198/ [accessed on 2 January 2024]
Feldman DN, Roman MJ. Aneurysms of the sinuses of Valsalva. Cardiology. 2006;106:73–81.
Paymard M, Higgins MD, Sinhal A, et al. Surgical or Percutaneous Repair of Sinus of Valsalva Rupture: Case Series and Literature Review. Heart Views. 2023;24(3):148-152.
Wang ZJ, Zou CW, Li DC, et al. Surgical repair of sinus of Valsalva aneurysm in Asian patients. Ann Thorac Surg 2007; 84:156 –160
Ayati A, Toofaninejad N, Hosseinsabet A, et al. Transcatheter closure of a ruptured sinus of valsalva: a systematic review of the literature. Front Cardiovasc Med. 2023;10:1227761.
Huang TT, Shan JG, Lin JH. Rupture of a non sinus of Valsalva aneurysm during pregnancy: Case report and review of literatures. Niger J Clin Pract. 2023;26(2):250-252.
Sawyers JL, Adams JE, Scott HW. Surgical treatment of aneurysms of the aortic sinuses with aorticoatrial fistula; experimental and clinical study. Surgery. 1957;41(1):26-42
Doost A, Craig JA, Soh SY. Acute rupture of a sinus of Valsalva aneurysm into the right atrium: a case report and a narrative review. BMC Cardiovasc Disord. 2020;20(1):84.
