Full HTML
Hypertrophic pachymeningitis during radiotherapy for locally advanced prostate cancer: A coincidental or causal relationship
Yukihiro Hama1, Etsuko Tate1
Author Affiliation
1Consultant, Department of Radiation Oncology, Tokyo-Edogawa Cancer Centre, Edogawa Hospital, Tokyo, Japan
Abstract
Hypertrophic pachymeningitis (HP) is a rare clinical disorder characterized by focal or diffuse thickening of the dura mater with various neurological manifestations. It is known to be associated with autoimmune diseases, infections, and neoplasms. However, a review of the literature did not reveal that HP occurs during radiotherapy for cancer. In this report, we present a rare case of HP during radiotherapy for cancer in a 71-year-old male patient with high-risk prostate cancer who developed a headache and abducens nerve palsy during radiotherapy following androgen deprivation therapy. Magnetic resonance imaging (MRI) revealed dura mater thickening without brain metastases. The cerebrospinal fluid analysis demonstrated elevated protein levels. The patient was diagnosed with HP and treated with oral prednisolone. Within 2 days of treatment, the headache subsided, and the abducens nerve palsy resolved completely after 6 months of radiotherapy. In view of these events, we suggested a possible correlation between radiotherapy and HP, particularly, if meningitis develops during radiotherapy in the absence of infection or cancer seeding.
DOI: 10.63475/yjm.v3i1.4509
Keywords: Abducens nerve palsy, Adverse effects, Dura mater, Hypertrophic pachymeningitis, Radiation-induced abnormalities
Pages: 54-56
View: 4
Download: 5
DOI URL: https://doi.org/10.63475/yjm.v3i1.4509
Publish Date: 11-05-2024
Full Text
INTRODUCTION
Hypertrophic pachymeningitis (HP) is a rare clinical disorder characterized by focal or diffuse thickening of the dura mater with various neurological manifestations such as headache, cranial nerve palsy, cerebellar ataxia, and paralysis [1,2]. HP is associated with several autoimmune diseases such as ANCA-associated vasculitis, rheumatoid arthritis, sarcoidosis, and IgG4-related disorder; infections such as tuberculosis, syphilis, and fungus diseases; neoplasms such as lymphoma, but in some cases, the cause of HP is unknown [1,2]. To our knowledge, there have been no reports of HP during radiotherapy for malignant tumors. Here we report a rare case of HP that developed during radiotherapy for locally advanced prostate cancer to increase the awareness of clinicians of the HP as a possible complication of radiotherapy.
CASE REPORT
A 71-year-old man with no significant past medical history was referred to our institution for radiotherapy for high-risk prostate cancer (initial prostate specific antigen [PSA] 20.2 ng/mL, Gleason score 4+3, cT2c N0 M0) after 6 months of maximal androgen deprivation therapy (MADT). Six months after MADT, PSA levels dropped below the detection limit. The patient underwent intensity-modulated radiation therapy (IMRT) at 2 Gy per fraction, for a total dose of 76 Gy. When 14 Gy of IMRT was performed, diplopia and headache appeared. Fundoscopy revealed no abnormality, but right abducens nerve palsy was noted.
Brain MRI showed no brain metastases or brainstem lesions (Figure 1a), but the dura mater was diffusely thickened. Contrast-enhanced MRI showed enhancement of the dura mater (Figure 1b).
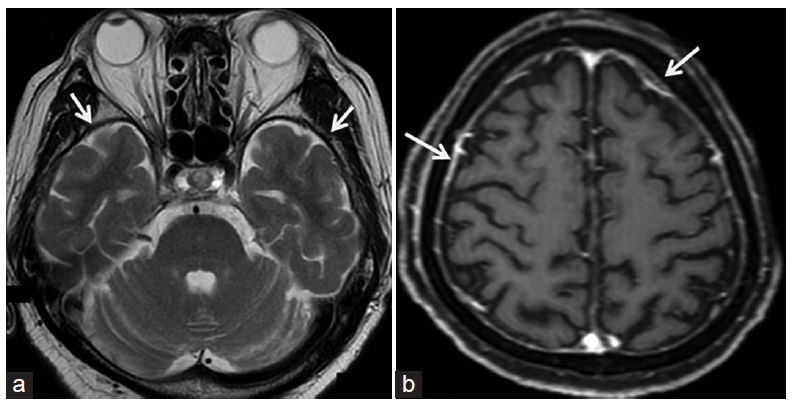
Figure 1: MRI of a 71-year-old man with hypertrophic pachymeningitis. (a) T2-weighted MRI shows no intramedullary lesions. The dura mater is thickened (arrows). (b) Gadoliniumenhanced T1-weighted MRI demonstrates diffuse thickening and enhancement of meninges (arrows). MRI: Magnetic resonance imaging
Cerebrospinal fluid (CSF) analysis showed total proteins of 0.875 g/L (normal: 0.15-0.45 g/L), cell count of 2 lymphocytes/uL, and glucose level of 70 mg/dL (normal: 50-80 mg/dL), while the CSF microbiology study was negative for Gram stain and no growth of microorganisms was observed. Concentrations of IgG, IgM, and acetylcholine receptor antibodies in CSF were all within normal limits. Blood test results showed aspartate aminotransferase (AST) level of 55 IU/L (normal: 11-35 IU/L), and lactate dehydrogenase (LDH) levels of 373 IU/L (normal: 105-237 IU/L). Complete blood count (CBC) test, kidney function tests, prostate-specific antigen (PSA) level, C-reactive protein level, and levels of IgG and IgM were within normal limits. Based on MRI findings, CSF analysis, and blood tests, a diagnosis of HP was made, which was most likely attributed to radiation therapy. Oral prednisolone was administered at a dose of 30 mg per day, which relieved the headache within two days, but the abducens nerve palsy remained. Prednisolone was continued during radiotherapy, but the dose was gradually tappered on the next days and finally discontinued after 2 weeks of radiotherapy. MADT was also stopped when radiation therapy was completed. The post-treatment course was uneventful, with no adverse events or relapses occurring during the 6-month follow-up after radiotherapy. Diplopia and abducens palsy gradually improved without treatment and were completely cured 6 months after radiotherapy.
DISCUSSION
HP can be caused by a variety of diseases, including infections (tuberculosis, syphilis, fungal infections), autoimmune/inflammatory diseases (granulomatosis with polyangiitis, sarcoidosis, and IgG4-related diseases), malignancies, and drug reactions, however, the cause is often idiopathic [1,2]. To our knowledge, this is the first case suggesting that cancer radiation can trigger HP.
HP has a variable clinical presentation depending on the underlying etiology and location of the lesion as well as the thickness of the dura mater on brain imaging. Headache and multiple cranial neuropathy are the most common clinical manifestations. Extraneurologic or systemic manifestations of HP may help define the etiology [3]. Contrast-enhanced MRI imaging is essential for HP diagnosis and its progression monitoring [4]. However, the etiological diagnosis of HP through clinical, laboratory, and imaging workup remains a challenge, and the final diagnosis is usually performed with tissue biopsy. It is essential to rule out infectious diseases, autoimmune/inflammatory diseases, and malignancies, especially lymphomas [3].
We hypothesized that the HP in our patient was most likely due to radiotherapy because there were no extraneurological manifestations. or systemic symptoms suggestive of the underlying etiology, in addition, MRI showed no matastases, while CSF studies were negative for infection with normal levels of IgG, IgM, and acetylcholine receptor antibodies. The pathogenesis of HP during radiotherapy is unclear. We propse that radiotherapy-induced tissue damage and antigen release [5,6] followed by an autoimmune reaction are the possible mechanism.
Treatment of HP depends on the underlying predisposing factor. For example, if the infections are the cause of HP, treatment would focus on treating the infection [7]. In Idiopathic HP, the most commonly used regimen is steroids (prednisone 1 mg/kg/day) [3]. On the other hand, the treatment of radiotherapy-associated HP is unclear. In our case, early initiation of oral prednisolone proved remarkably effective, resulting in complete resolution of headache within 2 days and complete abduction recovery 6 months later. However, strict exclusion of infectious causes is essential for the introduction of immunotherapy, as in cases of idiopathic and autoimmune/inflammatory PH.
There are some limitations to this case report. First, this is a report of a single case and not a large cohort study. Therefore, the relationship between radiation therapy and HP will remain a subject of debate, as the cause-and-effect relationship has not yet been directly investigated. Second, data on pathological and immunohistochemical findings were not available because tissue biopsy was not performed. Since the biopsy of the dura mater is an invasive procedure that is not free from serious complications, and since there was no suspicion of infection or the spread of cancer cells in the meninges based on MRI and CSF examinations, a tissue biopsy would not be necessary.
CONCLUSION
We observed an association between radiotherapy and HP in our case. However, it is still too early to draw a conclusion as we may only be in the early stages of learning about a possible link between radiation therapy and HP. An important challenge in our case is establishing causality, because it is unclear whether the relation between radiotherapy and HP is causal or incidental. Could radiotherapy be considered a new etiological risk factor for HP in the future? To confirm or refute this hypothesis, future studies and clinical research are needed to clarify this issue.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient for publication of this case report and all accompanying images.
AUTHORS’ CONTRIBUTIONS
All authors contributed to the completion of this work. The final manuscript was read and approved by all authors
References
- Matias TB, Cordeiro RA, Duarte JA, et al. Immune-mediated hypertrophic pachymeningitis and its mimickers: magnetic resonance imaging findings. Acad Radiol 2023:S1076-6332(23)00034-X doi: 10.1016/j.acra.2023.01.017
- Kupersmith MJ, Martin V, Heller G, et al. Idiopathic hypertrophic pachymeningitis. Neurology 2004;62:686-94 doi: 10.1212/01.wnl.0000113748.53023.b7
- Abrantes FF, Moraes MP, Rezende Filho FM, et al. A clinical approach to hypertrophic pachymeningitis. Arquivos de Neuro-Psiquiatria. 2020 Dec 7;78:797-804.
- Dash GK, Thomas B, Nair M, et al. Clinico-radiological spectrum and outcome in idiopathic hypertrophic pachymeningitis. J Neurol Sci. 2015 Mar 15;350(1-2):51-60
- Yahyapour R, Amini P, Rezapour S, et al. Radiation-induced inflammation and autoimmune diseases. Mil Med Res 2018;5:9
- Giaj-Levra N, Sciascia S, Fiorentino A, et al. Radiotherapy in patients with connective tissue diseases. Lancet Oncol 2016;17:e109-e117
- Mekinian A, Maisonobe L, Boukari L, et al. Characteristics, outcome and treatments with cranial pachymeningitis: A multicenter French retrospective study of 60 patients. Medicine. 2018;97(30):e11413.
